Occipital lobe ppt
- 1. ANATOMY,FUNCTIONS AND EVALUATION OF OCCIPITAL LOBE Dr.SUMIT KAMBLE SENIOR RESIDENT DM NEUROLOGY GOVT. MEDICAL COLLEGE ,KOTA
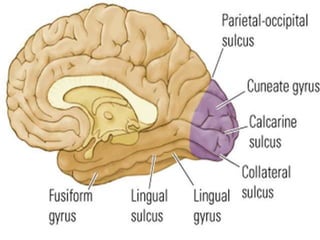
- 2. The two occipital lobes • Are the smallest of four paired lobes in the human cerebral cortex. • Separated from parietal lobe by: Parieto-occipital sulcus. • The OL 3 landmarks: • Calcrine fissure: Div. The upper and lower halves of the visual world. • Lingual Gyrus: • Fusiform Gyrus:
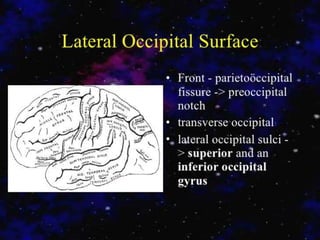
- 5. Four Lobes on the Lateral Surface OCCIPITAL LOBE The occipital lobe is separated from the parietal and temporal lobes by the line between the parieto- occipital sulcus and the preoccipital notch FRONTAL LOBE PARIETAL LOBE TEMPORAL LOBE Preocci pital Notch Parieto-occipital Sulcus
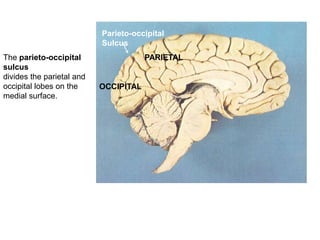
- 6. Parieto-occipital Sulcus OCCIPITAL PARIETALThe parieto-occipital sulcus divides the parietal and occipital lobes on the medial surface.
- 8. 1. V1 2. V2 3. V3 4. V3A 5. V4 6. V5 Primary Visual Cortex Secondary Visual Cortex
- 11. The occipital lobe • is the visual processing center of the mammalian brain containing most of the anatomical region of the visual cortex. • The primary visual cortex is Brodmann area 17, commonly called V1 (visual one). • Human V1 is located on the medial side of the occipital lobe within the calcarine sulcus; • the full extent of V1 often continues onto the posterior pole of the occipital lobe. V1 is often also called striate cortex because it can be identified by a large stripe of myelin, the Stria of Gennari.
- 12. Extrastriate regions • Visually driven regions outside V1 are called extrastriate cortex. • There are many extrastriate regions, and these are specialized for different visual tasks, such as visuospatial processing, color discrimination, and motion perception.
- 13. Connections of the Visual Cortex Connections -Primary Visual Cortex (V1) -Input from LGN -Output to all other levels -Secondary Visual Cortex (V2) Output to all other levels -After V2 •Output to the parietal lobe - Dorsal Stream •Output to the inferior temporal lobe - Ventral Stream •Output to the superior temporal sulcus (STS) - STS Stream • Dorsal Stream – Visual Guidance of Movements • Ventral Stream – Object Perception • STS – Visuospatial functions (bio movement
- 14. Connections V1- Largest area, called striate cortex. Receives the largest input from the LGN and projects to ALL other occipital regions. 1st processing level. V2 - Also projects to all other occipital areas. Segregates info from V1.
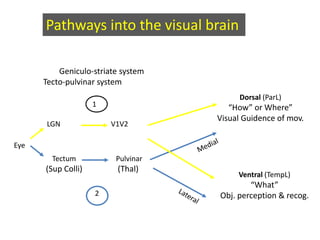
- 15. Pathways into the visual brain Geniculo-striate system Tecto-pulvinar system LGN V1V2 Ventral (TempL) “What” Obj. perception & recog. Tectum (Sup Colli) Pulvinar (Thal) 2 Dorsal (ParL) “How” or Where” Visual Guidence of mov. 1 Eye
- 16. Functions • A significant functional aspect of the occipital lobe is that it contains the primary visual cortex. • Retinal sensors convey stimuli through the optic tracts to the lateral geniculate bodies, where optic radiations continue to the visual cortex. • Each visual cortex receives raw sensory information from the outside half of the retina on the same side of the head and from the inside half of the retina on the other side of the head.
- 17. O.L Function V1 & V2 - function like mailboxes: segregating info to other areas., receives primary visual impressions Color/Form/Motion/Size and illumination. V3, V3A, V4, V5- Visual association areas- Recognition and identification of objects, storage of visual memories, it functions in more complex visual recognition and perception, revisualization, visual association and spatial orientation.
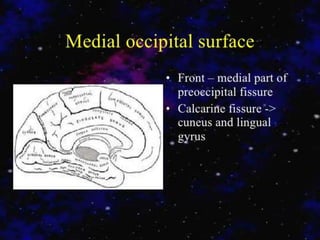
- 18. The primary visual cortex (Brodmann area 17 or, according to more recent nomenclature, V1) • is located almost entirely on the medial surface of the occipital lobe; just a small portion (perhaps 1 cm long) extends around the posterior pole onto the lateral surface. • The visual cortex also is called the striate cortex because a white myelinated fiber layer, the white stria of Gennari,is characteristic of this area. • The calcarine fissure extends from the parieto-occipital sulcus to the posterior pole, dividing the visual cortex into an upper portion (the cuneus gyrus) and a lower part (the lingual gyrus) most of the primary visual cortex is buried in the tissue within the calcarine fissure.
- 19. are two functions of the visual cortex, and such processing is a function of both its horizontal and its vertical organization. • The cells within the striate cortex are activated only by input from the LGN, although other cortical areas have input into the striate cortex. • The striate cortex communicates with the superior colliculus and the frontal eye fields. •Contour analysis and binocular vision
- 20. • Combines and analyzes the visual information relayed from the LGN and transmits this information to the higher visual association areas (the extrastriate cortex), which provide further interpretation. • These areas surround the striate cortex and are located on the lateral aspects of the occipital cortex. • Historically called Brodmann areas these areas now are known to contain several distinct cortical areas (designated V2, V3, V4, and V5)in which visual processing occurs.
- 21. Clinical Effects of Occipital Lobe Lesions • Visual Field Defects • Cortical blindness • Visual Anosognosia • Visual Illusions • Visual hallucinations • Visual Agnosias
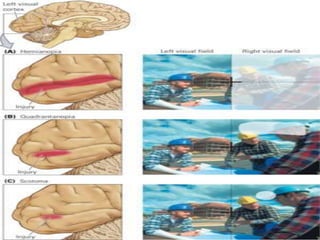
- 22. Visual field defects • The most familiar clinical abnormality resulting from a lesion of one occipital lobe, is a contralateral homonymous hemianopia,. • Extensive destruction abolishes all vision in the corresponding half of each visual field. • With a neoplastic lesion that eventually involves the entire striate region, the field defect may extend from the periphery toward the center, and loss of color vision (hemiachromatopsia) often precedes loss of black and white. • Destruction of only part of the striate cortex on one side yields characteristic field defects that accurately indicate the loci of the lesion.
- 24. Cortical Blindness • With bilateral lesions of the occipital lobes (destruction of area 17 of both hemispheres), there is a loss of sight that can be conceptualized as bilateral hemianopia. • The degree of blindness may be equivalent to that which follows severing of the optic nerves. • The pupillary light reflexes are preserved because they depend upon visual fibers that terminate in the midbrain, but reflex closure of the eyelids to threat or bright light may be preserved
- 25. • No changes are detectable in the retinas. • The eyes are still able to move through a full range and, if there is macular sparing as there usually is with vascular lesions, optokinetic nystagmus can be elicited • Visual imagination and visual imagery in dreams are preserved. • With rare exceptions, no cortical potentials can be evoked in the occipital lobes by light flashes or pattern changes (visual evoked response), and the alpha rhythm is lost in the electroencephalogram
- 26. Less-complete bilateral lesions • leave the patient with varying degrees of visual perception. • There may also be visual hallucinations of either elementary or complex types. • The mode of recovery from cortical blindness:There will be a regular progression from cortical blindness through visual agnosia and partially impaired perceptual function to recovery. • Even with recovery, the patient may complain of visual fatigue (asthenopia) and difficulties in fixation and fusion.
- 27. The usual cause of cortical blindness • is occlusion of the posterior cerebral arteries (most often embolic) or the equivalent, occlusion of the distal basilar artery. • Macular sparing may leave the patient with an island of barely serviceable central vision. • The infarct may also involve the mediotemporal regions or thalami, which share the posterior cerebral artery supply, with a resulting Korsakoff amnesic defect and a variety of other neurologic deficits referable to the high midbrain and diencephalon (drowsiness, akinetic mutism etc… )
- 28. Patients with bilateral occipital lobe damage • may have complete“cortical” blindness. • Some patients with cortical blindness are unaware that they cannot see, and some even confabulate visual descriptions or blame their poor vision on dim lighting or not having their glasses (Anton syndrome, originally described in 1899). • Patients with Anton syndrome may describe objects they “see” in the room around them but walk immediately into the wall.
- 29. Visual Anosognosia (Anton Syndrome ) • The main characteristic of this disorder is the denial of blindness by a patient who obviously cannot see. • The patient acts as though he could see, and in attempting to walk, collides with objects, even to the point of injury. • The lesions in cases of negation of blindness extend beyond the striate cortex to involve the visual association areas.
- 30. Visual Illusions (Metamorphopsias • These may present as distortions of form, size, movement, or color like deformation of the image, change in size, illusion of movement, or a combination of all three. • Illusions of these types have been reported with lesions confined to the occipital lobes but are more frequently caused by shared occipitoparietal or occipitotemporal lesions; • The right hemisphere appears to be involved more often than the left.
- 31. Illusions of movement • occur more frequently with posterior temporal lesions or seizures, polyopia (one object appearing as two or more objects) more frequently with occipital lesions (it also occurs in hysteria), and • palinopsia (perseveration of visual images, as in the frames of a celluloid film) with both posterior parietal and occipital lesions. • Visual field defects are present in many of the cases. • In all these conditions the anatomic correlates are imprecise.
- 32. Visual Hallucinations • These phenomena may be elementary or complex, and both types have sensory as well as cognitive aspects. • Elementary (or unformed) hallucinations include flashes of light, colors, luminous points, stars, multiple lights (like candles), and geometric forms (circles, squares, and hexagons). • They may be stationary or moving (zigzag, oscillations, vibrations, or pulsations). • Complex hallucinations include objects, persons, or animals and infrequently, more complete scenes that are indicative of lesions in the visual association areas or their connections with the temporal lobes.
- 33. Color vision defects • Two types of color vision deficit are associated with occipital lesions. • First, a complete loss of color vision, or achromatopsia, may occur either ipsilaterally or in one visual hemifield with lesions that involve portions of the visual association cortex (Brodmann areas 18 and 19). • Second, patients with pure alexia and lesions of the left occipital lobe fail to name colors, although their color matching and other aspects of color perception are normal.
- 34. • Patients often confabulate an incorrect color name when asked what color an object is. • This deficit can be called color agnosia, in the sense that a normally perceived color cannot be properly recognized. • Although this deficit has been termed color anomia, these patients can usually name the colors of familiar objects such as a school bus or the inside of a watermelon.
- 35. Balint Syndrome and Simultanagnosia • In 1909, Balint described a syndrome in which patients act blind, yet can describe small details of objects in central vision. • The disorder is usually associated with bilateral hemisphere lesions, often involving the parietal and frontal lobes.
- 36. Balint syndrome • involves a triad of deficits: (1) psychic paralysis of gaze, also called ocular motor apraxia, or difficulty directing the eyes away from central fixation; (2) optic ataxia, or incoordination of extremity movement under visual control (with normal coordination under proprioceptive control; and (3) impaired visual attention.
- 37. These deficits • result in the perception of only small details of a visual scene, with loss of the ability to scan and perceive the “big picture.” • Patients with Balint syndrome literally cannot see the forest for the trees. • Some but not all patients have bilateral visual field deficits.
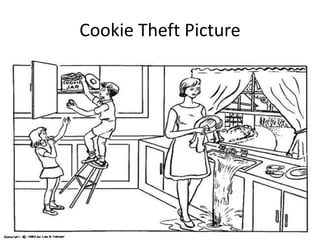
- 38. Simultanagnosia • To establish the presence of simultanagnosic symptoms, patients are asked to describe complex visual displays, such as the commonly used “Boston Cookie Theft” picture, which is a component of the Boston Diagnostic Aphasia Examination. • In the picture, the sink in the kitchen is overflowing as a boy and his sister attempt to steal cookies from the cookie jar without their mother noticing.
- 40. Patients take • a clearly piecemeal approach to interpreting the scene by reporting isolated items from the image. For instance, a patient may report seeing a “boy,” “stool,” and a “woman.” • However, when asked to interpret the overall meaning of the picture, the patient fails to comprehend the global whole. • Another picture used to assess visual impairments of patients with simultanagnosia is the “Telegraph Boy” picture. • Upon examination of higher nervous system functions, patients display no general intellectual impairments.
- 41. Telegraph Boy
- 42. In bedside neurological examination • helpful tests include asking the patient to interpret a complex drawing or photograph, such as the “Cookie Theft” picture from the Boston Diagnostic Aphasia Examination and the National Institutes of Health Stroke Scale.
- 43. Partial deficits • related to Balint syndrome have also been described, including isolated optic ataxia, or impaired visually guided reaching toward an object. • Optic ataxia likely results from disruption of the transmission of visual information for visual direction of motor acts from the occipital cortex to the premotor areas. • This function involves portions of the dorsal occipital and parietal areas as part of the “dorsal visual Stream”
- 44. A second partial Balint syndrome • deficit is simultanagnosia, or loss of ability to perceive more than one item at a time, first described by Wolpert in 1924. • The patient sees details of pictures, but not the whole. • Many such patients have left occipital lesions and associated pure alexia without agraphia; these patients can often read “letter-by-letter,” or one letter at a time, but they cannot recognize a word at a glance
- 47. Visual Object Agnosia • Visual object agnosia is the quintessential visual agnosia: the patient fails to recognize objects by sight, with preserved ability to recognize them through touch or hearing in the absence of impaired primary visual perception or dementia • In 1890, Lissauer distinguished two subtypes of visual object agnosia: apperceptive visual object agnosia, referring to the synthesis of elementary perceptual elements into a unified image, and associative visual object agnosia, in which the meaning of a perceived stimulus is appreciated by recall of previous visual experiences.
- 48. Apperceptive Visual Agnosia • The first type, apperceptive visual agnosia, is difficult to separate from impaired perception or partial cortical blindness. • Any failure of object recognition in which relatively basic visual functions (acuity, color, motion) are preserved is apperceptive. • Patients with apperceptive visual agnosia can pick out features of an object correctly (e.g., lines, angles, colors, movement), but they fail to appreciate the whole object • Warrington and Rudge (1995) pointed to the right parietoccipital cortex for its importance in visual processing of objects, and they found this area critical to apperceptive visual agnosia.
- 49. • Apperceptive visual agnosia related to bilateral occipital lesions a “pseudoagnosic syndrome” associated with visual processing defects, as compared to true visual agnosias, in which the right parietal cortex is deficient in identifying and recognizing visual objects. • Recent evidence of the functions of specific cortical areas has included the specialization of the medial occipital cortex for appreciation of color and texture,whereas the lateral occipital cortex is more involved with shape perception. • Deficits in these specific visual functions can be seen in patients with visual object agnosia
- 50. • apperceptive visual agnosia usually occurs in patients with bilateral occipital lesions. • It may represent a stage in recovery from complete cortical blindness. • Deficits in recognition of visual objects may be especially apparent with recognition of degraded images, such as drawings rather than actual objects. • Apperceptive visual agnosia can also be part of dementing syndromes
- 51. Associative visual agnosia • It is defect in the association of the object with past experience and memory . The inability to recognize an object despite an apparent perception of the object is associative agnosia. • Some patients can copy or match drawings of objects they cannot name, thus excluding a primary defect of visual perception. • Aphasia is excluded because the patient can identify the same object presented in the tactile or auditory modality • occurs with bilateral occopitotemoral junction lessions.
- 52. prosopagnosia • Patients with facial agnosia cannot recognize any previously known faces, including their own as seen in a mirror or photograph. • First, patients who cannot match pictures of faces must have defective face processing,or apperceptive prosopagnosia, whereas those who can match faces but simply fail to recognize familiar examples(either friends and relatives or famous personages) have associative prosopagnosia
- 53. Benton Face Recognition • History: “facial agnosia”/ prosopagnosia • Purpose: Measures visualoperceptual discrimination of unfamiliar faces (not recognition/memory) • Associated with right hemisphere: parietal, occipitoparietal and occipitotemporal • 3 parts: – Match identical front view – Match front view with ¾ view – Match front view with various lighting conditions
- 54. In clinical studies • prosopagnosia may occur either as an isolated deficit or as part of a more general visual agnosia for objects and colors. Faces are likely the most complex and individualized visual displays to recognize, but some patients with visual object agnosia can recognize faces, suggesting that there may be a specific brain area devoted to facial recognition.
- 55. The anatomical localization of prosopagnosia • parallels that of the other visual agnosias. • Most studies have reported bilateral temporo- occipital lesions, often involving the fusiform or occipitotemporal gyri, but cases with unilateral posterior right hemisphere lesions have also been described. • Facial perception seems localized to the fusiform gyri, but recognition of familiar faces may require anterior temporal memory stores
- 56. The disconnection hypothesis • has been invoked in prosopagnosia, reflecting interruption of fibers passing from the occipital cortices to the centers where memories of faces are stored. • Prosopagnosia also occurs in dementing illnesses such as frontotemporal dementia and posterior cortical atrophy
- 57. Optic Aphasia • The syndrome of optic aphasia, or optic anomia, is intermediate • between agnosias and aphasias. • The patient with optic aphasia cannot name objects presented visually but can demonstrate recognition of the objects by pantomiming or describing their use. • The preserved recognition of the objects distinguishes optic aphasia from associative visual agnosia. • Like visual agnosics, patients with optic aphasia can name objects presented in the auditory or tactile modalities, distinguishingthem from anomic aphasics.
- 58. In optic aphasia • information about the object must reach parts of the cortex involved in recognition, perhaps in the right hemisphere, but the information is not available to the language cortex for naming. • Patients with optic aphasia may confabulate incorrect names when asked to name an object they clearly recognize,just as the patient with color agnosia confabulates incorrect color names.
- 59. • Visuospatial Agnosia • Among this variety of disorders of spatial perception and orientation, one disruptive form is topographical disorientation—the inability to find one’s way around familiar environments such as one’s neighborhood. • People with this deficit seem unable to recognize landmarks that would indicate the appropriate direction in which to travel • Most people with topographical disorientation have other visual deficits, especially defects in facial recognition. • Critical area for this disorder lies in the right medial occipitotemporal region, including the fusiform and lingual gyri.
- 60. Epilepsy and occipital lobes • Occipital lobe seizures are triggered by a flash, or a visual image that contains multiple colors. These are called flicker stimulation (usually through TV) these seizures are referred to as photo-sensitivity seizures. Patients having experienced occipital seizures described their seizure as seeing bright colors, and having severe blurred vision (vomiting was also apparent in some patients).
- 61. Occipital seizures • are triggered mainly during the day, through television, video games or any flicker stimulatory system. • Occipital seizures originate from an epileptic focus confined within the occipital lobes. They may be spontaneous or triggered by external visual stimuli. Occipital lobe epilepsies are etiologically idiopathic, symptomatic, or cryptogenic. • Symptomatic occipital seizures can start at any age, as well as any stage after or during the course of the underlying causative disorder. • Idiopathic occipital epilepsy usually starts in childhood. • Occipital epilepsies account for approximately 5% to 10% of all epilepsies.