Contents
What is steatocystoma multiplex?
Steatocystoma multiplex also called multiple sebaceous cysts, steatocystomatosis, sebocystomatosis, or epidermal polycystic disease, is a rare skin disorder characterized by the development of numerous sebum-containing dermal noncancerous (benign) cysts known as steatocystomas 1, 2, 3, 4, 5. These growths begin in the skin’s sebaceous glands, which normally produce an oily substance called sebum that lubricates the skin and hair. Steatocystomas are filled with sebum. Steatocystoma multiplex lesions have been described as hamartomatous malformations of the pilosebaceous duct junction (hair follicle unit). If a single cyst of this type is found, it is called steatocystoma simplex.
In affected individuals, steatocystomas typically first appear during adolescence and are found most often on the torso, neck, upper arms, and upper legs. These cysts are usually the only sign of the condition. However, some affected individuals also have mild abnormalities involving the teeth or the fingernails and toenails. In steatocystoma multiplex, the tendency to develop cysts is inherited in an autosomal dominant fashion, so one parent can be expected to also have steatocystoma multiplex. It may also occur sporadically (non-hereditary). Both males and females may be affected.
Steatocystoma multiplex can be caused by mutations in the keratin 17 (KRT17) gene on chromosome 17q21.2 6, 7, 8, 9, 4, 10. The KRT17 gene provides instructions for making a protein called keratin 17 or K17 4, 10. Keratins are a group of tough, fibrous proteins that form the structural framework of certain cells, particularly cells that make up the skin, hair, nails, and similar tissues. Keratin 17 (K17) is produced in the nails, the hair follicles, and the skin on the palms of the hands and soles of the feet 4, 10. It is also found in the skin’s sebaceous glands, which produce an oily substance called sebum that normally lubricates the skin and hair 4, 10.
When steatocystoma multiplex is caused by mutations in the KRT17 gene, it is inherited in an autosomal dominant pattern. Autosomal dominant inheritance means one copy of the altered gene in each cell is sufficient to cause the disorder. In most cases, an affected person inherits the condition from an affected parent. In people with steatocystoma multiplex who do not have identified KRT17 gene mutations, there is usually no family history of the disorder.
Keratin 17 partners with a similar protein, keratin 6b, to form molecules called keratin intermediate filaments. These filaments assemble into dense networks that provide strength and resilience to the skin, nails, and other tissues. Networks of keratin intermediate filaments protect these tissues from being damaged by friction and other everyday physical stresses. Keratin 17 is also among several keratins involved in wound healing.
The KRT17 gene mutations that cause steatocystoma multiplex alter the structure of keratin 17, preventing it from forming strong, stable networks within cells. The defective keratin network disrupts the growth and function of cells in the skin and nails, including cells that make up the sebaceous glands. These abnormalities lead to the growth of sebum-containing cysts in people with steatocystoma multiplex. However, it is unclear why steatocystomas are typically the only feature of this disorder.
Many researchers believe that steatocystoma multiplex is a variant form of a disorder called pachyonychia congenita type 2, which can also result from mutations in the KRT17 gene 11, 12, 13, 14, 15. Like steatocystoma multiplex, pachyonychia congenita involves the growth of steatocystomas. Pachyonychia congenita is also associated with more severe nail abnormalities and a painful skin condition called palmoplantar keratoderma, which are not usually found in people with steatocystoma multiplex.
In some cases, people with steatocystoma multiplex do not have an identified mutation in the KRT17 gene. The cause of the condition in these individuals is unknown. Factors such as infections, trauma, or immunological episodes might be responsible as a trigger factor in steatocystoma multiplex 16.
Other gene mutations rarely associated with steatocystoma multiplex include N92S, R94C, and R94H 17. The gene different mutations can result in the same clinical phenotypes, whereas the same mutations can cause different clinical phenotypes 18.
The prevalence of steatocystoma multiplex is unknown, it appears to be rare 17.
A biopsy is needed for steatocystoma multiplex diagnosis, which on microscopic examination showed the cysts to be lined by stratified squamous epithelium whose stratum corneum shows wavy appearance, refractive and strongly eosinophilic without a granular layer. Sebaceous glands are usually present in the cyst wall and lanugo hair within the cyst cavity 19, 12, 5.
Steatocystoma multiplex treatment is varied and in general, unsatisfactory, because of the difficulty of approaching such disseminated lesions 17, 20. Surgery, needle aspiration, use of lasers such as CO2 and Erbium YAG, cryotherapy or oral isotretinoin are potential therapies options 12, 13, 15. However, surgical excision remains the mainstay in most cases 21, 22, 23, 24. The eventual recurrence of the lesions after treatment is the rule 1.
- Individual cysts can be removed surgically. In most cases, small incisions (cuts into the skin) allow the cyst and its contents to be extracted through the opening. If it is tethered to the underlying skin, excision biopsy may be necessary.
- Cysts can also be removed by laser, electrosurgery or cryotherapy.
- Inflammation can be reduced with oral antibiotics
- Oral isotretinoin is not curative but may temporarily shrink the cysts and reduce inflammation.
- A short course (2 to 4 weeks) of oral tetracycline, topical clindamycin, or benzoyl peroxide wash (ie, antibiotics with anti-inflammatory properties) might be considered for management of noninfectious inflammatory lesions 25, 15.
Inflamed lesions can be addressed with injection of corticosteroids or drainage 26. Use of oral isotretinoin for the treatment of steatocystoma multiplex has been reported with mixed results. Most responsive patients had steatocystoma multiplex suppurativa 27. Isotretinoin usually does not eradicate this condition, but decreases the size of suppurative lesions 26. This therapeutic response probably reflects the anti-inflammatory effect of retinoids 27.
A combination of oral rifampicin and clindamycin has shown effectiveness in the case of steatocystoma multiplex suppurativa 28. The treatment with adalimumab in patients with coexistent steatocystoma multiplex suppurativa and hidradenitis suppurativa has shown good efficacy 3.
Figure 1. Steatocystoma multiplex
Footnotes: Numerous skin-colored, freely mobile firm papules and nodules on (A) the back and (B) the forearm of a female patient that had slowly enlarged and increased in number over 5 years.
[Source 29 ]Figure 2. Steatocystoma Multiplex
Footnotes: (a) Steatocystoma multiplex over the neck. Note the yellowish nature of the lesions (b) Steatocystoma multiplex over the back.
[Source 2 ]Figure 3. Steatocystoma multiplex chest
Footnotes: Extensive steatocystoma multiplex over the chest
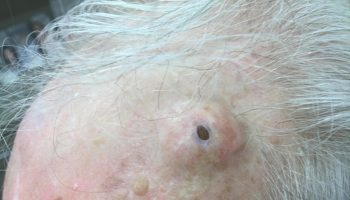
Figure 4. Steatocystoma multiplex forehead and scalp
Footnotes: (a, b) Multiple skin-colored papular and nodulocystic lesions varying in size (from 4 to 6 cm) over the forehead.
[Source 30 ]Figure 5. Steatocystoma multiplex suppurativa
Footnotes: Steatocystoma multiplex suppurativa is a much rarer inflammatory variant of steatocystoma multiplex, associated with severe inflammatory lesions resembling those of hidradenitis suppurativa. Steatocystoma multiplex suppurativa with nodulocystic lesions, scarring, and sinuses in the right armpit. Secondary bacterial infection leads to malodourous discharge and abscess 3, 31. Appropriate treatment for the suppurative form of steatocystoma multiplex includes incision and drainage as well as antimicrobial therapy 32.
[Source 30 ]What is the cause of steatocystoma multiplex?
Steatocystoma multiplex can be caused by mutations in the keratin 17 (KRT17) gene on chromosome 17q21.2 6, 7, 8, 9, 4, 10. The KRT17 gene provides instructions for making a protein called keratin 17 or K17 4, 10. Keratins are a group of tough, fibrous proteins that form the structural framework of certain cells, particularly cells that make up the skin, hair, nails, and similar tissues. Keratin 17 (K17) is produced in the nails, the hair follicles, and the skin on the palms of the hands and soles of the feet 4, 10. It is also found in the skin’s sebaceous glands, which produce an oily substance called sebum that normally lubricates the skin and hair 4, 10.
When steatocystoma multiplex is caused by mutations in the KRT17 gene, it is inherited in an autosomal dominant pattern. Autosomal dominant inheritance means one copy of the altered gene in each cell is sufficient to cause the disorder. In most cases, an affected person inherits the condition from an affected parent. In people with steatocystoma multiplex who do not have identified KRT17 gene mutations, there is usually no family history of the disorder.
Keratin 17 partners with a similar protein, keratin 6b, to form molecules called keratin intermediate filaments. These filaments assemble into dense networks that provide strength and resilience to the skin, nails, and other tissues. Networks of keratin intermediate filaments protect these tissues from being damaged by friction and other everyday physical stresses. Keratin 17 is also among several keratins involved in wound healing.
The KRT17 gene mutations that cause steatocystoma multiplex alter the structure of keratin 17, preventing it from forming strong, stable networks within cells. The defective keratin network disrupts the growth and function of cells in the skin and nails, including cells that make up the sebaceous glands. These abnormalities lead to the growth of sebum-containing cysts in people with steatocystoma multiplex. However, it is unclear why steatocystomas are typically the only feature of this disorder.
Many researchers believe that steatocystoma multiplex is a variant form of a disorder called pachyonychia congenita type 2, which can also result from mutations in the KRT17 gene 11, 12, 13, 14, 15. Like steatocystoma multiplex, pachyonychia congenita involves the growth of steatocystomas. Pachyonychia congenita is also associated with more severe nail abnormalities and a painful skin condition called palmoplantar keratoderma, which are not usually found in people with steatocystoma multiplex.
In some cases, people with steatocystoma multiplex do not have an identified mutation in the KRT17 gene. The cause of the condition in these individuals is unknown. Factors such as infections, trauma, or immunological episodes might be responsible as a trigger factor in steatocystoma multiplex 16.
Other gene mutations rarely associated with steatocystoma multiplex include N92S, R94C, and R94H 17. The gene different mutations can result in the same clinical phenotypes, whereas the same mutations can cause different clinical phenotypes 18.
Steatocystoma multiplex inheritance pattern
When steatocystoma multiplex is caused by mutations in the KRT17 gene, it is inherited in an autosomal dominant pattern. Autosomal dominant inheritance means one copy of the altered gene in each cell is sufficient to cause the disorder. In most cases, an affected person inherits the condition from an affected parent.
In people with steatocystoma multiplex who do not have identified KRT17 gene mutations, there is usually no family history of the disorder.
Steatocystoma multiplex symptoms
In steatocystoma multiplex, the tendency to develop cysts is inherited in an autosomal dominant fashion, so one parent can be expected to also have steatocystoma multiplex. It may also occur sporadically (non-hereditary). Both males and females may be affected.
The onset at puberty is presumably due to hormonal stimulus of the pilosebaceous unit. Classically, the lesions have appeared most commonly on the chest and may also occur on the abdomen, upper arms, armpits, face and groin. In some cases cysts may develop all over the body. Most often, the lesions of steatocystoma multiplex are mobile, non-tender dermal cysts without overlying surface change of the epidermis.
The cysts are mostly small (2 to 4 mm) but can grow if unchecked to form 2 cm or larger cysts 33. They tend to be soft to firm semi-translucent bumps, and contain an oily, yellow liquid. Sometimes a small central punctum can be identified and they may contain one or more hairs (eruptive vellus hair cysts). They may become inflamed and heal with scarring, like acne nodules (see nodulocystic acne and hidradenitis suppurativa).
Steatocystomas are thought to come from an abnormal lining of the passageway to the oil glands (sebaceous duct).
The largest case series of steatocystoma multiplex is a review of 64 patients for demographic, clinical, and histopathologic information 34. The study reported that the majority of cases were sporadic and that an average age of onset was 26 years (range 4 to 64 years-old) 34. The most common location of lesions was on the arms (35%), chest (29%), armpits (20%), and neck (23%) 34. Lesions were found on the legs in only 12.5% and buttocks in only 3.1% of patients. A female-to-male ratio of 1.2:1 was reported 34. The cysts of steatocystoma multiplex are usually asymptomatic. However, a suppurative variant exists and it’s called steatocystoma multiplex suppurativa. Steatocystoma multiplex suppurativa is a much rarer inflammatory variant of steatocystoma multiplex, associated with severe inflammatory lesions resembling those of hidradenitis suppurativa, in which the cysts become easily inflamed and suppurate owing to minor trauma (see Figure 5). Symptoms such as pain, itching and fever may occur in the steatocystoma multiplex suppurativa. The evolution of steatocystoma multiplex to steatocystoma multiplex suppurativa is rare and can happen at any time during the course of the disease. Reports of serious infections can result due to low socioeconomic status and poor adherence to treatment. Secondary bacterial infection leads to malodourous discharge and abscess 3, 31. Cystic lesions are often movable, with consistency ranging from firm to elastic. Nail disorder, such as hypertrophy, occur in most cases 26. Appropriate treatment for the suppurative form of steatocystoma multiplex includes incision and drainage as well as antimicrobial therapy 32.
In addition to steatocystoma multiplex suppurativa, there are other reports of rare variants of steatocystoma multiplex 19. A rare subtype of steatocystoma multiplex, which is called acral subcutaneous steatocystoma multiplex, has been described in five patients, who have experienced lesions on the flexor surfaces of the distal aspects of the arms 35. A female predominance was reported in acral subcutaneous steatocystoma multiplex, with a female-to-male ratio of 4:1 35.
Steatocystoma multiplex also has been reported to occur on the scalp, which results in a concurrent acquired hairloss that may have been secondary to trichotillomania 36. Another rare case included large, firm, disfiguring nodules that were confined to the scrotum, which revealed steatocystoma multiplex with extensive calcification that resulted in adhesion 37. Associations have been found between steatocystoma multiplex and pilar cysts, preauricular sinuses, natal teeth, and trichoblastomas 38, 39, 40.
Steatocystoma multiplex diagnosis
A biopsy is needed for steatocystoma multiplex diagnosis, which on microscopic examination showed the cysts to be lined by stratified squamous epithelium whose stratum corneum shows wavy appearance, refractive and strongly eosinophilic without a granular layer. Sebaceous glands are usually present in the cyst wall and lanugo hair within the cyst cavity 19, 12, 5.
Steatocystoma multiplex differential diagnosis
Steatocystoma multiplex differential diagnosis include:
- Acne conglobata. Acne conglobata is a rare severe form of nodulocystic acne, a severe form of acne affecting the face and upper trunk, characterized by nodules and cysts that typically resolve with scarring. Acne conglobata presents with groups of multiple comedones and inflammatory papules, pustules, and nodules involving the trunk, limbs, and buttocks. Interconnecting abscesses and draining sinuses become secondarily infected causing pain and malodour. Healing is slow, leaving unsightly hypertrophic and atrophic scars. Acne conglobata is often very persistent, lasting into the 30s or 40s. Patients with acne conglobata often need additional treatments on top of oral isotretinoin, such as oral antibiotics for secondary bacterial infection; systemic corticosteroids to reduce inflammation and adalimumab, used off-label, for resistant severe disease.
- Milia. Milia are tiny white bumps or small cysts containing keratin (the skin protein) on the skin. Milia are almost always seen in newborn babies. These harmless cysts present as tiny pearly-white bumps just under the surface of the skin. Milia occur when dead skin becomes trapped in small pockets at the surface of the skin or mouth. They are common in newborn infants. Similar cysts are seen in the mouths of newborn infants. They are called Epstein pearls. These cysts also go away on their own. Adults may develop milia on the face. The bumps and cysts also occur on parts of the body that are swollen (inflamed) or injured. Rough sheets or clothing may irritate the skin and mild reddening around the bump. The middle of the bump will stay white. Irritated milia are sometimes called “baby acne”. This is incorrect since milia are not a true from of acne. Milia do not need to be treated unless they are a cause for concern for the patient. They often clear up by themselves within a few months. Where possible, further trauma should be minimised to reduce the development of new lesions. The lesion may be de-roofed using a sterile needle or blade and the contents squeezed or pricked out. They may be destroyed using diathermy and curettage, or cryotherapy. For widespread lesions, topical retinoids may be helpful. Chemical peels, dermabrasion and laser ablation have been reported to be effective when used for very extensive milia. Milia en plaque may improve with minocycline (a tetracycline antibiotic).
- Epidermoid Cyst. Epidermoid cysts also called sebaceous cysts are the most common benign skin cysts derived from the infundibulum or upper portion of a hair follicle 41, 42. Historically, epidermoid cysts have been referred to by various terms, including follicular infundibular cysts, epidermal cysts, and epidermal inclusion cysts 41. The term epidermal inclusion cyst refers specifically to an epidermoid cyst that is the result of the implantation of epidermal elements in the dermis 41. Because most lesions originate from the follicular infundibulum, the more general term epidermoid cyst is favored. The term sebaceous cyst should be avoided because it implies that the cyst is of sebaceous origin and epidermoid cysts do not involve sebaceous glands, nor do they contain sebum. Epidermoid cysts contain soft “cheesy” like material that’s composed of keratin, a protein component of skin, hair, and nails. Epidermoid cysts form when the top layer of skin (the epidermis) grows into the middle layer of the skin (the dermis) 43. This may occur due to injury or blocked hair follicles. An epidermoid cyst may have no pain or other symptoms associated with it, but if it becomes inflamed or infected, it may grow, become painful and red, and may rupture.
Steatocystoma multiplex treatment
Medical treatments have been used with variable results to lessen inflammation, minimize scarring, and reduce the need for surgery 44, 45, 46, 47. However, surgical excision remains the mainstay in most cases 21, 22, 23, 24. The eventual recurrence of the lesions after treatment is the rule 1.
- Individual cysts can be removed surgically. In most cases, small incisions (cuts into the skin) allow the cyst and its contents to be extracted through the opening. If it is tethered to the underlying skin, excision biopsy may be necessary.
- Cysts can also be removed by laser, electrosurgery or cryotherapy.
- Inflammation can be reduced with oral antibiotics
- Oral isotretinoin is not curative but may temporarily shrink the cysts and reduce inflammation.
- A short course (2 to 4 weeks) of oral tetracycline, topical clindamycin, or benzoyl peroxide wash (ie, antibiotics with anti-inflammatory properties) might be considered for management of noninfectious inflammatory lesions 25, 15.
Reports have detailed modified techniques for surgical removal of these lesions, which are often numerous, even in the hundreds. Two patients were treated with a radiofrequency device to make 1 to 2 mm incisions followed by expression of the cyst and removal of the cyst wall with forceps. No sutures were used, no scars occurred, and there was no recurrence after five months of follow up 48. Alternatively, five patients were treated by 2 to 3 mm incision with a blade followed by removal of the cyst using a vein hook (used in ambulatory phlebectomy). The procedure was successful in all five patients, with no side effects and no recurrence over follow-up periods of 14 to 22 months 49. Lasers have been used in the treatment of steatocystoma multiplex. One patient experienced substantial clearance of lesions after two treatments using the diode laser to target the superficial sebaceous glands and the fractionated erbium-doped fiber laser to target the cystic component in the dermis 50. Another report details the successful treatment of steatocystoma multiplex in a patient with pachyonychia congenita type 2 with the erbium:yttrium-aluminum-garnet laser to create a punctum allowing for drainage of the lesions 51. There was no scarring or recurrence in three months of follow-up 51. The carbon dioxide laser has been used for cyst opening, drainage, and wall vaporization, with good cosmetic result and no recurrence over two years of follow up 32.
A combination of oral rifampicin and clindamycin has shown effectiveness in the case of steatocystoma multiplex suppurativa 28. The treatment with adalimumab in patients with coexistent steatocystoma multiplex suppurativa and hidradenitis suppurativa has shown good efficacy 3.
Steatocystoma multiplex prognosis
Steatocystoma multiplex is a benign skin disorder. In some patients, it may have psychosocial implications resulting from the disfigurement due to widespread lesions or from scarring seen in the inflammatory variant, steatocystoma suppurativa. The prognosis for patients with steatocystoma multiplex is excellent. No reports describe malignant transformation within these benign adnexal tumors.
- Rahman MH, Islam MS, Ansari NP. Atypical steatocystoma multiplex with calcification. ISRN Dermatol 2011. 2011 doi: 10.5402/2011/381901. 381901[↩][↩][↩]
- Palaniappan V, Karthikeyan K. Steatocystoma Multiplex. Indian Dermatol Online J. 2023 Dec 1;15(1):105-112. doi: 10.4103/idoj.idoj_490_23[↩][↩][↩]
- Atzori L, Zanniello R, Pilloni L, Rongioletti F. Steatocystoma multiplex suppurativa associated with hidradenitis suppurativa successfully treated with adalimumab. J Eur Acad Dermatol Venereol. 2019;33:42–4. doi: 10.1111/jdv.15848[↩][↩][↩][↩][↩]
- Steatocystoma multiplex. https://medlineplus.gov/genetics/condition/steatocystoma-multiplex[↩][↩][↩][↩][↩][↩][↩][↩][↩]
- Steatocystoma multiplex. https://dermnetnz.org/topics/steatocystoma-multiplex[↩][↩][↩]
- Antal AS, Kulichova D, Redler S, Betz RC, Ruzicka T. Steatocystoma multiplex: keratin 17 – the key player? Br J Dermatol. 2012 Dec;167,6:1395–7. doi: 10.1111/j.1365-2133.2012.11073.x[↩][↩]
- Kamra HT, Gadgil PA, Ovhal AG, Narkhede RR. Steatocystoma multiplex-a rare genetic disorder: a case report and review of the literature. J Clin Diagn Res. 2013 Jan;7,1,166–8. doi: 10.7860/JCDR/2012/4691.2698[↩][↩]
- Wang J, Li J, Li X, Lei D, Xiao W, Li Z, et al. A recurrent mutation in the KRT17 gene responsible for severe steatocystoma multiplex in a large Chinese family. Clin Exp Dermatol. 2018 Mar;43, 2:205–8. doi: 10.1111/ced.13311[↩][↩]
- Smith FJ, Corden LD, Rugg EL, Ratnavel R, Leigh IM, Moss C, et al. Missense mutations in keratin 17 cause either pachyonychia congenita type 2 or a phenotype resembling steatocystoma multiplex. J Invest Dermatol. 1997 Feb;108,2:220–3. doi: 10.1111/1523-1747.ep12335315[↩][↩]
- KRT17 gene. https://medlineplus.gov/genetics/gene/krt17/[↩][↩][↩][↩][↩][↩][↩][↩]
- Ofaiche J, Duchatelet S, Fraitag S, Nassif A, Nougué J, Hovnanian A. Familial pachyonychia congenita with steatocystoma multiplex and multiple abscesses of the scalp due to the p.Asn92Ser mutation in keratin 17. Br J Dermatol. 2014 Dec;171, 6:1565–7. doi: 10.1111/bjd.13123[↩][↩]
- Lima AM, Batista CMA, Rocha SP, Reis CMS, Leal IIR, Azevedo LEL. Esteatocistoma múltiplo. An Bras Dermatol. 2011;86:165–166. doi: 10.1590/s0365-05962011000100031[↩][↩][↩][↩][↩]
- Varshney M, Aziz M, Maheshwari V, Alam K, Jain A, Arif SH, et al. Steatocystoma multiplex. BMJ Case Rep. 2011;2011 doi: 10.1136/bcr.04.2011.4165. bcr0420114165[↩][↩][↩]
- Ha WW, Wang J, Wang W, Fu HY, Tang HY, Tang XF, et al. A novel missense mutation of keratin 17 gene in a chinese family with steatocystoma multiplex. Ann Dermatol. 2013;25:508–510. doi: 10.5021/ad.2013.25.4.508[↩][↩]
- Gordon Spratt EA, Kaplan J, Patel RR, Kamino H, Ramachandran SM. Steatocystoma. Dermatol Online J. 2013 Dec 16;19(12):20721. https://escholarship.org/uc/item/1d4682q3[↩][↩][↩][↩][↩]
- Jain M, Puri V, Katiyar Y, Sehgal S. Acral steatocystoma multiplex. Indian Dermatol Online J. 2013;4:156–7. doi: 10.4103/2229-5178.110644[↩][↩]
- Reick-Mitrisin V, Reddy A, Shah BA. A breast imaging case of steatocystoma multiplex: A rare condition involving multiple anatomic regions. Cureus. 2022;14:e27756. doi: 10.7759/cureus.27756[↩][↩][↩][↩]
- Kim JY, Park JH, Sohng C, Jang YH, Lee SJ, Lee WJ. Huge steatocystoma multiplex with new point mutation in the Exon 1 of KRT 17 Gene. Ann Dermatol. 2018;30:633–5. doi: 10.5021/ad.2018.30.5.633[↩][↩]
- Kamra HT, Gadgil PA, Ovhal AG, Narkhede RR. Steatocystoma multiplex-a rare genetic disorder: a case report and review of the literature. J Clin Diagn Res. 2013;7:166–168. doi: 10.7860/JCDR/2012/4691.2698[↩][↩][↩]
- Santana CN, Pereira DD, Lisboa AP, Leal JM, Obadia DL, Silva RS. Steatocystoma multiplex suppurativa: case report of a rare condition. An Bras Dermatol. 2016 Sep-Oct;91(5 suppl 1):51-53. doi: 10.1590/abd1806-4841.20164539[↩]
- Kamra HT, Gadgil PA, Ovhal AG, Narkhede RR. Steatocystoma multiplex-a rare genetic disorder: a case report and review of the literature. J Clin Diagn Res. 2013 Jan;7,1:166–8. doi: 10.7860/JCDR/2012/4691.2698[↩][↩]
- Rongioletti F, Cattarini G, Romanelli P. Late onset vulvar steatocystoma multiplex. Clin Exp Dermatol. 2002 Sep;27,6:445–7. doi: 10.1046/j.1365-2230.2002.01027.x[↩][↩]
- Kim SJ, Park HJ, Oh ST, Lee JY, Cho BK. A case of steatocystoma multiplex limited to the scalp. Ann Dermatol. 2009 Feb;21,1:106–9. doi: 10.5021/ad.2009.21.1.106[↩][↩]
- Wang J, Li J, Li X, Lei D, Xiao W, Li Z, et al. A recurrent mutation in the KRT17 gene responsible for severe steatocystoma multiplex in a large Chinese family. Clin Exp Dermatol. 2018 Mar;43,2:205–8. doi: 10.1111/ced.13311[↩][↩]
- Adams B, Shwayder T. Steatocystoma multiplex suppurativum. Int J Dermatol. 2008;47(11):1155–6. doi: 10.1111/j.1365-4632.2008.03698.x[↩][↩]
- Fekete GL, Fekete JE. Steatocystoma multiplex generalisata partially suppurativa–case report. Acta Dermatovenerol Croat. 2010;18(2):114-9.[↩][↩][↩]
- Apaydin R, Bilen N, Bayramgürler D, Basdas F, Harova G, Dökmeci S. Steatocystoma multiplex suppurativum: oral isotretinoin treatment combined with cryotherapy. Australas J Dermatol. 2000;41:98–100. doi: 10.1046/j.1440-0960.2000.00403.x[↩][↩]
- Ahmed G, Prabha N, Ganguly S. Familial steatocystoma multiplex generalisita suppuritiva: Oral rifampicin and clindamycin combination worth a trial. Indian J Dermatol. 2021;66:553–5. doi: 10.4103/ijd.IJD_117_20[↩][↩]
- Georgakopoulos JR, Ighani A, Yeung J. Numerous asymptomatic dermal cysts: Diagnosis and treatment of steatocystoma multiplex. Can Fam Physician. 2018 Dec;64(12):892-899. https://pmc.ncbi.nlm.nih.gov/articles/PMC6371868[↩]
- Alotaibi L, Alsaif M, Alhumidi A, Turkmani M, Alsaif F. Steatocystoma Multiplex Suppurativa: A Case with Unusual Giant Cysts over the Scalp and Neck. Case Rep Dermatol. 2019 Mar 19;11(1):71-76. doi: 10.1159/000498882[↩][↩]
- Fletcher J, Posso-De Los Rios C, Jambrosic J, Alavi A. Coexistence of hidradenitis suppurativa and steatocystoma multiplex: Is it a new variant of hidradenitis suppurativa? J Cutan Med Surg. 2021;25:586–90. doi: 10.1177/12034754211010145[↩][↩]
- Rossi R, Cappugi P, Battini M, Mavilia L, Campolmi P. CO2 laser therapy in a case of steatocystoma multiplex with prominent nodules on the face and neck. Int J Dermatol. 2003 Apr;42(4):302-4. doi: 10.1046/j.1365-4362.2003.01309.x[↩][↩][↩]
- Kamra HT, Gadgil PA, Ovhal AG, Narkhede RR. Steatocystoma multiplex-a rare genetic disorder: a case report and review of the literature. J Clin Diagn Res. 2013 Jan;7(1):166-8. doi: 10.7860/JCDR/2012/4691.2698[↩]
- Cho S, Chang SE, Choi JH, Sung KJ, Moon KC, Koh JK. Clinical and histologic features of 64 cases of steatocystoma multiplex. J Dermatol. 2002 Mar;29(3):152-6. doi: 10.1111/j.1346-8138.2002.tb00238.x[↩][↩][↩][↩]
- Marzano AV, Tavecchio S, Balice Y, Polloni I, Veraldi S. Acral subcutaneous steatocystoma multiplex: a distinct subtype of the disease? Australas J Dermatol. 2012 Aug;53(3):198-201. doi: 10.1111/j.1440-0960.2011.00851.x[↩][↩]
- Lee D, Chun JS, Hong SK, Seo JK, Choi JH, Koh JK, Sung HS. Steatocystoma multiplex confined to the scalp with concurrent alopecia. Ann Dermatol. 2011 Oct;23(Suppl 2):S258-60. doi: 10.5021/ad.2011.23.S2.S258[↩]
- Rahman MH, Islam MS, Ansari NP. Atypical steatocystoma multiplex with calcification. ISRN Dermatol. 2011;2011:381901. doi: 10.5402/2011/381901[↩]
- Sardana K, Sharma RC, Jain A, Mahajan S. Facial steatocystoma multiplex associated with pilar cyst and bilateral preauricular sinus. J Dermatol. 2002 Mar;29(3):157-9. doi: 10.1111/j.1346-8138.2002.tb00239.x[↩]
- King NM, Lee AM. Natal teeth and steatocystoma multiplex: a newly recognized syndrome. J Craniofac Genet Dev Biol. 1987;7(3):311-7.[↩]
- Gianotti R, Cavicchini S, Alessi E. Simultaneous occurrence of multiple trichoblastomas and steatocystoma multiplex. Am J Dermatopathol. 1997 Jun;19(3):294-8. doi: 10.1097/00000372-199706000-00017[↩]
- Epidermoid Cyst. https://emedicine.medscape.com/article/1061582-overview[↩][↩][↩]
- Epidermoid cyst. https://dermnetnz.org/topics/epidermoid-cyst[↩]
- Epidermoid Cyst (Sebaceous Cyst). https://skinsight.com/skin-conditions/epidermoid-cyst-sebaceous-cyst[↩]
- Gürel MS, Bitiren M, Özardalı İ. Steatokistoma multipleks. T Klin J Dermatol. 2000;10:209–12.[↩]
- Notowicz A. Treatment of lesions of steatocystoma multiplex and other epidermal cysts by cryosurgery. J Dermatol Surg Oncol. 1980;6:98–9. doi: 10.1111/j.1524-4725.1980.tb00820.x[↩]
- Krahenbuhl A, Eichmann A, Pfaltz M. CO2 laser therapy for steatocystoma multiplex. Dermatologica. 1991;183:294–6. doi: 10.1159/000247704[↩]
- Moritz DL, Silverman RA. Steatocystoma multiplex treated with isotretinoin: a delayed response. Cutis. 1988 Nov;42(5):437-9.[↩]
- Choudhary S, Koley S, Salodkar A. A modified surgical technique for steatocystoma multiplex. J Cutan Aesthet Surg. 2010 Jan;3(1):25-8. doi: 10.4103/0974-2077.63284[↩]
- Lee SJ, Choe YS, Park BC, Lee WJ, Kim DW. The vein hook successfully used for eradication of steatocystoma multiplex. Dermatol Surg. 2007 Jan;33(1):82-4. doi: 10.1111/j.1524-4725.2007.33013.x[↩]
- Moody MN, Landau JM, Goldberg LH, Friedman PM. 1,450-nm diode laser in combination with the 1550-nm fractionated erbium-doped fiber laser for the treatment of steatocystoma multiplex: a case report. Dermatol Surg. 2012 Jul;38(7 Pt 1):1104-6. doi: 10.1111/j.1524-4725.2012.02391.x[↩]
- Mumcuoğlu CT, Gurel MS, Kiremitci U, Erdemir AV, Karakoca Y, Huten O. Er: yag laser therapy for steatocystoma multiplex. Indian J Dermatol. 2010 Jul-Sep;55(3):300-1. doi: 10.4103/0019-5154.70690[↩][↩]