Echo Mitral Regurg
- 1. Echocardiographic Evaluation of Mitral Regurgitation Vincent Brinkman, MD Cardiovascular Medicine The Ohio State University
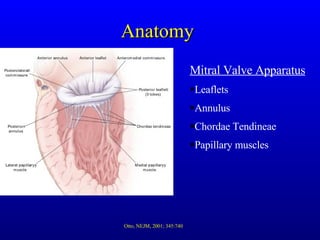
- 2. Anatomy Mitral Valve Apparatus Leaflets Annulus Chordae Tendineae Papillary muscles Otto, NEJM, 2001; 345:740
- 3. Etiology Leaflets Myxomatous (most common) Rheumatic disease Endocarditis Congential HOCM (SAM) Otto, NEJM, 2001; 345:740
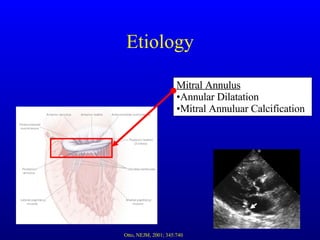
- 4. Etiology Mitral Annulus Annular Dilatation Mitral Annuluar Calcification Otto, NEJM, 2001; 345:740
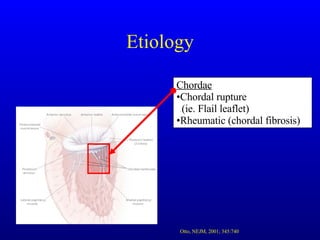
- 5. Etiology Chordae Chordal rupture (ie. Flail leaflet) Rheumatic (chordal fibrosis) Otto, NEJM, 2001; 345:740
- 6. Etiology Papillary Muscles Ischemia Infiltrative (amyloid, sarcoid) Congenital (malposition) Otto, NEJM, 2001; 345:740
- 7. Physiology Early Mitral Regurgitation Increased LV end diastolic pressure Increased LV contractility via increased preload Decreased or stable afterload due to filling of LA Preserved / hyperdynamic LV systolic function Bonow et al., JACC 2006; 48:e1
- 8. Physiology Chronic Compensated Regurgitation Dilatation of left ventricle with hypertrophy Dilated left atrium with normal pressures Normal to hyperdynamic LV function Chronic Decompensated Regurgitation Enlarged LV chamber and decline of LV function
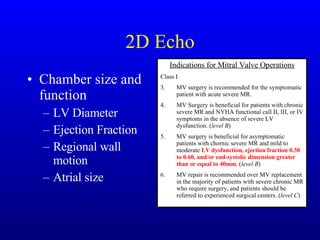
- 9. Treatment Surgical indications With symptoms Without symptoms LV parameters Atrial fibrillation Pulmonary HTN Rest/stress Flail Leaflet Ease of repair Stress ECHO Indications for Mitral Valve Operations Class I MV surgery is recommended for the symptomatic patient with acute severe MR. MV Surgery is beneficial for patients with chronic severe MR and NYHA functional call II, III, or IV symptoms in the absence of severe LV dysfunction. ( level B ) MV surgery is beneficial for asymptomatic patients with chornic severe MR and mild to moderate LV dysfunction, ejection fraction 0.30 to 0.60, and/or end-systolic dimension greater than or equal to 40mm. ( level B ) MV repair is recommended over MV replacement in the majority of patients with severe chronic MR who require surgery, and patients should be referred to experienced surgical centers. ( level C ) Class IIa MV repair is reasonable in experienced surgcial centers for asymptomatic patients with chronic severe MR with preserved LV function ( EF > 0.6 and ESLVD <40mm) in whom the likelihood of successful repair is > 90% ( level B ) MV surgery is reasonable for asymptomatic patients with chronic severe MR, preserved LV function, and new onset AF ( level C ) MV Surgery is reasonable for asymptomatic patients with chronic severe MR, preserved LV function, and pulmonary hypertensino (PASP > 50mmHG at rest or > 60mmHG with exercise). ( level C ) MV Surgery is reasonable for patients with chronic severe MR due to a primary abnormality of the mitral apparatus and NYHA functional call III-IV symptoms and severe LV dysfunction (EF < 0.30) in whom MV repair is highly likely. ( level C ) Class IIb MV repair may be considered for patients with chornic severe secondary MR due to severe LV dysfunction who have NYHA functional lass III-IV symptoms despite optimal medical therapy, including bi-v pacing. ( level C ) Class III MV surgery is not indicated for asymptomatic patients with MR and preserved LV function in whom significant doubt about the feasibility of repair exists. ( level C ) Isolated MV surgery is not indicated for patients with mild to moderate MR> ( level C ). Bonow et al., JACC 2006; 48:e1
- 10. Repair vs. Replacement Repair Mitral valve prolapse Annular dilatation Some rheumatic cases Replacement Severe endocarditis Severe calcification Chordal disruption
- 11. Echo Indications Indications for Transthoracic Echocardiography Class I 1. Transthoracic echocardiography is indicated for baseline evaluation of LV size and function, RV and left atrial size, pulmonary artery pressure, and severity of MR in any patient suspected of having MR. (Level C) 2. Transthoracic echocardiography is indicated for delineation of the mechanism of MR. (Level B) 3. Transthoracic echocardiography is indicated for annual or semiannual surveillance of LV function (estimated by ejection fraction and end systolic dimension) in asymptomatic patients with moderate to severe MR. (Level C) 4. Transthoracic echocardiography is indicated in patients with MR to evaluate the MV apparatus and LV function after a change in signs or symptoms. (Level C) 5. Transthoracic echocardiography is indicated to evaluate LV size and function and MV hemodynamics in the initial evaluation after MV replacement or MV repair. (Level C) Class IIa Exercise Doppler echocardiography is reasonable in asymptomatic patients with severe MR to assess exercise tolerance and the effects of exercise on pulmonary artery pressure and MR severity. (Level C) Class III Transthoracic echocardiography is not indicated for routine follow-up evaluation of asymptomatic patients with mild MR and normal LV size and systolic function. (Level C)
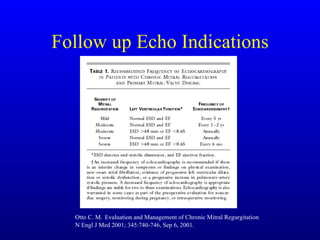
- 12. Follow up Echo Indications Otto C. M. Evaluation and Management of Chronic Mitral Regurgitation N Engl J Med 2001; 345:740-746, Sep 6, 2001.
- 13. The ECHO exam Quantify severity Establish the cause Evaluate LV function Evaluate associated findings Atrial Size Pulmonary pressures Etc.
- 14. 2D Echo Chamber size and function LV Diameter Ejection Fraction Regional wall motion Atrial size Indications for Mitral Valve Operations Class I MV surgery is recommended for the symptomatic patient with acute severe MR. MV Surgery is beneficial for patients with chronic severe MR and NYHA functional call II, III, or IV symptoms in the absence of severe LV dysfunction. ( level B ) MV surgery is beneficial for asymptomatic patients with chornic severe MR and mild to moderate LV dysfunction, ejection fraction 0.30 to 0.60, and/or end-systolic dimension greater than or equal to 40mm. ( level B ) MV repair is recommended over MV replacement in the majority of patients with severe chronic MR who require surgery, and patients should be referred to experienced surgical centers. ( level C )
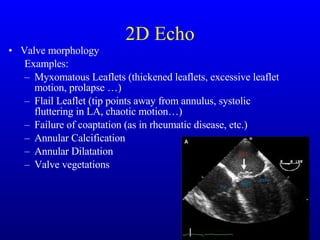
- 15. 2D Echo Valve morphology Examples: Myxomatous Leaflets (thickened leaflets, excessive leaflet motion, prolapse …) Flail Leaflet (tip points away from annulus, systolic fluttering in LA, chaotic motion…) Failure of coaptation (as in rheumatic disease, etc.) Annular Calcification Annular Dilatation Valve vegetations
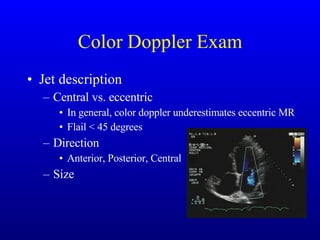
- 16. Color Doppler Exam Jet description Central vs. eccentric In general, color doppler underestimates eccentric MR Flail < 45 degrees Direction Anterior, Posterior, Central Size
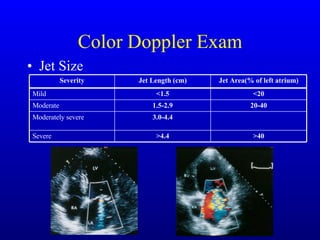
- 17. Color Doppler Exam Jet Size >40 >4.4 Severe 3.0-4.4 Moderately severe 20-40 1.5-2.9 Moderate <20 <1.5 Mild Jet Area(% of left atrium) Jet Length (cm) Severity
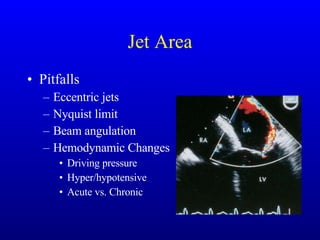
- 18. Jet Area Pitfalls Eccentric jets Nyquist limit Beam angulation Hemodynamic Changes Driving pressure Hyper/hypotensive Acute vs. Chronic
- 19. Vena Contracta Narrowest area of proximal jet. OK to use in central and eccentric jets Best measured in parasternal long view, but usually best seen in apical views Not apical 2 chamber view due to leaflet coaptation. Use narrow sector and zoom mode. Not affected by driving pressures / hemodynamics Vena Contracta <0.3cm = mild >0.6cm = severe
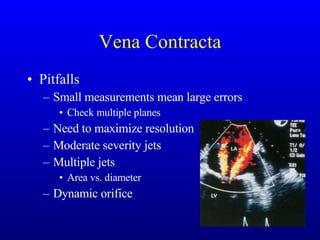
- 20. Vena Contracta Pitfalls Small measurements mean large errors Check multiple planes Need to maximize resolution Moderate severity jets Multiple jets Area vs. diameter Dynamic orifice
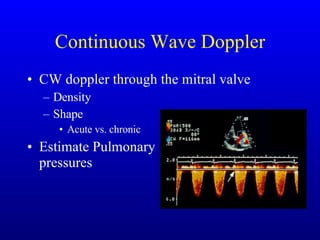
- 21. Continuous Wave Doppler CW doppler through the mitral valve Density Shape Acute vs. chronic Estimate Pulmonary pressures
- 22. Pulse Wave Doppler Mitral Inflow E vs. A wave predominance Pulmonary Vein Flow Normal Blunting Reversal
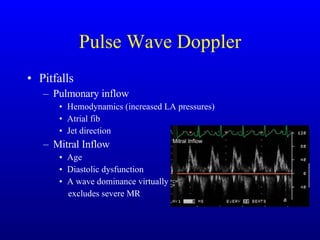
- 23. Pulse Wave Doppler Pitfalls Pulmonary inflow Hemodynamics (increased LA pressures) Atrial fib Jet direction Mitral Inflow Age Diastolic dysfunction A wave dominance virtually excludes severe MR
- 24. Quantifying MR Proximal Isovelocity Surface Area (PISA) Continuity equation, or volume in equals volume out Cross sectional area x velocity time integral = stroke volume With PISA, we use max velocities to determine the ERO: Proximal area x Proximal Velocity = Distal Area x Distal Velocity Distal Area = (Proximal Area x Proximal Velocity) / Distal Velocity
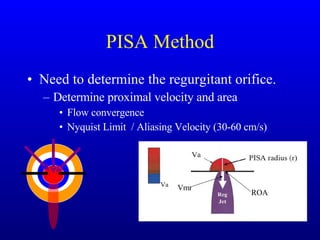
- 25. PISA Method Need to determine the regurgitant orifice. Determine proximal velocity and area Flow convergence Nyquist Limit / Aliasing Velocity (30-60 cm/s) Vmr ROA
- 26. PISA Method <0.2cm 2 = mild 0.2-0.29cm 2 = mod >0.4cm 2 = severe
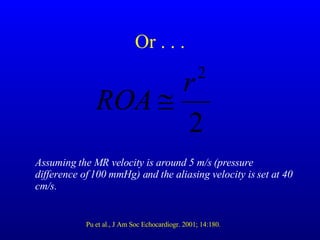
- 27. Or . . . Assuming the MR velocity is around 5 m/s (pressure difference of 100 mmHg) and the aliasing velocity is set at 40 cm/s. Pu et al., J Am Soc Echocardiogr. 2001; 14:180.
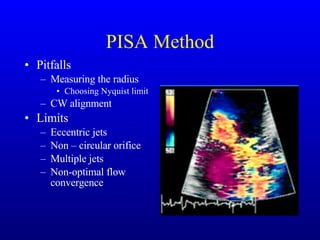
- 28. PISA Method Pitfalls Measuring the radius Choosing Nyquist limit CW alignment Limits Eccentric jets Non – circular orifice Multiple jets Non-optimal flow convergence
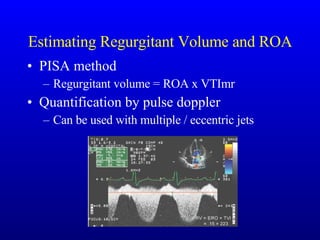
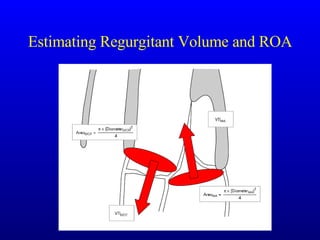
- 29. Estimating Regurgitant Volume and ROA PISA method Regurgitant volume = ROA x VTImr Quantification by pulse doppler Can be used with multiple / eccentric jets
- 30. Estimating Regurgitant Volume and ROA
- 31. Regurgitant Volume Regurgitant Volume Regurgitant Fraction
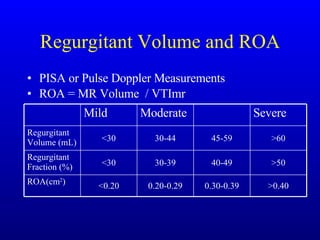
- 32. Regurgitant Volume and ROA PISA or Pulse Doppler Measurements ROA = MR Volume / VTImr >0.40 0.30-0.39 0.20-0.29 <0.20 ROA(cm 2 ) >50 40-49 30-39 <30 Regurgitant Fraction (%) >60 45-59 30-44 <30 Regurgitant Volume (mL) Severe Moderate Mild
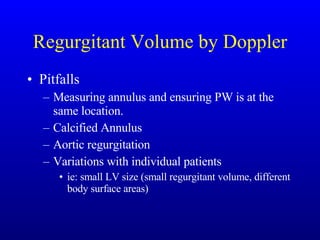
- 33. Regurgitant Volume by Doppler Pitfalls Measuring annulus and ensuring PW is at the same location. Calcified Annulus Aortic regurgitation Variations with individual patients ie: small LV size (small regurgitant volume, different body surface areas)
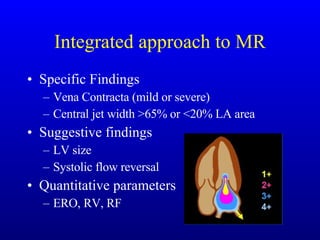
- 34. Integrated approach to MR Specific Findings Vena Contracta (mild or severe) Central jet width >65% or <20% LA area Suggestive findings LV size Systolic flow reversal Quantitative parameters ERO, RV, RF
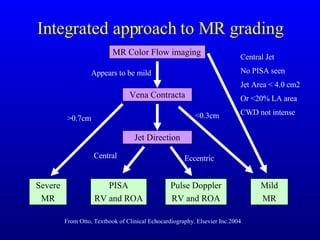
- 35. Integrated approach to MR grading MR Color Flow imaging Vena Contracta Jet Direction Severe MR PISA RV and ROA Pulse Doppler RV and ROA Mild MR From Otto, Textbook of Clinical Echocardiography. Elsevier Inc.2004 Appears to be mild >0.7cm <0.3cm Central Eccentric Central Jet No PISA seen Jet Area < 4.0 cm2 Or <20% LA area CWD not intense
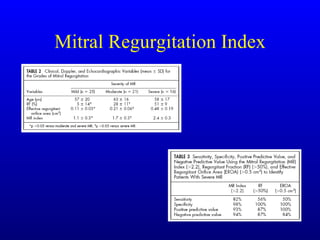
- 38. ROA and Outcomes
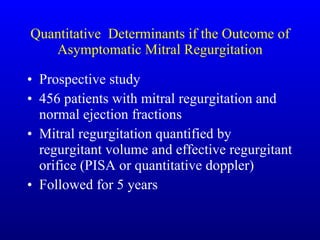
- 39. Quantitative Determinants if the Outcome of Asymptomatic Mitral Regurgitation Prospective study 456 patients with mitral regurgitation and normal ejection fractions Mitral regurgitation quantified by regurgitant volume and effective regurgitant orifice (PISA or quantitative doppler) Followed for 5 years
- 40. Quantitative Determinants if the Outcome of Asymptomatic Mitral Regurgitation Survival Death from cardiac cause
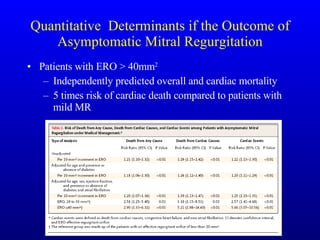
- 41. Quantitative Determinants if the Outcome of Asymptomatic Mitral Regurgitation Patients with ERO > 40mm 2 Independently predicted overall and cardiac mortality 5 times risk of cardiac death compared to patients with mild MR
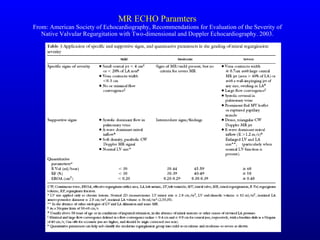
- 42. MR ECHO Paramters From: American Society of Echocardiography, Recommendations for Evaluation of the Severity of Native Valvular Regurgitation with Two-dimensional and Doppler Echocardiography. 2003.
- 43. MR ECHO Paramters From: American Society of Echocardiography, Recommendations for Evaluation of the Severity of Native Valvular Regurgitation with Two-dimensional and Doppler Echocardiography. 2003.
- 44. Paramater advantages and disadvantages
- 45. Other modalities TEE Intraoperative TEE 3D Echo Color m-mode