Hypertensive Retinopathy
- 2. HYPERTENSIVE RETINOPATHY BY: Sana Saleem
- 3. Hypertensive Retinopathy Definition Introduction Prevalence Symptoms Pathophysiology Diagnostic techniques and signs Associated conditions Management
- 4. Hypertensive Retinopathy Hypertensive retinopathy is damage to the retina caused by high blood pressure. Hypertensive retinopathy is retinal vascular damage caused by hypertension. Hypertensive retinopathy is a condition characterized by a spectrum of retinal vascular signs in people with elevated blood pressure
- 5. Hypertensive Retinopathy - Introduction Bilateral Symmetrical Small blood vessel disease Caused by systemic hypertension Acute or chronic Systolic or diastolic
- 6. Hypertensive Retinopathy – History & Symptoms Possible history of systemic hypertension Systemic hypertension largely asymptomatic Hypertensive retinopathy largely asymptomatic The eye examination will often give the first clue of systemic hypertension
- 7. Hypertensive Retinopathy - Prevalence The second most common retinal vascular disease Systemic hypertension (>160/90mmHg) Malignant hypertension (240/140mmhg) 0.5-0.75% Hypertensive retinopathy 4-10%
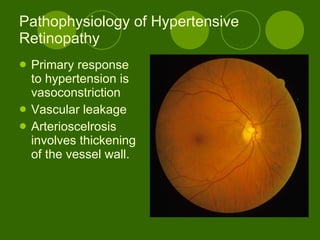
- 9. Pathophysiology of Hypertensive Retinopathy Primary response to hypertension is vasoconstriction Vascular leakage Arterioscelrosis involves thickening of the vessel wall.
- 10. Hypertensive Retinopathy – Pathophysiology A disease of the retinal microvasculature Cholesterol deposition in the tunica intima of medium and large arteries reduction in the lumen size of these vessels Arteriolosclerosis causes a breakdown in autoregulation the high pressures in the arterioles are transmitted to the retinal capillaries capillary closure or haemorrhage occurs
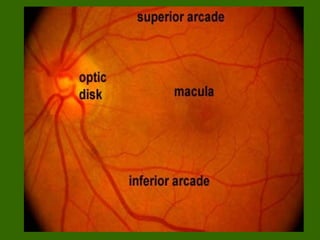
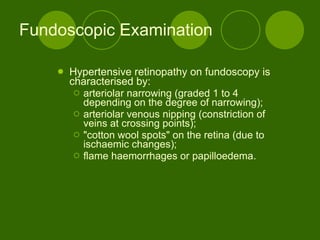
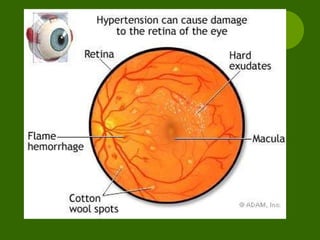
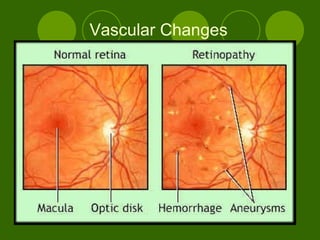
- 11. Fundoscopic Examination Hypertensive retinopathy on fundoscopy is characterised by: arteriolar narrowing (graded 1 to 4 depending on the degree of narrowing); arteriolar venous nipping (constriction of veins at crossing points); "cotton wool spots" on the retina (due to ischaemic changes); flame haemorrhages or papilloedema.
- 13. Vascular Changes
- 15. Hypertensive Retinopathy – Prevalence, Risk factors Afro-Caribbeans = relative risk factor 2x Age Family history Obesity Smoking Stress Alcohol consumption Lack of exercise
- 16. Hypertensive Retinopathy – Diagnostic Techniques & Signs Ophthalmoscopy (non-malignant retinopathy) Arteriosclerosis from chronic disease focal arteriolar narrowing arterio-venous crossing changes venous constriction and deflection distal banking arteriolar colour changes vessel sclerosis Similar signs with ageing Sphygmomanometry blood pressure measurement is required to make a positive diagnosis in the absence of malignant retinopathy changes
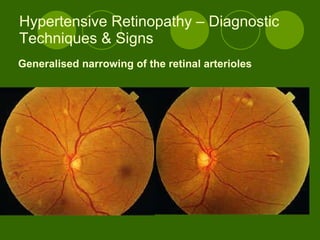
- 17. Hypertensive Retinopathy – Diagnostic Techniques & Signs Generalised narrowing of the retinal arterioles
- 18. Hypertensive Retinopathy – Diagnostic Techniques & Signs
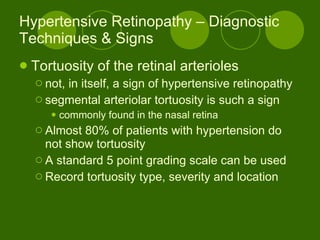
- 19. Hypertensive Retinopathy – Diagnostic Techniques & Signs Tortuosity of the retinal arterioles not, in itself, a sign of hypertensive retinopathy segmental arteriolar tortuosity is such a sign commonly found in the nasal retina Almost 80% of patients with hypertension do not show tortuosity A standard 5 point grading scale can be used Record tortuosity type, severity and location
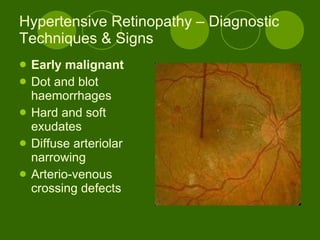
- 20. Hypertensive Retinopathy – Diagnostic Techniques & Signs Early malignant Dot and blot haemorrhages Hard and soft exudates Diffuse arteriolar narrowing Arterio-venous crossing defects
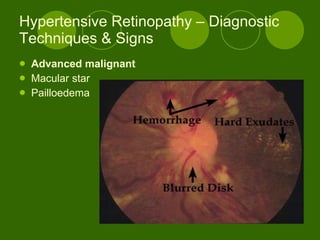
- 21. Hypertensive Retinopathy – Diagnostic Techniques & Signs Advanced malignant Macular star Pailloedema
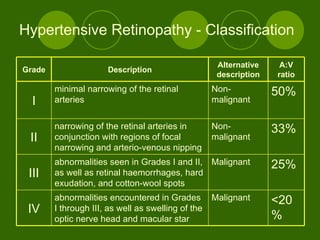
- 22. Hypertensive Retinopathy - Classification <20% Malignant abnormalities encountered in Grades I through III, as well as swelling of the optic nerve head and macular star IV 25% Malignant abnormalities seen in Grades I and II, as well as retinal haemorrhages, hard exudation, and cotton-wool spots III 33% Non-malignant narrowing of the retinal arteries in conjunction with regions of focal narrowing and arterio-venous nipping II 50% Non-malignant minimal narrowing of the retinal arteries I A:V ratio Alternative description Description Grade
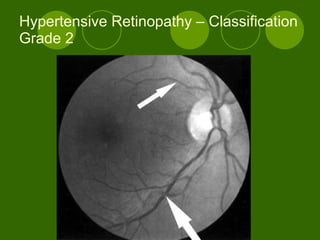
- 23. Hypertensive Retinopathy – Classification Grade 2
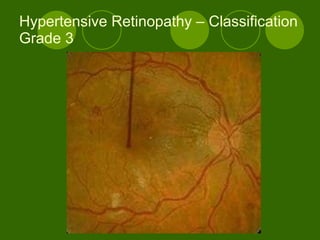
- 24. Hypertensive Retinopathy – Classification Grade 3
- 25. Hypertensive Retinopathy – Classification Grade 4
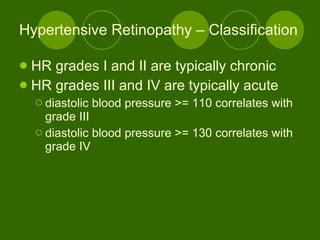
- 26. Hypertensive Retinopathy – Classification HR grades I and II are typically chronic HR grades III and IV are typically acute diastolic blood pressure >= 110 correlates with grade III diastolic blood pressure >= 130 correlates with grade IV
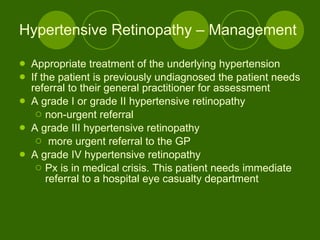
- 27. Hypertensive Retinopathy – Management Appropriate treatment of the underlying hypertension If the patient is previously undiagnosed the patient needs referral to their general practitioner for assessment A grade I or grade II hypertensive retinopathy non-urgent referral A grade III hypertensive retinopathy more urgent referral to the GP A grade IV hypertensive retinopathy Px is in medical crisis. This patient needs immediate referral to a hospital eye casualty department
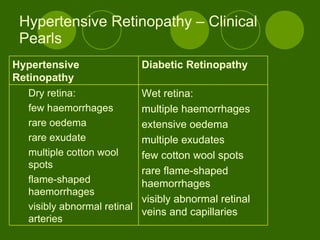
- 28. Hypertensive Retinopathy – Clinical Pearls Wet retina: multiple haemorrhages extensive oedema multiple exudates few cotton wool spots rare flame-shaped haemorrhages visibly abnormal retinal veins and capillaries Dry retina: few haemorrhages rare oedema rare exudate multiple cotton wool spots flame-shaped haemorrhages visibly abnormal retinal arteries Diabetic Retinopathy Hypertensive Retinopathy
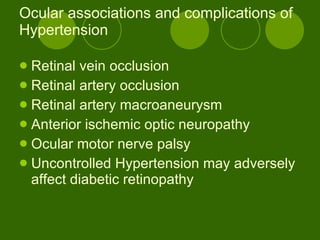
- 29. Ocular associations and complications of Hypertension Retinal vein occlusion Retinal artery occlusion Retinal artery macroaneurysm Anterior ischemic optic neuropathy Ocular motor nerve palsy Uncontrolled Hypertension may adversely affect diabetic retinopathy
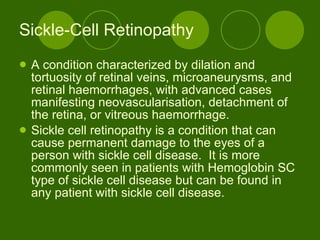
- 30. Sickle-Cell Retinopathy A condition characterized by dilation and tortuosity of retinal veins, microaneurysms, and retinal haemorrhages, with advanced cases manifesting neovascularisation, detachment of the retina, or vitreous haemorrhage. Sickle cell retinopathy is a condition that can cause permanent damage to the eyes of a person with sickle cell disease. It is more commonly seen in patients with Hemoglobin SC type of sickle cell disease but can be found in any patient with sickle cell disease.
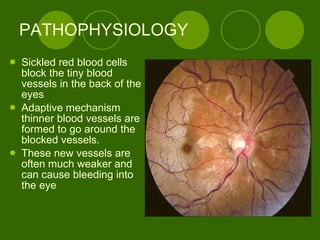
- 31. PATHOPHYSIOLOGY Sickled red blood cells block the tiny blood vessels in the back of the eyes Adaptive mechanism thinner blood vessels are formed to go around the blocked vessels. These new vessels are often much weaker and can cause bleeding into the eye
- 32. Symptoms What are the symptoms of sickle cell retinopathy? Usually there are no symptoms in the early stages Damage has already happened when vision problems occur.
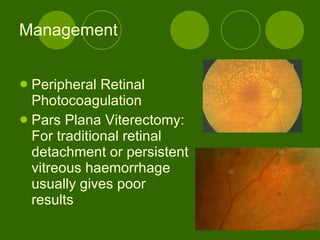
- 33. Management Peripheral Retinal Photocoagulation Pars Plana Viterectomy: For traditional retinal detachment or persistent vitreous haemorrhage usually gives poor results
- 34. Source Merck Source http://www.mercksource.com Merck Manual http://www.merck.com/mmpe/sec09/ch106/ch106f.html Clinical Ophthalmology -Kanski Medline Plus http://www.nlm.nih.gov/ The New England Journal Of Medicine http://content.nejm.org/cgi/content/short/351/22/2310 Eyeweb http:// www.eyeweb.org/hypertension.htm University of Maryland Medical Center http://www.umm.edu/ency/article/000999.htm