Peptic ulcer
Download as PPTX, PDF28 likes10,919 views
This document discusses benign gastric and duodenal ulcers. It defines peptic ulcers as lesions in the stomach or duodenum mucosa. Gastric ulcers are caused by an imbalance of protective and damaging factors in the gastric mucosa. Duodenal ulcers are often caused by Helicobacter pylori infection or NSAID use. Medical management includes treating H. pylori infection, providing pain relief, and protecting the mucosa. Surgical procedures are indicated for complications like perforation or hemorrhage. Common procedures include vagotomy, drainage procedures like pyloroplasty, and resections like antrectomy or subtotal gastrectomy.
1 of 46
Downloaded 125 times

































Recommended
Perforated peptic ulcers



Perforated peptic ulcersSefeen Geris This document discusses perforated peptic ulcers. It first covers the surgical anatomy and blood supply of the stomach and duodenum. It then discusses the epidemiology, pathophysiology, risk factors, presentation, diagnosis, and treatment of perforated peptic ulcers. Key points include that perforations are more common in duodenal versus gastric ulcers and have a higher mortality rate for gastric ulcers. Risk factors include H. pylori infection, NSAID use, smoking, and Zollinger-Ellison syndrome. Patients typically present with sudden severe abdominal pain. Diagnosis involves upright chest x-rays showing free air. Treatment is surgical repair of the perforation.
Obstructive jaundice



Obstructive jaundicemostafa hegazy This document provides information about jaundice and obstruction of the biliary tract. It begins with an overview of the causes of yellow discoloration of the skin and mucous membranes, which is caused by bilirubin accumulation. It then describes the breakdown of red blood cells and how bilirubin is processed and excreted. The document outlines various causes of obstructive jaundice including gallstones, strictures, tumors, and external compression. Investigation methods and treatment approaches for different biliary obstructions are also summarized.
GASTRIC OUTLET OBSTRUCTION



GASTRIC OUTLET OBSTRUCTIONRakesh Minocha Gastric outlet obstruction is caused by benign or malignant diseases that obstruct gastric emptying. Common benign causes include peptic ulcer disease while pancreatic cancer is a frequent malignant cause. Patients experience nausea, vomiting and weight loss. Diagnosis involves distinguishing functional from mechanical causes and identifying the underlying etiology. Treatment focuses on rehydration and correcting metabolic abnormalities as well as addressing the mechanical obstruction through endoscopic or surgical interventions.
Stomach pathology



Stomach pathologyRawalpindi Medical College The key points are:
- Peptic ulcers are chronic, solitary ulcers that occur where the gastrointestinal tract is exposed to gastric acid and pepsin, most commonly the duodenum and stomach.
- Risk factors include H. pylori infection, NSAID use, smoking, stress, and family history.
- Common symptoms are epigastric pain, nausea, vomiting, bleeding.
- Treatment involves eradication of H. pylori, PPIs, histamine blockers, and sometimes surgery for complications.
Post gastrectomy syndrome 



Post gastrectomy syndrome Youttam Laudari Dumping syndrome occurs after gastric surgery when food empties too quickly from the stomach into the small intestine. It has early and late forms. Early dumping causes GI symptoms like nausea within 30 minutes and cardiovascular symptoms like palpitations. Late dumping 2-3 hours later can cause hypoglycemia. Treatment involves dietary changes and medications like octreotide. Other post-gastrectomy syndromes include afferent loop obstruction and vitamin deficiencies. Surgery may be needed to correct mechanical issues or revise reconstructions.
Acute Calculous Cholecystitis



Acute Calculous CholecystitisSun Yai-Cheng Acute calculous cholecystitis is caused by obstruction of the cystic duct by a gallstone. Symptoms include biliary colic, fever, and right upper quadrant pain. Ultrasound and hepatobiliary scintigraphy can diagnose thickened gallbladder walls and obstruction. Treatment involves early laparoscopic cholecystectomy for mild cases, or initial conservative treatment with antibiotics and potential percutaneous cholecystostomy for severe cases presenting with sepsis, with delayed cholecystectomy once the patient improves. Guidelines recommend early surgery for mild disease and initial medical management for severe acute cholecystitis.
Chronic Pancreatitis 



Chronic Pancreatitis Prudhvi Krishna This document provides an overview of chronic pancreatitis, including its pathophysiology, etiology, clinical features, diagnosis, and management. It discusses how chronic pancreatitis represents a continuous inflammatory and fibrosing process of the pancreas resulting in permanent dysfunction. The main causes are alcohol use and genetic factors. Patients present with abdominal pain in 95% of cases and can develop weight loss, steatorrhea, and diabetes. Diagnosis involves tests of pancreatic function and imaging tests looking for features like calcification. Treatment focuses on pain control, managing maldigestion with pancreatic enzyme replacement, and addressing complications like pseudocysts and stenosis.
Volvulus in git



Volvulus in gitairwave12 The document discusses different types of intestinal volvulus including gastric, small bowel, large bowel, and combinations. Gastric volvulus is classified as organoaxial or mesenteroaxial depending on the axis of rotation. Small bowel volvulus often occurs due to midgut malrotation. Large bowel volvulus commonly affects the cecum or sigmoid colon. Sigmoid volvulus is the most common type of large bowel volvulus and presents as an inverted U-shape on imaging. Cecal volvulus results from torsion of the cecum around its own mesentery.
Obstructive jaundice



Obstructive jaundiceSelvaraj Balasubramani Obstructive jaundice is one of the important surgical topics. In this playlist I have discussed the introduction, choledocholithiasis, Carcinoma Pancreas and biliary atresia. If you watch all these videos together you will become confident in Managing obstructive jaundice.
Acute and Chronic Cholecystitis



Acute and Chronic CholecystitisSujith Jose This document discusses acute and chronic cholecystitis. Acute cholecystitis typically occurs due to gallstone impaction and results in inflammation of the gallbladder. Common symptoms include fever, right upper quadrant pain, and nausea. Diagnosis involves physical exam findings like Murphy's sign along with supportive lab and ultrasound results showing gallstones, thickened gallbladder walls, and pericholecystic fluid. Treatment involves antibiotics, pain medication, and cholecystectomy usually within 3 days. Chronic cholecystitis is due to long-standing gallstones or cholecystoses and results in a thickened, non-functioning gallbladder. Cholecystectomy is the treatment for chronic cholecystitis.
Chronic pancreatitis



Chronic pancreatitisikramdr01 This document provides an overview of chronic pancreatitis, including its definition, epidemiology, pathology, classification, clinical features, diagnosis and treatment. Chronic pancreatitis is defined as permanent and irreversible damage to the pancreas resulting in inflammation, fibrosis and destruction of pancreatic tissue. It has an annual incidence of 3-9 cases per 100,000 people. Alcohol is a major risk factor. Diagnosis involves evaluating pancreatic function and structure through imaging, endoscopy and genetic/serological testing. Treatment focuses on pain management, pancreatic enzyme supplementation and surgery for severe cases.
Pancreatic pseudocyst



Pancreatic pseudocystdraakif This document summarizes information about pancreatic pseudocysts. It defines pancreatic pseudocysts as fluid collections contained by fibrous tissue that develop more than 4 weeks after acute or chronic pancreatitis. It describes the typical location, composition, and pathophysiology of pseudocysts. It also outlines the clinical presentation, diagnostic approach, natural history, potential complications, and treatment options for pancreatic pseudocysts, including percutaneous drainage, endoscopic drainage, and surgical drainage. The preferred intervention is typically endoscopic drainage given its less invasive nature, though surgery may be necessary for complicated or failed non-surgical cases.
Crohns disease



Crohns diseasesyed ubaid Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract. It is more common in western nations and presents most often in teens and twenties. While the exact cause is unknown, it involves a complex interplay of genetic and environmental factors. Common symptoms include abdominal pain, diarrhea, weight loss, and fever. Complications can include strictures, fistulas, abscesses, and small bowel obstruction. Diagnosis involves imaging tests like colonoscopy, capsule endoscopy, and CT scans to identify areas of inflammation and complications throughout the bowels.
Acute cholecystitis.pptx



Acute cholecystitis.pptxPradeep Pande The document provides tips for using a PowerPoint presentation on acute cholecystitis. It recommends:
1) Freely editing, modifying, and adding your name to slides.
2) Not worrying about number of slides, as half are blank except for titles.
3) Showing blank slides first to elicit student responses before presenting information.
4) Repeating this process of blank slide then information slide at the end for active learning.
5) Using this approach for self-study as well.
6) Checking notes for bibliography citations.
Management of acute pancreatitis



Management of acute pancreatitisBashir BnYunus This document provides an overview of the management of acute pancreatitis. It defines acute pancreatitis as the inflammation of the pancreas often associated with pancreatic duct dilation. It discusses the epidemiology, etiology, pathogenesis, clinical forms, investigations, risk assessment, treatment and prognosis of acute pancreatitis. The management involves resuscitation, assessing severity, treating any underlying causes, and monitoring for complications which can include pancreatic necrosis, infection and multi-organ failure. Severity is assessed using scoring systems like Ranson's criteria or CT severity index to determine prognosis and guide management.
Mallory weiss syndrome



Mallory weiss syndromeDaniel Augustine Mallory-Weiss syndrome and corrosive injury are caused by vomiting and corrosive ingestion respectively, leading to tears in the gastric mucosa or esophagus. GERD is caused by reflux of gastric acid into the esophagus due to incompetence of the lower esophageal sphincter, resulting in inflammation and ulcers. Hiatal hernia is a protrusion of the stomach through the esophageal hiatus that can cause reflux. Barret's esophagus is a complication of longstanding GERD where the esophageal mucosa is replaced by intestinal metaplasia, increasing the risk of esophageal adenocarcinoma.
Malrotation



MalrotationZahoor Khan This document summarizes malrotation of the gut, which occurs when normal rotation and fixation of the intestines fails to occur during fetal development. It describes the normal embryological process of gut rotation including the 270 degree counter-clockwise rotation of the midgut. Malrotation results in abnormal peritoneal bands that can cause bowel obstruction. Presentation is often bilious vomiting in infants, and diagnosis is made through imaging showing abnormal intestinal positioning. Treatment involves immediate surgery to reduce volvulus if present and lyse abnormal bands, with appendectomy also performed.
Gastro-oesophageal Reflux Disease by Anish Dhakal (Aryan)



Gastro-oesophageal Reflux Disease by Anish Dhakal (Aryan)Dr. Aryan (Anish Dhakal) GERD case scenario, introduction, investigations, lifestyle modifications, medical and surgical management including anti-reflux surgical modalities
Gastric outlet obstruction



Gastric outlet obstructionRajeshwar Kamineni This document provides an overview of gastric outlet obstruction (GOO). It discusses that GOO can result from benign or malignant causes that obstruct gastric emptying. The most common benign causes are peptic ulcer disease and gastric polyps, while pancreatic cancer is the most common malignant cause. Patients present with nausea, vomiting, weight loss, and dehydration. Diagnosis involves distinguishing mechanical from functional causes, and benign from malignant etiologies. Treatment depends on the underlying cause, with surgery considered for benign cases unresponsive to medical management or in select malignant cases for palliation.
Approach to chronic diarrhoea 



Approach to chronic diarrhoea Abhinav Srivastava This document discusses the evaluation and causes of chronic diarrhea. It begins by defining chronic diarrhea and outlining the normal stool production process. It then describes the main mechanisms that can cause diarrhea - osmotic, secretory, inflammatory, and dysmotility. Specific causes are discussed under each mechanism, including diseases, medications, toxins, and dietary factors. The document outlines the evaluation of a patient with chronic diarrhea, including history, physical exam, stool tests, imaging, and other lab tests. It provides guidance on testing for malabsorption and evaluating postsurgical causes of chronic diarrhea.
Chronic diarrhoea



Chronic diarrhoeaVarun Karri This document discusses chronic diarrhea, defining it as diarrhea lasting more than 4 weeks. It classifies chronic diarrhea based on factors such as duration, volume, pathophysiology, and stool characteristics. Common causes include infections, inflammatory bowel disease, irritable bowel syndrome, malabsorption issues, and medication side effects. A thorough history, physical exam, and laboratory testing can help identify the underlying cause and guide management, which may include dietary changes, medications, or further testing and procedures.
Abdiminal tuberculosis



Abdiminal tuberculosisThorlikonda Sasidhar 1. Abdominal tuberculosis refers to tuberculosis infection of the gastrointestinal tract, mesenteric lymph nodes, peritoneum, and organs like the liver and spleen.
2. It is commonly caused by Mycobacterium tuberculosis or M. bovis bacteria and spreads via ingestion, hematogenous spread, or lymphatic spread.
3. Common presentations include abdominal pain, fever, weight loss, and the formation of masses, strictures, or ascites in the abdomen. Investigations include imaging tests, blood tests, and microbiological analysis of samples.
Gall bladder & biliary tract anomalies and variants



Gall bladder & biliary tract anomalies and variantsSanal Kumar This document describes the normal anatomy of the gallbladder and biliary tract, as well as common anatomical variations and anomalies. It discusses the normal divisions and structures of the gallbladder and cystic duct. It then covers several anomalies including agenesis of the gallbladder, gallbladder duplication, wandering gallbladder, gallbladder torsion, and variations in gallbladder shape. The document also discusses ectopic locations of the gallbladder and variations in cystic duct insertion and bile duct anatomy.
PERI-AMPULLARY CARCINOMA



PERI-AMPULLARY CARCINOMADr. Shashank Agrawal All you need to know about peri-ampullary cancer
Periampullary cancer is a common diagnosis with patient with progressive jaundice in northern part of India
Timely diagnosis and proper treatment in a way towards cure
Obstructive jaundice



Obstructive jaundiceMohammedAlHinai18 The patient is a 65-year-old male with a history of chronic pancreatitis who presents with jaundice, weight loss, clay-colored stools, and itching. On examination, he appears jaundiced and emaciated with scratch marks and a palpable mass in the right upper abdomen. Imaging shows a mass in the head of the pancreas causing dilation of the pancreatic and bile ducts. Given the clinical findings and imaging results, pancreatic cancer is suspected. Biopsy of the mass confirms pancreatic adenocarcinoma. Surgical resection offers the only chance of cure but many patients have advanced disease at presentation.
Gastric outlet obstruction 



Gastric outlet obstruction Prakat Aryal The document discusses gastric outlet obstruction (GOO), which refers to any mechanical impediment to gastric emptying. It can be caused by benign or malignant conditions. Common benign causes include peptic ulcer disease and gastric polyps, while pancreatic cancer is a frequent malignant cause. Symptoms include vomiting, weight loss, and dehydration. Diagnosis involves imaging like barium studies and endoscopy. Treatment of GOO focuses on rehydration, nutritional support, and correcting electrolyte imbalances. Surgical intervention may be needed for persistent or malignant obstructions.
Gastric Cancer 09.



Gastric Cancer 09.Shaikhani. Gastric tumors can be benign or malignant. The most common malignant tumors are adenocarcinoma, lymphoma, and gastrointestinal stromal tumor (GIST). Risk factors for gastric cancer include H. pylori infection, diet, genetics, and conditions causing gastric atrophy. Early detection of gastric cancer improves survival rates. Treatment depends on the stage but may involve surgery, chemotherapy, and radiation therapy. Gastric lymphoma is usually non-Hodgkin's lymphoma and has a better prognosis than adenocarcinoma. GIST tumors originate in the stomach wall and can be benign or malignant depending on size and other characteristics.
Gall bladder disease



Gall bladder diseasePuneet Shukla Gallbladder disease is common, affecting around 5% of the population. Gallstones are the most common cause of gallbladder disease and occur more often in women, with increasing age. Symptoms include biliary colic, acute cholecystitis, and in rare cases gallbladder cancer. Treatment options include oral medication, lithotripsy for single stones, and cholecystectomy for symptomatic or complicated cases. Complications can include cholangitis, pancreatitis, and choledocholithiasis requiring ERCP.
Peptic ulcer



Peptic ulcerAniedu Ifeanyichukwu Peptic Ulcer Disease is caused by stomach acid and pepsin damaging the stomach or duodenal lining. Risk factors include H. pylori infection, smoking, NSAIDs, and age. The two main types are gastric and duodenal ulcers. Patients may experience abdominal pain or bleeding. Diagnosis involves endoscopy, biopsy, and breath testing. Treatment focuses on eradicating H. pylori, reducing acid with PPIs or H2 blockers, and surgery for complications. Lifestyle changes and multi-drug antibiotic regimens are effective at curing ulcers and preventing recurrence.
More Related Content
What's hot (20)
Obstructive jaundice



Obstructive jaundiceSelvaraj Balasubramani Obstructive jaundice is one of the important surgical topics. In this playlist I have discussed the introduction, choledocholithiasis, Carcinoma Pancreas and biliary atresia. If you watch all these videos together you will become confident in Managing obstructive jaundice.
Acute and Chronic Cholecystitis



Acute and Chronic CholecystitisSujith Jose This document discusses acute and chronic cholecystitis. Acute cholecystitis typically occurs due to gallstone impaction and results in inflammation of the gallbladder. Common symptoms include fever, right upper quadrant pain, and nausea. Diagnosis involves physical exam findings like Murphy's sign along with supportive lab and ultrasound results showing gallstones, thickened gallbladder walls, and pericholecystic fluid. Treatment involves antibiotics, pain medication, and cholecystectomy usually within 3 days. Chronic cholecystitis is due to long-standing gallstones or cholecystoses and results in a thickened, non-functioning gallbladder. Cholecystectomy is the treatment for chronic cholecystitis.
Chronic pancreatitis



Chronic pancreatitisikramdr01 This document provides an overview of chronic pancreatitis, including its definition, epidemiology, pathology, classification, clinical features, diagnosis and treatment. Chronic pancreatitis is defined as permanent and irreversible damage to the pancreas resulting in inflammation, fibrosis and destruction of pancreatic tissue. It has an annual incidence of 3-9 cases per 100,000 people. Alcohol is a major risk factor. Diagnosis involves evaluating pancreatic function and structure through imaging, endoscopy and genetic/serological testing. Treatment focuses on pain management, pancreatic enzyme supplementation and surgery for severe cases.
Pancreatic pseudocyst



Pancreatic pseudocystdraakif This document summarizes information about pancreatic pseudocysts. It defines pancreatic pseudocysts as fluid collections contained by fibrous tissue that develop more than 4 weeks after acute or chronic pancreatitis. It describes the typical location, composition, and pathophysiology of pseudocysts. It also outlines the clinical presentation, diagnostic approach, natural history, potential complications, and treatment options for pancreatic pseudocysts, including percutaneous drainage, endoscopic drainage, and surgical drainage. The preferred intervention is typically endoscopic drainage given its less invasive nature, though surgery may be necessary for complicated or failed non-surgical cases.
Crohns disease



Crohns diseasesyed ubaid Crohn's disease is a chronic inflammatory bowel disease that can affect any part of the gastrointestinal tract. It is more common in western nations and presents most often in teens and twenties. While the exact cause is unknown, it involves a complex interplay of genetic and environmental factors. Common symptoms include abdominal pain, diarrhea, weight loss, and fever. Complications can include strictures, fistulas, abscesses, and small bowel obstruction. Diagnosis involves imaging tests like colonoscopy, capsule endoscopy, and CT scans to identify areas of inflammation and complications throughout the bowels.
Acute cholecystitis.pptx



Acute cholecystitis.pptxPradeep Pande The document provides tips for using a PowerPoint presentation on acute cholecystitis. It recommends:
1) Freely editing, modifying, and adding your name to slides.
2) Not worrying about number of slides, as half are blank except for titles.
3) Showing blank slides first to elicit student responses before presenting information.
4) Repeating this process of blank slide then information slide at the end for active learning.
5) Using this approach for self-study as well.
6) Checking notes for bibliography citations.
Management of acute pancreatitis



Management of acute pancreatitisBashir BnYunus This document provides an overview of the management of acute pancreatitis. It defines acute pancreatitis as the inflammation of the pancreas often associated with pancreatic duct dilation. It discusses the epidemiology, etiology, pathogenesis, clinical forms, investigations, risk assessment, treatment and prognosis of acute pancreatitis. The management involves resuscitation, assessing severity, treating any underlying causes, and monitoring for complications which can include pancreatic necrosis, infection and multi-organ failure. Severity is assessed using scoring systems like Ranson's criteria or CT severity index to determine prognosis and guide management.
Mallory weiss syndrome



Mallory weiss syndromeDaniel Augustine Mallory-Weiss syndrome and corrosive injury are caused by vomiting and corrosive ingestion respectively, leading to tears in the gastric mucosa or esophagus. GERD is caused by reflux of gastric acid into the esophagus due to incompetence of the lower esophageal sphincter, resulting in inflammation and ulcers. Hiatal hernia is a protrusion of the stomach through the esophageal hiatus that can cause reflux. Barret's esophagus is a complication of longstanding GERD where the esophageal mucosa is replaced by intestinal metaplasia, increasing the risk of esophageal adenocarcinoma.
Malrotation



MalrotationZahoor Khan This document summarizes malrotation of the gut, which occurs when normal rotation and fixation of the intestines fails to occur during fetal development. It describes the normal embryological process of gut rotation including the 270 degree counter-clockwise rotation of the midgut. Malrotation results in abnormal peritoneal bands that can cause bowel obstruction. Presentation is often bilious vomiting in infants, and diagnosis is made through imaging showing abnormal intestinal positioning. Treatment involves immediate surgery to reduce volvulus if present and lyse abnormal bands, with appendectomy also performed.
Gastro-oesophageal Reflux Disease by Anish Dhakal (Aryan)



Gastro-oesophageal Reflux Disease by Anish Dhakal (Aryan)Dr. Aryan (Anish Dhakal) GERD case scenario, introduction, investigations, lifestyle modifications, medical and surgical management including anti-reflux surgical modalities
Gastric outlet obstruction



Gastric outlet obstructionRajeshwar Kamineni This document provides an overview of gastric outlet obstruction (GOO). It discusses that GOO can result from benign or malignant causes that obstruct gastric emptying. The most common benign causes are peptic ulcer disease and gastric polyps, while pancreatic cancer is the most common malignant cause. Patients present with nausea, vomiting, weight loss, and dehydration. Diagnosis involves distinguishing mechanical from functional causes, and benign from malignant etiologies. Treatment depends on the underlying cause, with surgery considered for benign cases unresponsive to medical management or in select malignant cases for palliation.
Approach to chronic diarrhoea 



Approach to chronic diarrhoea Abhinav Srivastava This document discusses the evaluation and causes of chronic diarrhea. It begins by defining chronic diarrhea and outlining the normal stool production process. It then describes the main mechanisms that can cause diarrhea - osmotic, secretory, inflammatory, and dysmotility. Specific causes are discussed under each mechanism, including diseases, medications, toxins, and dietary factors. The document outlines the evaluation of a patient with chronic diarrhea, including history, physical exam, stool tests, imaging, and other lab tests. It provides guidance on testing for malabsorption and evaluating postsurgical causes of chronic diarrhea.
Chronic diarrhoea



Chronic diarrhoeaVarun Karri This document discusses chronic diarrhea, defining it as diarrhea lasting more than 4 weeks. It classifies chronic diarrhea based on factors such as duration, volume, pathophysiology, and stool characteristics. Common causes include infections, inflammatory bowel disease, irritable bowel syndrome, malabsorption issues, and medication side effects. A thorough history, physical exam, and laboratory testing can help identify the underlying cause and guide management, which may include dietary changes, medications, or further testing and procedures.
Abdiminal tuberculosis



Abdiminal tuberculosisThorlikonda Sasidhar 1. Abdominal tuberculosis refers to tuberculosis infection of the gastrointestinal tract, mesenteric lymph nodes, peritoneum, and organs like the liver and spleen.
2. It is commonly caused by Mycobacterium tuberculosis or M. bovis bacteria and spreads via ingestion, hematogenous spread, or lymphatic spread.
3. Common presentations include abdominal pain, fever, weight loss, and the formation of masses, strictures, or ascites in the abdomen. Investigations include imaging tests, blood tests, and microbiological analysis of samples.
Gall bladder & biliary tract anomalies and variants



Gall bladder & biliary tract anomalies and variantsSanal Kumar This document describes the normal anatomy of the gallbladder and biliary tract, as well as common anatomical variations and anomalies. It discusses the normal divisions and structures of the gallbladder and cystic duct. It then covers several anomalies including agenesis of the gallbladder, gallbladder duplication, wandering gallbladder, gallbladder torsion, and variations in gallbladder shape. The document also discusses ectopic locations of the gallbladder and variations in cystic duct insertion and bile duct anatomy.
PERI-AMPULLARY CARCINOMA



PERI-AMPULLARY CARCINOMADr. Shashank Agrawal All you need to know about peri-ampullary cancer
Periampullary cancer is a common diagnosis with patient with progressive jaundice in northern part of India
Timely diagnosis and proper treatment in a way towards cure
Obstructive jaundice



Obstructive jaundiceMohammedAlHinai18 The patient is a 65-year-old male with a history of chronic pancreatitis who presents with jaundice, weight loss, clay-colored stools, and itching. On examination, he appears jaundiced and emaciated with scratch marks and a palpable mass in the right upper abdomen. Imaging shows a mass in the head of the pancreas causing dilation of the pancreatic and bile ducts. Given the clinical findings and imaging results, pancreatic cancer is suspected. Biopsy of the mass confirms pancreatic adenocarcinoma. Surgical resection offers the only chance of cure but many patients have advanced disease at presentation.
Gastric outlet obstruction 



Gastric outlet obstruction Prakat Aryal The document discusses gastric outlet obstruction (GOO), which refers to any mechanical impediment to gastric emptying. It can be caused by benign or malignant conditions. Common benign causes include peptic ulcer disease and gastric polyps, while pancreatic cancer is a frequent malignant cause. Symptoms include vomiting, weight loss, and dehydration. Diagnosis involves imaging like barium studies and endoscopy. Treatment of GOO focuses on rehydration, nutritional support, and correcting electrolyte imbalances. Surgical intervention may be needed for persistent or malignant obstructions.
Gastric Cancer 09.



Gastric Cancer 09.Shaikhani. Gastric tumors can be benign or malignant. The most common malignant tumors are adenocarcinoma, lymphoma, and gastrointestinal stromal tumor (GIST). Risk factors for gastric cancer include H. pylori infection, diet, genetics, and conditions causing gastric atrophy. Early detection of gastric cancer improves survival rates. Treatment depends on the stage but may involve surgery, chemotherapy, and radiation therapy. Gastric lymphoma is usually non-Hodgkin's lymphoma and has a better prognosis than adenocarcinoma. GIST tumors originate in the stomach wall and can be benign or malignant depending on size and other characteristics.
Gall bladder disease



Gall bladder diseasePuneet Shukla Gallbladder disease is common, affecting around 5% of the population. Gallstones are the most common cause of gallbladder disease and occur more often in women, with increasing age. Symptoms include biliary colic, acute cholecystitis, and in rare cases gallbladder cancer. Treatment options include oral medication, lithotripsy for single stones, and cholecystectomy for symptomatic or complicated cases. Complications can include cholangitis, pancreatitis, and choledocholithiasis requiring ERCP.
Similar to Peptic ulcer (20)
Peptic ulcer



Peptic ulcerAniedu Ifeanyichukwu Peptic Ulcer Disease is caused by stomach acid and pepsin damaging the stomach or duodenal lining. Risk factors include H. pylori infection, smoking, NSAIDs, and age. The two main types are gastric and duodenal ulcers. Patients may experience abdominal pain or bleeding. Diagnosis involves endoscopy, biopsy, and breath testing. Treatment focuses on eradicating H. pylori, reducing acid with PPIs or H2 blockers, and surgery for complications. Lifestyle changes and multi-drug antibiotic regimens are effective at curing ulcers and preventing recurrence.
pepticulcer-160130225146.pdf



pepticulcer-160130225146.pdfSatyanarayanRaigar Peptic Ulcer Disease is caused by stomach acid and pepsin damaging the stomach or duodenal lining. Risk factors include H. pylori infection, smoking, NSAIDs, and age. The two main types are gastric and duodenal ulcers. Patients may experience abdominal pain or bleeding. Diagnosis involves endoscopy, biopsy, and breath testing. Treatment focuses on eradicating H. pylori, reducing acid with PPIs or H2 blockers, and surgery for complications. Lifestyle changes and multi-drug antibiotic regimens are effective at curing ulcers and preventing recurrence.
Benigne Diseases Of Stomach...



Benigne Diseases Of Stomach...biswanath das Benigne diseases of stomach are one of the serious conditions of our world.... so here u get littlebit information about these diseases...hope it will help you for your future study about these diseases... thank you.
Veterinary gastrointestinal surgery



Veterinary gastrointestinal surgeryRekha Pathak this content is made by collection of photographs and literature from different sources about veterinary gastrointestinal surgery
PEPTIC ULCER.pptx



PEPTIC ULCER.pptxMelba Shaya Sweety PEPTIC ULCER
Pathophysiology
Nursing
Melba Sahaya Sweety
Chinna Chadayan
Comprehensive Nursing
Pediatric Nursing
Child Health Nursing
peptic ulcer mohammad abu sad 1.pptx



peptic ulcer mohammad abu sad 1.pptxMohamadAbusaad Peptic ulcer disease is caused by an imbalance between aggressive factors like H. pylori infection, NSAIDs, and acid that damage the stomach or duodenal lining, and defensive mucosal mechanisms. Common symptoms include abdominal pain and bleeding. Diagnosis involves endoscopy to visualize ulcers and test for H. pylori. Treatment includes lifestyle modifications, medications to reduce acid production like PPIs, eradicating H. pylori with antibiotic therapy, and sometimes surgery for complications. Managing risk factors can help prevent ulcers from recurring.
Peptic Ulcer Disease.pptx



Peptic Ulcer Disease.pptxMARIPOLTUCJANG Clinical Therapeutics
Discussion on the Pathophysiology down to Pharmacological Management of Peptic Ulcer Disease
Peptic Ulcer Disease.pptx



Peptic Ulcer Disease.pptxMARIPOLTUCJANG Peptic ulcer disease is defined as chronic ulcers that occur in portions of the gastrointestinal tract exposed to gastric acid and pepsin. Common causes include Helicobacter pylori infection and NSAID use.
The document discusses gastric anatomy and physiology related to acid secretion. It also covers the pathogenesis of peptic ulcers involving an imbalance between aggressive and defensive factors. Diagnostics include endoscopy to visualize ulcers and test for H. pylori.
Management involves acid suppression with PPIs or H2 blockers as well as cytoprotective agents. H. pylori infection is treated with antibiotic combinations. NSAID-induced ulcers are prevented or treated with PPIs or misopro
Peptic ulcer disease



Peptic ulcer diseaseKanchan Devi This document discusses peptic ulcer disease. It defines peptic ulcers as open sores that develop on the lining of the esophagus, stomach, or upper small intestine. The most common causes are Helicobacter pylori bacteria and NSAID use. Symptoms vary depending on the location of the ulcer but can include abdominal pain, nausea, vomiting, and bleeding. Diagnosis involves endoscopy or imaging tests. Treatment involves antibiotics, acid-reducers, or surgery if complications occur. Surgical procedures aim to reduce acid production or allow drainage around the ulcer.
Fwd: Bambury tutorial Upper GI Surgery



Fwd: Bambury tutorial Upper GI SurgeryJeku Jacob ---------- Forwarded message ----------
From: UCD Graduate '09 None <[email protected]>
Date: 2009/2/12
Subject: Bambury tutorial Upper GI Surgery
To: [email protected]
She does not know that we have this so please don't print it and bring it to
the lecture
3. 13 Mar 20 Acid Peptic Disease2 dt 13 mar 2020.pptx



3. 13 Mar 20 Acid Peptic Disease2 dt 13 mar 2020.pptxrenecorpuz1 GERD is caused by reflux of stomach contents into the esophagus. Symptoms include burning chest pain and difficulty swallowing. Investigations include endoscopy and pH monitoring. Treatment involves lifestyle changes, antacids, PPIs, and fundoplication surgery if other treatments are ineffective. Complications include esophagitis, Barrett's esophagus, and esophageal cancer. Hiatal hernia is a protrusion of the stomach through the diaphragm.
causing various symptoms Acute Gastritis.pptx



causing various symptoms Acute Gastritis.pptxssuser71aa7e causing various symptoms Acute Gastritis.pptx
dokumen.tips_veterinary-gastrointestinal-surgery.ppt



dokumen.tips_veterinary-gastrointestinal-surgery.pptsozanmuhamad1 This document discusses various gastrointestinal surgical procedures in veterinary medicine. It covers topics such as gastric and abomasal ulcers, gastric dilatation and torsion, gastric neoplasms, bloat, and rumen fistulation and rumenotomy. Diagnostic techniques including radiography, endoscopy, and ultrasound are mentioned. Surgical treatments including gastrectomy, pyloroplasty, and rumenostomy are summarized. The document provides an overview of common gastrointestinal surgical conditions and procedures in large animals.
SURGICAL COMPLICATIONS OF PUD md 5 july.pptx



SURGICAL COMPLICATIONS OF PUD md 5 july.pptxAmos Brighton This document outlines the anatomy, etiology, clinical features, diagnosis, and complications of peptic ulcer disease (PUD). It discusses the role of H. pylori infection and NSAID use in increasing aggressive factors and decreasing defensive factors in the stomach and duodenum, leading to ulcer formation. Common complications of PUD include bleeding, perforation, and gastric outlet obstruction. Surgical procedures for complications involve closure, excision, vagotomy, and reconstructive procedures depending on the location and type of ulcer. Recurrence can occur due to incomplete treatment of underlying causes.
Peptic ulcer disease (pud)



Peptic ulcer disease (pud)Jordan Mwelwa This presentation is to help readers to be equipped with knowledge on predisposing factor to peptic ulcer disease and how it can be managed in the clinical/hospital setup.
Recently uploaded (20)
Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...



Acute & Chronic Inflammation, Chemical mediators in Inflammation and Wound he...Ganapathi Vankudoth A complete information of Inflammation, it includes types of Inflammation, purpose of Inflammation, pathogenesis of acute inflammation, chemical mediators in inflammation, types of chronic inflammation, wound healing and Inflammation in skin repair, phases of wound healing, factors influencing wound healing and types of wound healing.
Digestive Powerhouses: Liver, Gallbladder, and Pancreas for Nursing Students



Digestive Powerhouses: Liver, Gallbladder, and Pancreas for Nursing StudentsViresh Mahajani This educational PowerPoint presentation is designed to equip GNM students with a solid understanding of the liver, pancreas, and gallbladder. It explores the anatomical structures, physiological processes, and clinical significance of these vital organs. Key topics include:
Liver functions: detoxification, metabolism, and bile synthesis.
Gallbladder: bile storage and release.
Pancreas: exocrine and endocrine functions, including digestive enzyme and hormone production. This presentation is ideal for GNM students seeking a clear and concise review of these important digestive system components."
Neurologic Manifestations of Infective Endocarditis.pptx



Neurologic Manifestations of Infective Endocarditis.pptxdribnibrahem164 neurological complications of infective endocarditis
Solubilization in Pharmaceutical Sciences: Concepts, Mechanisms & Enhancement...



Solubilization in Pharmaceutical Sciences: Concepts, Mechanisms & Enhancement...KHUSHAL CHAVAN This presentation provides an in-depth understanding of solubilization and its critical role in pharmaceutical formulations. It covers:
Definition & Mechanisms of Solubilization
Role of surfactants, micelles, and bile salts in drug solubility
Factors affecting solubilization (pH, polarity, particle size, temperature, etc.)
Methods to enhance drug solubility (Buffers, Co-solvents, Surfactants, Complexation, Solid Dispersions)
Advanced approaches (Polymorphism, Salt Formation, Co-crystallization, Prodrugs)
This resource is valuable for pharmaceutical scientists, formulation experts, regulatory professionals, and students interested in improving drug solubility and bioavailability.
DIAGNOSIS OF PREGNANCY PPT IN ALL TRIMESTER



DIAGNOSIS OF PREGNANCY PPT IN ALL TRIMESTERdaminipatel37 Diagnosis of all three trimester of pregnancy
TunesKit Spotify Converter Crack With Registration Code 2025 Free



TunesKit Spotify Converter Crack With Registration Code 2025 Freedfsdsfs386 TunesKit Spotify Converter is a software tool that allows users to convert and download Spotify music to various formats, such as MP3, AAC, FLAC, or WAV. It is particularly useful for Spotify users who want to keep their favorite tracks offline and have them in a more accessible format, especially if they wish to listen to them on devices that do not support the Spotify app.
https://shorturl.at/LDQ9c
Copy Above link & paste in New Tab
Dr. Jaymee Shell’s Perspective on COVID-19



Dr. Jaymee Shell’s Perspective on COVID-19Jaymee Shell Dr. Jaymee Shell views the COVID-19 pandemic as both a crisis that exposed weaknesses and an opportunity to build stronger systems. She emphasizes that the pandemic revealed critical healthcare inequities while demonstrating the power of collaboration and adaptability.
Shell highlights that organizations with gender-diverse executive teams are 25% more likely to experience above-average profitability, positioning diversity as a business necessity rather than just a moral imperative. She notes that the pandemic disproportionately affected women of color, with one in three women considering leaving or downshifting their careers.
To combat inequality, Shell recommends implementing flexible work policies, establishing clear metrics for diversity in leadership, creating structured virtual collaboration spaces, and developing comprehensive wellness programs. For healthcare providers specifically, she advocates for multilingual communication systems, mobile health units, telehealth services with alternatives for those lacking internet access, and cultural competency training.
Shell emphasizes the importance of mental health support through culturally appropriate resources, employee assistance programs, and regular check-ins. She calls for diverse leadership teams that reflect the communities they serve and community-centered care models that address social determinants of health.
In her words: "The COVID-19 pandemic didn't create healthcare inequalities – it illuminated them." She urges building systems that reach every community and provide dignified care to all.
Correlation of vitamin D level with prediabetes status_Dr Ahmed Al Montasir_f...



Correlation of vitamin D level with prediabetes status_Dr Ahmed Al Montasir_f...zilkerapurbo Correlation of vitamin D level with prediabetes status
Creatine’s Untold Story and How 30-Year-Old Lessons Can Shape the Future



Creatine’s Untold Story and How 30-Year-Old Lessons Can Shape the FutureSteve Jennings Creatine burst into the public consciousness in 1992 when an investigative reporter inside the Olympic Village in Barcelona caught wind of British athletes using a product called Ergomax C150. This led to an explosion of interest in – and questions about – the ingredient after high-profile British athletes won multiple gold medals.
I developed Ergomax C150, working closely with the late and great Dr. Roger Harris (1944 — 2024), and Prof. Erik Hultman (1925 — 2011), the pioneering scientists behind the landmark studies of creatine and athletic performance in the early 1990s.
Thirty years on, these are the slides I used at the Sports & Active Nutrition Summit 2025 to share the story, the lessons from that time, and how and why creatine will play a pivotal role in tomorrow’s high-growth active nutrition and healthspan categories.
PERSONALITY DEVELOPMENT & DEFENSE MECHANISMS.pptxPersonality and environment:...



PERSONALITY DEVELOPMENT & DEFENSE MECHANISMS.pptxPersonality and environment:...ABHAY INSTITUTION Personality theory is a collection of ideas that explain how a person's personality develops and how it affects their behavior. It also seeks to understand how people react to situations, and how their personality impacts their relationships.
Key aspects of personality theory
Personality traits: The characteristics that make up a person's personality.
Personality development: How a person's personality develops over time.
Personality disorders: How personality theories can be used to study personality disorders.
Personality and environment: How a person's personality is influenced by their environment.
Sudurpaschim logsewa aayog Medical Officer 8th Level Curriculum



Sudurpaschim logsewa aayog Medical Officer 8th Level CurriculumDr Ovels Sudurpaschim province psc ( lok sewa aayog) medical officer 8th level syllabus
The influence of birth companion in mother care and neonatal outcome



The influence of birth companion in mother care and neonatal outcomelksharma10797 this content related to birth companionship, role of birth companion in care of mother and neonatal
Neurologic Manifestations of Infective Endocarditis.pptx



Neurologic Manifestations of Infective Endocarditis.pptxMohamadAlhes Neurological complications of inflective endocarditis
Role of Artificial Intelligence in Clinical Microbiology.pptx



Role of Artificial Intelligence in Clinical Microbiology.pptxDr Punith Kumar Artificial Intelligence (AI) is revolutionizing clinical microbiology by enhancing diagnostic accuracy, automating workflows, and improving patient outcomes. This presentation explores the key applications of AI in microbial identification, antimicrobial resistance detection, and laboratory automation. Learn how machine learning, deep learning, and data-driven analytics are transforming the field, leading to faster and more efficient microbiological diagnostics. Whether you're a researcher, clinician, or healthcare professional, this presentation provides valuable insights into the future of AI in microbiology.
MORPHOLOGICAL FEATURES OF PNEUMONIA.....



MORPHOLOGICAL FEATURES OF PNEUMONIA.....maheenmazhar021 This presentation provides a detailed exploration of the morphological and microscopic features of pneumonia, covering its histopathology, classification, and clinical significance. Designed for medical students, pathologists, and healthcare professionals, this lecture differentiates bacterial vs. viral pneumonia, explains lobar, bronchopneumonia, and interstitial pneumonia, and discusses diagnostic imaging patterns.
💡 Key Topics Covered:
✅ Normal lung histology vs. pneumonia-affected lung
✅ Morphological changes in lobar, bronchopneumonia, and interstitial pneumonia
✅ Microscopic features: Fibroblastic plugs, alveolar septal thickening, inflammatory cell infiltration
✅ Stages of lobar pneumonia: Congestion, Red hepatization, Gray hepatization, Resolution
✅ Common causative pathogens (Streptococcus pneumoniae, Klebsiella pneumoniae, Mycoplasma, etc.)
✅ Clinical case study with diagnostic approach and differentials
🔬 Who Should Watch?
This is an essential resource for medical students, pathology trainees, and respiratory health professionals looking to enhance their understanding of pneumonia’s morphological aspects.
Research Hyopthesis and Research Assumption



Research Hyopthesis and Research AssumptionDr. Binu Babu Nursing Lectures Incredibly Easy Research Hyopthesis and Assumption
Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...



Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...PVI, PeerView Institute for Medical Education Co-Chairs, Robert M. Hughes, DO, and Christina Y. Weng, MD, MBA, prepared useful Practice Aids pertaining to retinal vein occlusion for this CME activity titled “Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Specialty Care.” For the full presentation, downloadable Practice Aids, and complete CME information, and to apply for credit, please visit us at https://bit.ly/3NyN81S. CME credit will be available until March 3, 2026.
Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...



Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...PVI, PeerView Institute for Medical Education
Peptic ulcer
- 1. Benign Gastric and Duodenal Ulcers Dr.Sujith Mathew Jose PG in General Surgery Coimbatore Medical College Coimbatore
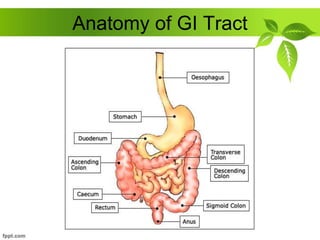
- 2. Anatomy of GI Tract
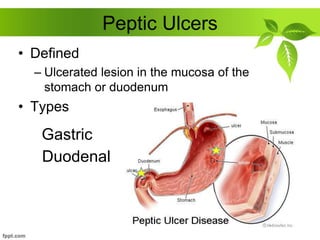
- 3. Peptic Ulcers • Defined – Ulcerated lesion in the mucosa of the stomach or duodenum • Types Gastric Duodenal
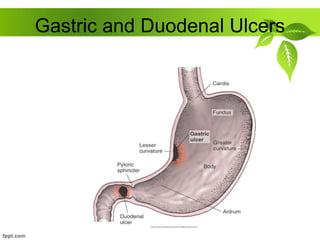
- 4. Gastric and Duodenal Ulcers
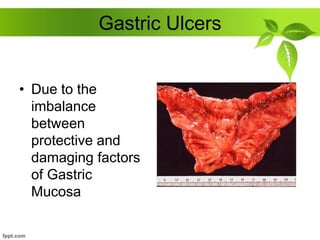
- 5. Gastric Ulcers • Due to the imbalance between protective and damaging factors of Gastric Mucosa
- 6. Stomach Defense Systems • Mucous layer – Coats and lines the stomach – First line of defense • Bicarbonate – Neutralizes acid • Prostaglandins – Hormone-like substances that keep blood vessels dilated for good blood flow – Thought to stimulate mucus and bicarbonate production
- 7. CAUSES of GASTRIC ULCER Atropic Gastritis Duodenogastric bile reflux Gastric Stasis Smoking NSAIDS Steroids HELICOBACTER PYLORI (70%) Lower Socioeconomic group
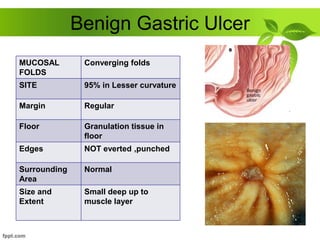
- 8. Benign Gastric Ulcer MUCOSAL FOLDS Converging folds SITE 95% in Lesser curvature Margin Regular Floor Granulation tissue in floor Edges NOT everted ,punched Surrounding Area Normal Size and Extent Small deep up to muscle layer
- 9. Malignant Gastric Ulcer MUCOSAL FOLDS Effacing Mucosal folds SITE Greater curvature Margin Irregular margin Floor Necrotic Slough in the floor Edges Everted Edges Surrounding Area Shows nodules, ulcers and irregularities Size and Extent Large and Deep
- 10. Types of Gastric Ulcer Type I in the andrum, near lesser curvature Type II Combined gastric and duodenal ulcer Type III Prepyloric Type IV Ulcer in the proximal stomach and Cardia 55% 25% 15% 5%
- 11. Gastric Ulcers • Pain occurs 1-2 hours after meals • Pain usually does not wake patient • Accentuated by ingestion of food • Risk for malignancy • Deep and penetrating and usually occur on the lesser curvature of the stomach
- 12. Gastric ulcer >3cm is called GIANT GASTRIC ULCER Gastric Ulcers is equal in both sexes affect older population less common than duodenal ulcers
- 13. Duodenal Ulcers Aetiology HELICOBACTER PYLORI (90%) NSAIDS, Steroids Zollinger Ellison Syndrome Alcohol, Smoking Blood Group O MEN 1 Chronic Pancreatitis
- 14. Duodenal Ulcers • Pain occurs 2-4 hours after meals • Pain wakes up patient • Pain relieved by food • Very little risk for malignancy
- 15. • Most Common in first part of duodenum • Chronic Ulcer penetrates the mucosa and into the muscle coat, leading to fibrosis • Fibrosis ------- Pyloric Stenosis
- 16. ANTERIOR ULCER ---- PERFORATE POSTERIOR ULCER ---- BLEEDS
- 17. GASTRIC ULCER erode LEFT GASTRIC VESSELS and SPLENIC VESSELS DUODENAL ULCER erodes GASTRODUODENAL artery
- 18. • Microscopically, Duodenal Ulcer shows, Destruction of Muscular Coat Base of ulcer with Granulation Tissue Arteries in the region shows ENDARTERITIS OBLITERANS
- 19. General Peptic Ulcer Symptoms PAIN Epigastric ---- Radiating to Back Periodicity Due to spontaneous Healing of ulcer Vomiting Present when stenosis occurs Weight Alteration Gastric loss Duodenal - > Gain Bleeding May present as anemia
- 20. Clinical Features GASTRIC ULCER DUODENAL ULCER Pain after food Intake Pain before food intake Periodicity less Common Periodicity more Common Weight loss +++ Weight Gain+++ Male = Female Male > Female Hemetemesis more Malena more
- 21. INVESTIGATIONS • Esophagogastrodeodenoscopy (EGD) • Upper gastrointestinal series (UGI) (Barium swallow) • Urea Breath Testing • USG
- 22. GASTRODUODENOSCOPY – Endoscopic procedure – Visualizes ulcer crater – Ability to take tissue biopsy to R/O cancer and diagnose H. pylori
- 23. It is fundamental that any gastric ulcer should be regarded as being Malignant, no matter how classically it resemble a benign gastric ulcer Multiple biopsies should be taken, as many as 10 well targeted biopsies
- 24. Biopsy can be taken to look for the presence of Helicobacter Pylori
- 25. Rapid Urease Test C13 or C14 breath test – Client drinks a carbon-enriched urea solution – Excreted carbon dioxide is then measured Faecal Antigen Test
- 26. BARIUM MEAL X Ray of Benign Gastric Ulcer • Outpouching of ulcer crater beyond the gastric contour (exoluminal)
- 27. HAMPTOMs LINE • Overhanging mucosa at the margins of a benign gastric ulcer, project inwards towards the ulcer HAMPTOMs LINE
- 28. • Regular/ Round Margin of the Ulcer Crater STOMACH SPOKE WHEEL PATTERN
- 29. • Converging mucosal folds towards the base of ulcer
- 30. Complications of Peptic Ulcers • Hemorrhage – Blood vessels damaged as ulcer erodes into the muscles of stomach or duodenal wall – Coffee ground vomitus or occult blood in tarry stools • Perforation – An ulcer can erode through the entire wall – Bacteria and partially digested fool spill into peritoneum=peritonitis • Narrowing and obstruction (pyloric) – Swelling and scarring can cause obstruction of food leaving stomach=repeated vomiting
- 31. Medical Management • Provide pain relief – Antacids and mucosa protectors • Eradicate H. pylori infection – Two antibiotics and one acid suppressor • Heal ulcer – Eradicate infection – Protect until ulcer heals • Prevent recurrence – Decrease high acid stimulating foods in susceptible people – Avoid use of potential ulcer causing drugs – Stop smoking AIM
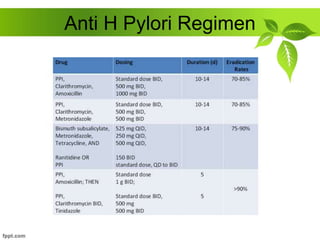
- 32. Anti H Pylori Regimen
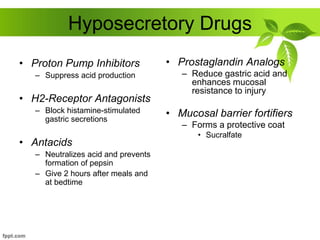
- 33. Hyposecretory Drugs • Proton Pump Inhibitors – Suppress acid production • H2-Receptor Antagonists – Block histamine-stimulated gastric secretions • Antacids – Neutralizes acid and prevents formation of pepsin – Give 2 hours after meals and at bedtime • Prostaglandin Analogs – Reduce gastric acid and enhances mucosal resistance to injury • Mucosal barrier fortifiers – Forms a protective coat • Sucralfate
- 34. Surgery • Greatly decreased from 1960 secondary to the discovery of H. pylori • Indication for Surgery – PERFORATION – OBSTRUCTION – HEMORRHAGE – NOT RESPONDING TO MEDICAL TREATMENT
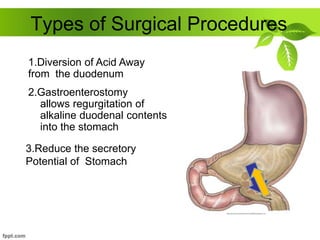
- 35. Types of Surgical Procedures 2.Gastroenterostomy allows regurgitation of alkaline duodenal contents into the stomach 1.Diversion of Acid Away from the duodenum 3.Reduce the secretory Potential of Stomach
- 36. Vagotomy Truncal Vagotomy – Section of the vagus nerve – Reduces the maximal acid output by app 50% Selective Vagotomy Highly Selective Vagotomy Fibres supplying the parietal cells are ligated Nerve of Latarjet which supplies andrum is retained So no drainage proceedure is required in HSV preserved Gastric branches are severed Hepatic branches are preserved
- 37. Drainage Procedures • Pyloroplasty It is a drainage procedure Longitudnal Sectioning of Pyloric Ring Incision is closed transversely
- 38. Gastrojejunostomy Alternative Drainage Procedure to Pyloroplasty Opening the lesser sac and performing anastomosis between the most dependent part of andrum and first jejunal loop.
- 39. Types of Surgical Procedures • Antrectomy – Lower half of stomach (antrum) makes most of the acid – Removing this portion (antrectomy) decreases acid production • Subtotal gastrectomy – Removes ½ to 2/3 of stomach • Remainder must be reattached to the rest of the bowel – Billroth I – Billroth II
- 40. Billroth I Gastrectomy Distal portion of the stomach is mobilised and resected The cut edge of the remnant is partially closed from Lesser Curvature aspect Stoma at greater curvature aspect Gastroduodenal anastomosis done
- 41. Billroth II Gastrectomy The lower portion of the stomach is removed and the remainder is anastomosed to the jejunum Duodenum is closed off by suture of staples High Operative Mortality and Morbidity
- 42. Sequelae of Peptic Ulcer Surgery • Recurrent Ulceration • Small Stomach Syndrome • Bile Vomiting • Early and Late Dumping • Post Vagotomy Diarrhoea • Malignant Transformation • Nutritional Consequences • Gall Stones
- 43. Dumping Syndrome EARLY DUMPING • Rapid emptying of hyperosmolar food and fluids from the stomach into the jejunum • Symptoms – Weakness – Faintness – Palpatations – Fullness – Discomfort – Nausea – diarrhea Rx Dietary manipulation Octreotide before meals Avoid High Carbohydrate Content
- 44. LATE DUMPING It is reactive hypoglycemia CHO load in small bowel ===> rise in blood glucose ===> Insulin levels to rise ===> Secondary Hypoglycemia
- 45. thankyou







