Viral host interactions
- 1. VIROLOGY PART iii VIRAL – HOST INTERACTIONS Dr.Riyaz Sheriff
- 2. Viral – host interactions • Cellular level • Individual level • Community level @ Cellular level • Cellular changes seen in tissue culture plate may not be seen in clinical infection Cell death Malignant transformation Cellular proliferation No effect
- 3. • Non structural proteins shut down the host protein & DNA synthesis • Large amount of Viral components change the cellular architecture of host cell • Toxic effects • Change in permeability of Host cell AUTOLYSIS • Formation of syncytium d/t fusion of adjacent cell membranes • Viral antigens will confer newer properties on host cell (cell adsorption, oncogenesis) • Changes in the host chromosome ( Measles, Mumps, Adenovirus, CMV & Varicella) • Inclusion bodies
- 4. Inclusion bodies • Structures with distinct size, shape , location and staining properties • Can be seen under light microscope after staining • May be seen in cytoplasm or nucleus • Generally acidophilic in nature – Pink in colour on staining with Giemsa or Eosin methylene blue stains • Some may be basophilic as well
- 5. Inclusion bodies • Helps in diagnosis – Negri bodies – intra cytoplasmic inclusion – Rabies – Guarnieri bodies – vaccinia – Bollinger bodies – fowl pox – Molluscum bodies – molluscum contagiosum – Cowdry type A – Herpes virus , Yellow fever virus – Cowdry type B – Adeno virus, Polio virus • Inclusion bodies my be an aggregate of virions or collection of viral antigens or the degenerative changes produced by viral infection.
- 6. Negri bodies – Rabies – Intracytoplasmic
- 7. Guarnieri bodies – vaccinia
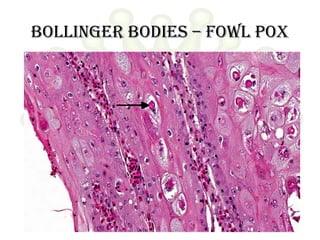
- 8. Bollinger bodies – fowl pox
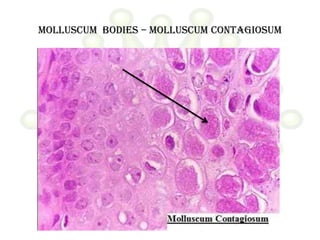
- 9. Molluscum bodies – molluscum contagiosum
- 10. Cowdry type A Hepatocyte with a large intranuclear inclusion body. Surrounded by a clear halo
- 11. Cowdry type b
- 12. Pathogenesis of viral infection • Inapparent • Apparent – Acute – Subacute – Chronic • Latent • Persistent tolerant infections : Congenital / Neonatal infections • Oncogenic virus • HIV
- 13. Route of entry • Respiratory tract (Most common) – Multiply locally Blood/Lymph Extensive multiplication Disease. – Small pox, chicken pox – Influenza , Rhinovirus (stay in respiratory tract itself) • Alimentary tract – All enveloped viruses are destroyed by bile – Rhinovirus is inactivated by gastric juice – Enterovirus, adenovirus, reo virus, hepatitis virus – Some multiply in GIT and transported to target organs (eg.Polio virus) • Genital tract • Conjunctiva • Skin • Vertical transmission – Mother to baby
- 14. Route of entry • Skin – Produce few local lesions – Papilloma, vaccinia, cowpox & molluscum contagiosum. – Viruses can enter through break in skin – Abrasions – Papiloma virus – Insect bites – Arbovirus – Animal bites – Rabies – Injections – Hepatitis • Genital tract – Human immuno deficiency virus
- 15. Route of entry • Conjunctiva – Local disease – Adenovirus – Systemic disease – Measles • Vertical transmission – Mother to baby – May occur at any stage till birth – Usally leads to fetal death and abortion – Maldevelopment – Rubella and Cytomegalovirus – Many tumor virus spread via this route
- 16. Spread of virus in the body • Studied by Fenner using mouse pox as a model
- 17. Mouse pox virus Enters through skin Local Multiplication Skin & Lymphatics Lymph Nodes Blood (Primary Viremia) Spleen , Liver (Central foci ) Extensive multiplication Spills into blood(Secondary Viremia) Clinical symptoms Virus reaches target organ Multiplication CLINICAL DISEASE
- 18. Incubation period • Time taken for virus to spread from site of entry to the organs of viral multiplication and causation of disease. • Localized diseases : Shorter incubation period • Systemic diseases : Longer incubation period • Incubation period shorter when directly introduced into blood stream
- 19. Host response Depends on 1. Virulence of the infecting strain 2. Resistance of the host » Immunological • Humoral • Cell mediated immunity » Non specific • Interferon production • Body temperature • Age • Malnutrition
- 20. • Viral infection liberates – Surface antigens – Internal antigens – Non structural antigens • Early proteins – Humoral immunity • IgG • IgM • IgA Mucosal surface Blood and Tissue
- 21. Immunoglobulins on viruses • Prevents attachment of virus to cell • Enhances viral degradation • Prevents release of virions from infected cell Immunoglobulin + Complement Surface damage of enveloped virions Cytolysis of virus infected cells
- 22. Role of antibodies • Role of antibodies in viral infection is limited • Antibody to internal antigen Non neutralizing • Antibody to surface antigen varying neutralization • Some antibodies can paradoxically increase infectivity • May contribute to Pathogenicity • Antibody may result in – Complement dependent cell injury – Immune complex type tissue injury
- 23. Role of cmi • Plays a major role in viral infection • Helps in recovery from viral infection • Can cause tissue damage as well • Deficient CMI increase in Herpes, Pox, Measles • Most often an infection provides long lasting immunity
- 24. Non immunological responses Macrophages phagocytose virus in blood. Body temperature : > 39°C inhibits most virus Exception – Herpes simplex – fever blisters Hormones : Corticosteroids enhance viral infection. Due to depression of immune system & inhibition of interferon synthesis Malnutrition Age
- 25. Interferons • Family of host coded proteins • No direct action on virus • Acts on host cells to make them refractory o viral infection. • On exposure to interferon cells produce TIP (Translation Inhibition Protein) inhibits translation of viral mRNA • Does not affect translation of host mRNA • Interferons are species specific. • RNA viruses are better inducers of interferon production • Temperature of > 40°C induces interferon secretion • Steroids and increased O2 tension decrease interferon synthesis • Synthesis starts in about 30mins of induction and reaches peak by 6-12 hours.
- 26. Interferons • α leucocytes • ß fibroblasts • Ɣ T-Lymphocytes • Inactivated by proteolytic enzymes • Resist 56°C – 60°C for 30-60mins • α & ß are resistant at pH range of 2-10 • Ɣ is labile at pH of 2 • Non toxic • Poorly antigenic • Cannot be estimated by routine serological methods
- 27. Use of Interferons • Ideal candidate for prophylaxis and treatment – Non toxic – Non antigenic – Diffuses freely in the body – Wide spectrum of antiviral activity • Drawback species specific • Current use URTI, Warts, Herpetic keratitis & anticancer agent in lymphomas
- 28. Biological effects of interferons • Anti-Viral : resistance to infection • Anti –Microbial: Resistance to intracellular infections (Toxoplasma, Chlamydia, Malaria) • Cellular effects : Inhibition of cell growth and proliferation, Increased expression of MHC antigens on cell surface • Immunoregulatory : – Increases activity of Natural killer (NK) calls and T cells. – Activates cell destruction activity of macrophage – Moderates antibody formation – Activates suppressor T cells – Suppresses DTH
- 29. Lab diagnosis • Microscopy : Demonstration of virus by electron microscopy Demonstration of inclusion bodies Fluorescent antibody techniques • Demonstration of viral antigen: Possible when viral antigens are abundant in the lesion Precipitation in gel Immunofluorescence CIE RIA ELISA PCR
- 30. Lab diagnosis • Isolation of virus : • Need proper transport media at appropriate temperature • Processing to remove bacterial contaminants • Inoculation in eggs • Animal inoculation • Tissue culture • Virus isolation has to be correlated with clinical history Identified by Neutralization tests
- 31. Lab diagnosis • Serological diagnosis : • Rise in titre of antibodies during course of disease • Examine paired sera – Acute – Convalescent (10-14 days later ) • When IgM alone is tested Single sample is enough – Neutralization test – Complement fixation – ELISA – Hemagglutination Inhibition
- 32. Immunoprophylaxis • Infection / vaccine Prolonged and effective immunity • Live vaccines more effective than killed vaccines • Successful Live vaccines – Small pox vaccine – Yellow fever vaccine – Polio Vaccine ( Sabin) • Killed vaccines prepared by inactivating viruses using Heat, Phenol, Formalin or BPL • Subunit vaccines – Hepatitis B
- 33. Live attenuated vaccines Advantages • Single dose • Administered by route of natural infection • Induce immunoglobulins • Induce CMI • Long lasting immunity • Economical • Apt for mass immunizations Disadvantages • Remote chance of reactivation of virus • Cannot be used in immunocompramised • Existence of other viruses may result in lessened immune response • Needs proper cold chain Killed vaccines • Safe • Stable • Can be given as combined vaccines • Multiple doses • Does not induce local immunity or cell mediated immunity
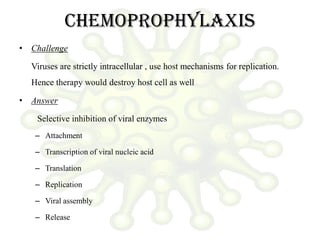
- 34. Chemoprophylaxis • Challenge Viruses are strictly intracellular , use host mechanisms for replication. Hence therapy would destroy host cell as well • Answer Selective inhibition of viral enzymes – Attachment – Transcription of viral nucleic acid – Translation – Replication – Viral assembly – Release
- 35. Antiviral agents • 1960 : First antiviral – Pox virus : Small pox eradicated by vaccination • 1962 : Idoxyuridine : Herpes Keratitis • 1970 : Acyclovir : effective in Herpes • Nucleoside analogues – Deoxyuridines • Idoxyuridine Herpetic keraitis • Trifluridine Less toxic • Bromovinyldeoxyuridine Herpes & Varicella – Adenine arabinoside • Herpetic keratitis • Herpes simplex • VZV – Acyclovir herpes – Ganciclovir Cytomegalovirus – Zidovudine HIV : inhibits viral reverse transcriptase
- 36. • Protease inhibitors – Saquinavir – Ritonovir – Indinavir • Others – Amantidine – blocks cell penetration by influenza A but not by B&C Antiviral agents