Female reproductive anatomy (1)
- 1. This information is important because it will raise your level of awareness and understanding about your physical body. It is imperative that you learn the changes you can expect to experience from menarche to menopause as you live with your female reproductive system 1 FEMALE REPRODUCTIVE ANATOMY
- 2. EXTERNAL GENTILIA • The vulva refers to those parts that are outwardly visible • The vulva includes: • Mons pubis • Labia majora • Labia minora • Clitoris • Urethral opening • Vaginal opening • Perineum • Individual differences in: • Size • Coloration • Shape • Of external gentalia are common 2
- 3. UNIT 3: FEMALE REPRODUCTIVE SYSTEM 3
- 4. MONS PUBIS • The triangular mound of fatty tissue that covers the pubic bone • It protects the pubic symphysis • During adolescence sex hormones trigger the growth of pubic hair on the mons pubis • Hair varies in coarseness curliness, amount, color and thickness 4
- 5. LABIA MAJORA • Referred to as the outer lips • They have a darker pigmentation • The Labia Majora: • Protect the introitus and urethral openings • Are covered with hair and sebaceous glands • Tend to be smooth, moist, and hairless • Become flaccid with age and after childbirth 5
- 6. LABIA MINORA • Referred to as the “inner lips” • Made up of erectile, connective tissue that darkens and swells during sexual arousal • Located inside the labia majora • They are more sensitive and responsive to touch than the labia majora • The labia minora tightens during intercourse 6
- 7. CLITORIS • Highly sensitive organ composed of nerves, blood vessels, and erectile tissue • Located under the prepuce • It is made up of a shaft and a glans • Becomes engorged with blood during sexual stimulation • Key to sexual pleasure for most women • Urethral opening is located directly below clitoris 7
- 8. VAGINAL OPENING INTROITUS • Opening may be covered by a thin sheath called the hymen • Using the presence of an intact hymen for determining virginity is erroneous • Some women are born without hymens • The hymen can be perforated by many different events 8
- 9. PERINEUM • The muscle and tissue located between the vaginal opening and anal canal • It supports and surrounds the lower parts of the urinary and digestive tracts • The perinium contains an abundance of nerve endings that make it sensitive to touch • An episiotomy is an incision of the perinium used during childbirth for widening the vaginal opening 9
- 10. Bartholin’s Glands (aka: Vestibular Glands) • The Bartholin's glands are located on each side of the vaginal opening. • They secrete fluid that helps lubricate the vagina. • Sometimes the ducts of these glands become obstructed. – Fluid backs up into the gland and causes swelling (Bartholin's cyst) 10
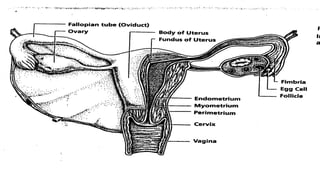
- 11. INTERNAL GENITALIA • The internal genitalia consists of the: • Vagina • Cervix • Uterus • Fallopian Tubes • Ovaries 11
- 12. 12
- 13. VAGINA • The vagina connects the cervix to the external genitals • It is located between the bladder and rectum • It functions : • As a passageway for the menstrual flow • For uterine secretions to pass down through the introitus • As the birth canal during labor • With the help of two Bartholin’s glands becomes lubricated during SI 13
- 14. CERVIX • The cervix connects the uterus to the vagina • The cervical opening to the vagina is small • This acts as a safety precaution against foreign bodies entering the uterus • During childbirth, the cervix dilates to accommodate the passage of the fetus • This dilation is a sign that labor has begun 14
- 15. UTERUS • Commonly referred to as the womb • A pear shaped organ about the size of a clenched fist • It is made up of the endometrium, myometrium and perimetrium • Consists of blood-enriched tissue that sloughs off each month during menstrual cycle • The powerful muscles of the uterus expand to accommodate a growing fetus and push it through the birth canal 15
- 16. OVIDUCTS 16
- 17. FALLOPIAN TUBES • Serve as a pathway for the ovum to the uterus • Are the site of fertilization by the male sperm • Often referred to as the oviducts or uterine tubes • Fertilized egg takes approximately 6 to 10 days to travel through the fallopian tube to implant in the uterine lining 17
- 18. 18
- 19. OVARIES • The female gonads or sex glands • They develop and expel an ovum each month • A woman is born with approximately 400,000 immature eggs called follicles • During a lifetime a woman release @ 400 to 500 fully matured eggs for fertilization • The follicles in the ovaries produce the female sex hormones, progesterone and estrogen • These hormones prepare the uterus for implantation of the fertilized egg 19
- 20. MENSTRUATION • Menarch, the onset of menstruation signals the bodily changes that transform a female body • Average age is 12.8 • Amount of bleeding varies from woman to woman • Expulsion of blood clots • Blood color can vary from bright red to dark maroon • Usually occurs every 25 to 32 days • Women can experience fluid retention, cramping, mood swings, weight gain, breast tenderness, diarrhea, and constipation 20
- 21. 21 Oogenesis
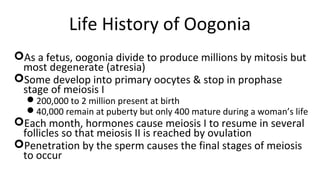
- 22. 22 Life History of Oogonia As a fetus, oogonia divide to produce millions by mitosis but most degenerate (atresia) Some develop into primary oocytes & stop in prophase stage of meiosis I 200,000 to 2 million present at birth 40,000 remain at puberty but only 400 mature during a woman’s life Each month, hormones cause meiosis I to resume in several follicles so that meiosis II is reached by ovulation Penetration by the sperm causes the final stages of meiosis to occur
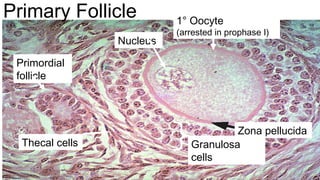
- 23. 23 Ovaries • Each follicle consists of an immature egg called an oocyte • Cells around the oocyte are called: – Follicle cells (one cell layer thick) • Stimulated to mature by FSH from the pituitary gland – Granulosa cells (when more than one layer is present) – Thecal cells: Cells in the ovarian stroma • Thecal & granulosa cells work together to produce estrogen • A protective layer of glycoprotein forms around the egg called the zona pellucida
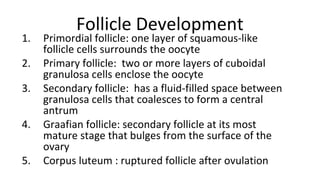
- 24. 24 Follicle Development 1. Primordial follicle: one layer of squamous-like follicle cells surrounds the oocyte 2. Primary follicle: two or more layers of cuboidal granulosa cells enclose the oocyte 3. Secondary follicle: has a fluid-filled space between granulosa cells that coalesces to form a central antrum 4. Graafian follicle: secondary follicle at its most mature stage that bulges from the surface of the ovary 5. Corpus luteum : ruptured follicle after ovulation
- 25. Ovary Histology
- 27. 27 Zona pellucida 1° Oocyte (arrested in prophase I) Granulosa cells Thecal cells Nucleus Primordial follicle Primary Follicle
- 29. 29 Graafian Follicle Fluid filled antrum Granulosa cells Oocyte 2° Corona radiata Stalk Zona pellucida
- 30. UNIT 3: FEMALE REPRODUCTIVE SYSTEM 30
- 33. OVULATION UNIT 3: FEMALE REPRODUCTIVE SYSTEM 33
- 34. OVARIAN HORMONES UNIT 3: FEMALE REPRODUCTIVE SYSTEM 34
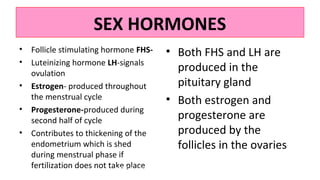
- 35. SEX HORMONES • Follicle stimulating hormone FHS- • Luteinizing hormone LH-signals ovulation • Estrogen- produced throughout the menstrual cycle • Progesterone-produced during second half of cycle • Contributes to thickening of the endometrium which is shed during menstrual phase if fertilization does not take place • Both FHS and LH are produced in the pituitary gland • Both estrogen and progesterone are produced by the follicles in the ovaries UNIT 3: FEMALE REPRODUCTIVE SYSTEM 35
- 36. DYSMENORRHEA • Painful menstrual cramps • Painful menses without evidence of a physical abnormality • Believed to be normal body response to uterine contractions • Other symptoms : • Nausea, vomiting, gastrointestinal disturbances, and fainting • Prostaglandins cause forceful, frequent uterine contractions called cramps 36
- 37. ENDOMETRIOSIS • Common cause of dysmennorrhea, dyspareunia, and infertility • Endometrium fragments and lodges in other parts of the pelvic cavity • Causes inflammation, bleeding, scarring,and adhesions • Causes are still being studied • Treated through hormonal therapy, laparoscopic surgery, or major surgical management 37