Burns- Modern Management
- 1. MODERN MANAGEMENT M M M C
- 2. Dr.B.SELVARAJ,MMSS;;MMcchh;;FFIICCSS;; Pediatric Surgeon Associate Professor Melaka Manipal Medical College Melaka; Malaysia M M M C
- 3. OBJECTIVES You should be able to • Identify types of Burns and their causes • Understand the pathophysiology of Burn injury • Describe the principles of managing a patient with Burns • Explain proper wound management techniques for treating Burns and Burn scars
- 4. Definition “ It is the response the of skin, mucous membrane and subcutaneous tissues to the thermal and few nonthermal injuries”
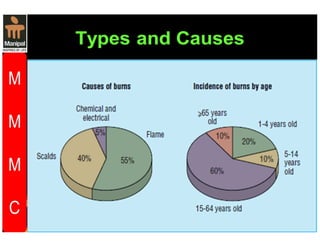
- 5. Types and Causes • Thermal injury - Scalds Spillage of hot liquids - Flame burns - Flash burns due to hot gases and combustible liquids - Contact burnscontact with hot metals • Electrical injury • Chemical injury acid alkali • Cold injury frostbite • Ionising radiation •
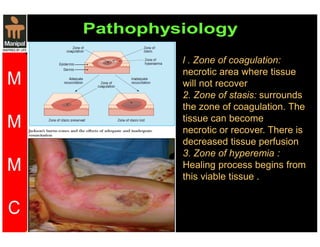
- 8. l . Zone of coagulation: necrotic area where tissue will not recover 2. Zone of stasis: surrounds the zone of coagulation. The tissue can become necrotic or recover. There is decreased tissue perfusion 3. Zone of hyperemia : Healing process begins from this viable tissue .
- 10. History • Find out the exact mechanism, including temperature of flame or water,duration of contact, concentration of chemical, voltage etc • Record factors suggesting inhalation injury, e.g. burns in a confined space,flash burns. • Enquire about other injuries. • Document first aid given so far. • Document timings of injury, first aid, and resuscitation
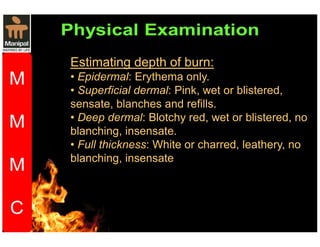
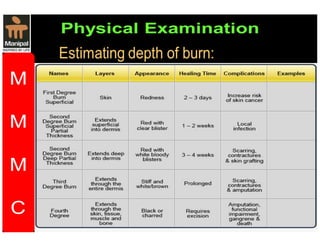
- 11. Estimating depth of burn: • Epidermal: Erythema only. • Superficial dermal: Pink, wet or blistered, sensate, blanches and refills. • Deep dermal: Blotchy red, wet or blistered, no blanching, insensate. • Full thickness: White or charred, leathery, no blanching, insensate
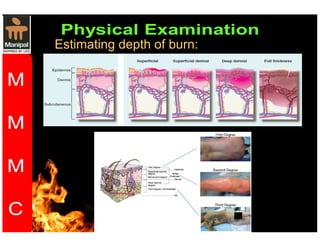
- 12. Estimating depth of burn:
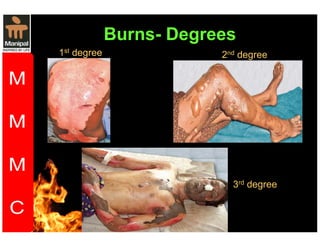
- 14. Burns- Degrees 1st degree 2nd degree 3rd degree
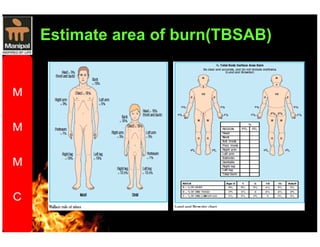
- 15. Physical Examination Estimate area of burn(TBSAB) Do not include areas of unblistered erythema. • Rule of nines • Rule of palm Patient’s hand is approximately 1% total body surface area (TBSA). • Lund and Browder chart is the most accurate method Fillup the chart
- 16. Estimate area of burn(TBSAB)
- 17. Signs of inhalation injury • Singed nasal hair. • Burns to face or oropharynx. Look for blistered palate. • Sooty sputum. • Drowsiness or confusion due to carbon monoxide inhalation. • Respiratory effort, breathlessness, stridor, or hoarseness are signs of impending airway obstruction and require immediate intubation
- 18. Burns- Initial management Immediate first aid • Stop the burning process (do not endanger yourself ). • Cool the wound. Douse with running water at 2–15*C for 20min (beware risk of hypothermia in infants, young children, and adults with 25% TBSA).
- 19. Resuscitation • A. Airway maintenance with C-spine control. Intubate if suspected inhalation injury; airway edema can be rapidly fatal. • B. Breathing and ventilation. • C. Circulation with haemorrhage control. • D. Disability and neurological status. • E. Exposure and environmental control. • F. Fluid resuscitation: child, 10% TBSA; adult, 15% TBSA burned.
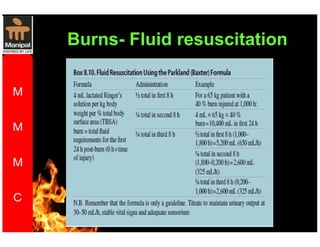
- 20. • Two large peripheral IV lines, preferably through unburned skin. • Send blood for FBC, UE, clotting, amylase, carboxyhaemoglobin. • Give 3–4mL Hartmann’s solution/kg/% TBSA burned. Half of this is given over the first 8h following injury, half over the next 16h. • Children need maintenance fl uid in addition. • Monitor resuscitation with urinary catheter (aim for urine output0.5–1mL/kg/h in adults and 1–1.5mL/kg/h in children). • Consider ECG, pulse, BP, respiratory rate, pulse oximetry, ABGs.
- 22. Management of burns wound • Superfi cial dermal burns will heal without scarring within 2 weeks as long as infection does not deepen the burn. • For small burns, outpatient treatment with simple, non-adherent dressings and twice weekly wound inspection is sufficient. • Wash burns with normal saline or chlorhexidine. • Debride large blisters. Elevate limbs to reduce pain and swelling. • Dress hands in plastic bags to allow mobilization
- 23. • Topical silver sulphadizine is used on deep burns to reduce risk of infection. • Escharotomy Performed for circumferential full thickness burns to the chest that limit ventilation or to the limbs that limit circulation. Patients may also need fasciotomies. • Excision and skin grafting Performed for deep dermal or full thickness burns that are too large to heal rapidly by secondary intention.
- 24. Criteria for referral to a burns unit • 15% TBSA burn in adult; 10% TBSA in child. • Burns to face, hands, feet, perineum, genitalia, major joints. • Full thickness burns 5% TBSA. • Electrical or chemical burns. • Associated inhalation injury—always intubate before transfer. • Circumferential burns of limbs or chest. • Burns in very young or old, pregnant women, and patients with significant comorbidities. • Any burn associated with major trauma.