Heart Failure
- 1. Heart Failure Ma. Tosca Cybil A. Torres, RN
- 2. ETIOLOGY AND PATHOPHYSIOLOGY Heart failure (HF) is an abnormal clinical condition involving impaired cardiac pumping that results in the characteristic pathophysiologic changes of vasoconstriction and fluid retention. HF is characterized by ventricular dysfunction, reduced exercise tolerance, diminished quality of life, and shortened life expectancy. Risk factors include coronary artery disease (CAD) and advancing age. Hypertension, diabetes, cigarette smoking, obesity, and high serum cholesterol also contribute to the development of HF.
- 3. TYPES OF CONGESTIVE HEART FAILURE Right Ventricular Failure, Left Ventricular Failure Because the two ventricles of the heart represent two separate pumping systems, it is possible for one to fail alone for a short period. Most heart failure begins with left ventricular failure and progresses to failure of both ventricles Acute pulmonary edema, a medical emergency, results from left ventricular failure. If pulmonary edema is not treated, death will occur from suffocation because the client literally drowns in his or her own fluids
- 4. Forward Failure, Backward Failure In forward failure, an inadequate output of the affected ventricle causes decreased perfusion to vital signs. In backward failure, blood backs up behind the affected ventricle, causing increased pressure in the atrium behind the affected ventricle. Low Output, High Output In low-output failure, not enough cardiac output is available to meet the demands of the body. High-output failure occurs when a condition causes the heart to work harder to meet the demands of the body. Systolic Failure, Diastolic Failure Systolic failure leads to problems with contraction and ejection of blood. Diastolic failure leads to problems with the heart relaxing and filling with blood.
- 5. CLINICAL MANIFESTATIONS HF can have an abrupt onset or it can be an insidious process resulting from slow, progressive changes. Compensatory mechanisms are activated to maintain adequate CO. Cardiac compensation occurs when compensatory mechanisms succeed in maintaining an adequate CO that is needed for tissue perfusion. Cardiac decompensation occurs when these mechanisms can no longer maintain adequate CO and inadequate tissue perfusion results. The most common form of HF is left-sided failure from left ventricular dysfunction. Blood backs up into the left atrium and into the pulmonary veins causing pulmonary congestion and edema. HF is usually manifested by biventricular failure.
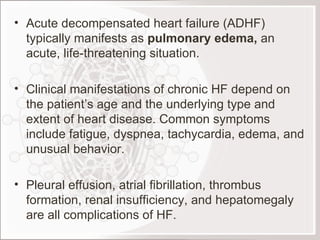
- 6. Acute decompensated heart failure (ADHF) typically manifests as pulmonary edema, an acute, life-threatening situation. Clinical manifestations of chronic HF depend on the patient’s age and the underlying type and extent of heart disease. Common symptoms include fatigue, dyspnea, tachycardia, edema, and unusual behavior. Pleural effusion, atrial fibrillation, thrombus formation, renal insufficiency, and hepatomegaly are all complications of HF.
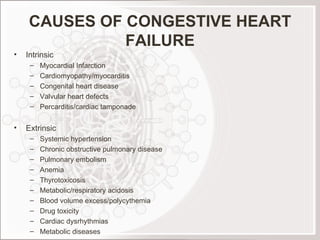
- 7. CAUSES OF CONGESTIVE HEART FAILURE Intrinsic Myocardial Infarction Cardiomyopathy/myocarditis Congenital heart disease Valvular heart defects Percarditis/cardiac tamponade Extrinsic Systemic hypertension Chronic obstructive pulmonary disease Pulmonary embolism Anemia Thyrotoxicosis Metabolic/respiratory acidosis Blood volume excess/polycythemia Drug toxicity Cardiac dysrhythmias Metabolic diseases
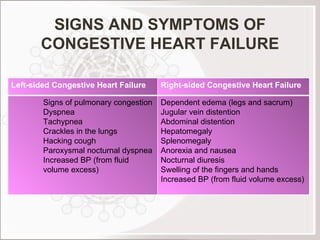
- 8. SIGNS AND SYMPTOMS OF CONGESTIVE HEART FAILURE Left-sided Congestive Heart Failure Right-sided Congestive Heart Failure Signs of pulmonary congestion Dyspnea Tachypnea Crackles in the lungs Hacking cough Paroxysmal nocturnal dyspnea Increased BP (from fluid volume excess) Dependent edema (legs and sacrum) Jugular vein distention Abdominal distention Hepatomegaly Splenomegaly Anorexia and nausea Nocturnal diuresis Swelling of the fingers and hands Increased BP (from fluid volume excess)
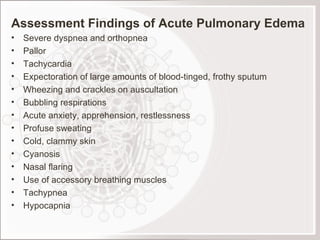
- 9. Assessment Findings of Acute Pulmonary Edema Severe dyspnea and orthopnea Pallor Tachycardia Expectoration of large amounts of blood-tinged, frothy sputum Wheezing and crackles on auscultation Bubbling respirations Acute anxiety, apprehension, restlessness Profuse sweating Cold, clammy skin Cyanosis Nasal flaring Use of accessory breathing muscles Tachypnea Hypocapnia
- 10. DIAGNOSTIC STUDIES The primary goal in diagnosis of HF is to determine the underlying etiology of HF. A thorough history physical examination chest x-ray electrocardiogram (ECG) laboratory- (serum chemistries, liver function studies, thyroid function studies, and complete blood count) hemodynamic assessment Echocardiogram stress testing cardiac catheterization
- 11. COLLABORATIVE MANAGEMENT Medications Digitalis Therapy Major therapy for CHF Has positive inotropic (strengthens force of cardiac contractility) and negative chronotropic effects (decreases heart rate) DOC: Lanoxin (Digoxin) Antidote for Toxicity: Digibind Nursing Responsibilities Assess heart rate before administration; if below 60 bpm or above 120 bpm, withhold the drug. Monitor serum potassium Assess for signs of Digitalis toxicity Bradycardia GI manifestations (anorexia, nausea, vomiting and diarrhea) Dysrhythmias Altered visual perceptions In males: gynecomastia, decreased libido and impotence
- 12. Diuretic Therapy To decrease cardiac workload by reducing circulating volume and thereby reduce preload Commonly used diuretics: Thiazides: Chlorthiazide (Diuril) Loop diuretics: Furosemide (Lasix) Potassium-Sparing: Spironolactone (Aldactone) Nursing Responsibilities Assess for signs of hypokalemia when administering loop and thiazide diuretics. Give potassium supplement and potassium-rich foods. Administer early in the morning or early in the afternoon to prevent sleep pattern disturbance related to nocturia.
- 13. Vasodilators To decrease afterload by decreasing resistance to ventricular emptying Commonly used vasodilators: Nitroprusside (Nipride) Hydralazine (Apresoline) Nifedipine Captopril (Capoten)
- 14. TREATMENT Diet: sodium-restricted diet to prevent fluid excess Activity: balanced program of activity and rest Oxygen Therapy: to increase oxygen supply
- 15. NURSING MANAGEMENT Providing Oxygenation Administer oxygen therapy per nasal cannula at 2-6 LPM as ordered Evaluate ABG analysis results Semi-Fowler’s or High-Fowler’s position to promote greater lung expansion Promoting Rest and Activity Bed rest or limited activity may be necessary during the acute phase Provide an overbed table close to the patient to allow resting the head and arms Use pillows for added support when in High-Fowler’s position Administer Diazepam (Valium) 2-10 mg 3-4x a day as ordered to allay apprehension Gradual ambulation is encouraged to prevent risk of venous thrombosis and embolism due to prolonged immobility Activities should progress through dangling, sitting up on a chair and then walking in increased distances under close supervision Assess for signs of activity intolerance (dyspnea, fatigue and increased pulse rate that does not stabilize readily)
- 16. Decreasing Anxiety Allow verbalization of feelings Identify strengths that can be used for coping Learn what can be done to decrease anxiety *** Anxiety causes increased breathlessness which may be perceived by the client as an increase in the severity of the heart failure and this in turn increases anxiety. Facilitating Fluid Balance Control of sodium intake Administer diuretics and digitalis as prescribed Monitor I and O, weight and V/S Dry phlebotomy (rotating tourniquets) Providing Skin Care Edematous skin is poorly nourished and susceptible to pressure sores Change position at frequent intervals Assess the sacral area regularly Use protective devices to prevent pressure sores
- 17. Promoting Nutrition Provide bland, low-calorie, low-residue with vitamin supplement during acute phase Frequent small feedings minimize exertion and reduce gastroistestinal blood requirements There may be no need to severely restrict sodium intake of the client who receives diuretics. “ No added salt” diet is prescribed. No processed foods in the diet. Promoting Elimination Advise to avoid straining at defecation which involves Valsalva manoeuvre. Administer laxative as ordered Encourage use of bedside commode
- 18. Facilitating Learning Teach the client and his family about the disorder and self-care Monitor signs and symptoms of recurring CHF (weight gain, loss of appetite, dyspnea, orthopnea, edema of the legs, persistent cough and report these to the physician) Avoid fatigue, balance rest with activity Observe prescribed sodium restrictions SFF rather than 3 large meals a day Take prescribed medications at regular basis Observe regular follow-up care as directed
- 19. If acute pulmonary edema occurs in the client with CHF, the following are the appropriate management: High-fowler’s position Morphine Sulfate 10-15mg/IV as ordered to allay anxiety, reduce preload and afterlaod Oxygen therapy at 40-70% by nasal cannula or face mask Aminophylline IV to relieve bronchospasm, increase urinary output and increase cardiac output Rapid digitalization Diuretic therapy Monitor serum potassium. Diuresis may result to hypokalemia.
- 20. PROGNOSIS The prognosis depends on the patient's age, the severity of the heart failure, the severity of the underlying heart disease and other factors. When congestive heart failure develops suddenly and has a treatable underlying cause, patients can sometimes return to normal heart function after treatment. With appropriate treatment, even individuals who develop congestive heart failure as a result of long- standing heart disease can often enjoy many years of productive life.