A 30-something male was involved in a single vehicle crash and had multiple injuries.
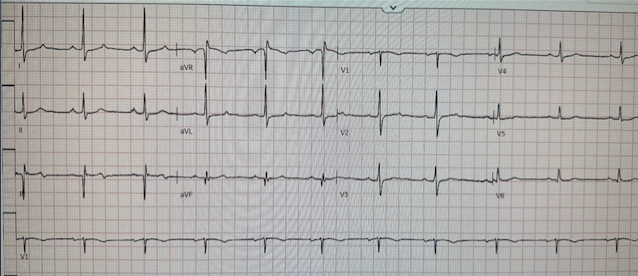
As a routine part of his critical trauma evaluation, he had an ECG recorded:
There is an rSR" in V1 and V2, with downsloping ST segment and inverted T-wave which is very similar to a Brugada Type 1 phenocopy. I was shown this ECG and thought that it could perhaps be Brugada, but I was more suspicious for Right Ventricular (RV) myocardial contusion. The RV is the most anterior part of the chest and is most likely to be contused with anterior chest trauma. Moreover, this degree of ST Elevation is very unusual for Brugada.
On the other hand, the accident was unexplained. Did the patient have an episode of VT due to Brugada, and lose consciousness while driving?
Here is one slice of the patient's chest CT
Note the pneumothorax, but the pneumothorax underlies leads V3-V5, not V1 and V2.
On the other hand, the RV lies directly under leads V1 and V2; this makes pneumothorax less likely as an etiology of the abnormal ECG.
The pneumothorax was expanded with a chest tube
At 17 hours, another ECG was recorded:
The hs troponin I peaked at 6500 ng/L -- this strongly suggests myocardial contusion. Is there also Brugada?
An echocardiogram was done. Here is the result:
The estimated left ventricular ejection fraction is 50 %.
There is no left ventricular wall motion abnormality identified.
Right ventricular prominence.
Normal right ventricular systolic performance lower limits of normal.
At 40 hours, another ECG was recorded:
Again, it has features of Type 1 Brugada
The electrophysiologist who was consulted was concerned for Brugada:
"It is unclear what precipitated his motor vehicle collision. The patient is not able to recall events preceding the crash (syncope, dizziness, lightheadedness). He has a family history concerning for arrhythmia. Given the circumstances of his car crash, we presume it was due to an underlying arrhythmia. I suspect his troponin elevation is due to acute myocardial injury (not acute thrombus) related to his polytrauma, possibly cardiac contusion, and reassuring that he has no wall motion abnormalities on TTE."
An MRI was done:
1) Normal LV function with no wall motion abnormalities
2) Normal dimensions of all cardiac chambers
3) No evidence of left ventricular myocardial scar on delayed enhancement
sequences after contrast administration
4) Hypokinesis involving the free wall of the right ventricle with delayed enhancement, concerning for right ventricular contusion. This appears to be immediately beneath the sternal fracture. At this point, recommend a short-term follow-up cardiac MRI tailored to evaluation of the right ventricle, in a few days after patient recovery.
2 weeks
Here is the final electrophysiology note:
It is unclear what precipitated his motor vehicle collision. The patient is not able to recall events preceding the crash (syncope, dizziness, lightheadedness, though reports feeling a popping sound). He has a family history concerning for arrhythmia with his father requiring some sort of device (PPM, ICD, unclear) at a young age. He has Brugada pattern on EKG with possible syncope, which is concerning for underlying paroxysmal ventricular arrhythmia. However, his cardiac MRI shows scar that is also possibly associated with his sternal fracture given his location.
Given the possibility of a ventricular arrhythmia, we would recommend the patient receive a Zoll LifeVest prior to discharge and repeat the cardiac MRI in 2-3 weeks.
Pending the results of the MRI, he could be considered for ICD placement if it does seem more consistent with Brugada syndrome rather than injury to the RV from contusion. In the meantime will use LifeVest to bridge him during ongoing workup for his RV scar.
Diagnosis:
1. Definite Right Ventricular Myocardial Contusion and
2. Possible Underlying Brugada syndrome.
If and when I get a confirmation or refutation of Brugada syndrome, I will update this post.
See our other cases of myocardial contusion and related cases (some of which have an important diagnosis OTHER THAN myocardial contusion!):
You must read this one: A Child with Blunt Trauma -- See how the ECG can be definite for myocardial contusion, but subtle, and what happens if you miss it.
===================================
MY Comment, by KEN GRAUER, MD (11/25/2022):
===================================
Highly interesting post by Dr. Smith regarding a 30-something male with multiple injuries from a motor vehicle accident. The KEY issues are highlighted by Dr. Smith's title of this post = "What is this ST Elevation, with Peak Troponin of 6500 ng/L?"
When I first saw the initial ECG in today's case — I interpreted the ECG changes in leads V1,V2 as consistent with a Brugada-1 pattern, most likely Brugada Phenocopy.
- As we've discussed on numerous other posts in Dr. Smith's ECG Blog (See My Comment at the bottom of the page in the May 5, 2022 post) — a growing number of conditions other than Brugada Syndrome have been found to temporarily produce a Brugada-1 ECG pattern. These include (among others) — acute febrile illness — variations in autonomic tone — hypothermia — ischemia-infarction — malignant arrhythmias — cardiac arrest — and especially Hyperkalemia. Patients with such conditions that may transiently mimic the ECG findings of a Brugada-1 pattern are said to have Brugada Phenocopy. The importance of being aware of this phenomenon of Brugada Phenocopy — is that correction of the underlying condition may result in resolution of the Brugada-1 ECG pattern, with a much better prognosis compared to patients with true Brugada Syndrome.
- Kazmi et al have reported on a case in which chest trauma was transiently associated with development of a Brugada-1 ECG pattern (J Am Coll Cardiol 73 [9-Supp-1], 2019). The authors postulate that the mechanism for producing the Brugada-1 ECG pattern was that anterior chest wall trauma caused a non-homogeneous depolarizing current (possibly related to opening of mechanicallly sensitive cardiac K+ATP channels). This ECG abnormality was transient in the case they report — consistent with trauma-induced Brugada Phenocopy.
- Alternatively (as per Dr. Smith) — it could be that a malignant arrhythmia that altered consciousness was the precipitating cause of both the motor vehicle crash, and of the Brugada-1 pattern on ECG.
As noted above — Dr. Smith was especially suspicious of RV (Right Ventricular) Myocardial Contusion as primarily responsible for the patient's initial ECG pattern.
- While impossible to rule out a malignant arrhythmia as the cause of the motor vehicle accident — I think it insightful to consider the combination of Brugada-1 Phenocopy + RV Myocardial Contusion as both contributing to the serial ECG changes seen in today's case.
What are the ECG Findings of Cardiac Contusion?
I've copied KEY points from My Comment in the August 6, 2022 post in Dr. Smith's ECG Blog — regarding the answer to this question. Overall — the ECG is less than optimally sensitive for detecting cardiac injury following blunt trauma. This is because the anterior anatomic position of the RV (Right Ventricle), and its immediate proximity to the sternum — makes the RV much more susceptible to blunt trauma injury than the LV. But because of the much greater electrical mass of the LV — electrical activity (and therefore ECG abnormalities) from the much smaller and thinner RV are more difficult to detect. To REVIEW (Sybrandy et al: Heart 89:485-489, 2003 — Alborzi et al: J The Univ Heart Ctr 11:49-54, 2016 — and Valle-Alonso et al: Rev Med Hosp Gen Méx 81:41-46, 2018) — ECG findings commonly reported in association with Cardiac Contusion include the following: - None (ie, The ECG may be normal — such that not seeing any ECG abnormalities does not rule out the possibility of cardiac contusion).
- Sinus Tachycardia (common in any trauma patient ...).
- Other Arrhythmias (PACs, PVCs, AFib, Bradycardia and AV conduction disorders — potentially lethal VT/VFib).
- RBBB (as by far the most common conduction defect — owing to the more vulnerable anatomic location of the RV). Fascicular blocks and LBBB are less commonly seen.
- Signs of Myocardial Injury (ie, Q waves, ST elevation and/or depression — with these findings suggesting LV involvement).
- QTc prolongation.
- Brugada Phenocopy (as per the Kazmi et al reference that I cited above).
- NOTE: Prediction of cardiac contusion "severity" on the basis of cardiac arrhythmias and ECG findings — is an imperfect science.
Additional KEY Points regarding Cardiac Contusion:
Despite the predominance for RV (rather than LV) injury — use of a right-sided V4R lead has not been shown to be helpful compared to use of a standard 12-lead ECG for detecting ECG abnormalities.
- In addition to ECG abnormalities related to the blunt trauma of cardiac contusion itself — Keep in mind the possibility of other forms of cardiac injury in these patients (ie, valvular injury, aortic dissection, septal rupture) — as well as the possibility of a primary cardiac event (ie, acute MI may have been the cause of an accident that led up to the trauma).
- ECG abnormalities may be delayed — so repeating the ECG if the 1st tracing is normal is appropriate when concerned about severe traumatic injury.
- That said — IF troponin is normal at 4-6 hours and IF the ECG is normal — then the risk of cardiac complications is extremely low.
What About Today's Case?
As I reconsidered today's case — I think the 3 serial ECGs are consistent with both ST elevation in leads V1,V2 from acute RV myocardial contusion + variations of Brugada-1 and Brugada-2 ECG Phenocopy patterns.
- For clarity — I've put together in Figure-1 a visual review of the 2 Brugada ECG patterns (from My Comment in the May 5, 2022 post) — with leads V1,V2,V3 from the 3 ECGs done in today's case.
- In ECG #1 — I still find it hard to distinguish between a Brugada-1 ECG pattern vs ST elevation in leads V1,V2 from acute RV insult vs some combination of the two. I suspect we are seeing a combined ECG effect (as well as a tall, slender R' in lead V1 from myocardial contusion-induced incomplete RBBB).
- In ECG #2 — the ST-T wave abnormality is greatly reduced, and now primarily found in lead V2. Although bearing similarity to the Brugada-2 ECG pattern (in Panel B of Figure-1) — the shape of the ST segment descent from the r' peak is unusual for a Brugada-2 pattern in that it includes a short coved segment (outlined in RED — highlighted by the BLUE arrow). Doesn't this shape look to be more consistent with superimposed ST elevation rather than a Brugada-2 pattern alone?
- In ECG #3 — this unusually shaped coved segment (outlined in RED — highlighted by the BLUE arrow) is now even more prominent. I thought this coved segment to be more consistent with superimposed ST elevation from acute RV injury rather than solely the result of a Brugada-1 and/or Brugada-2 pattern.
- BOTTOM LINE: As per Dr. Smith's discussion above — the markedly elevated serum troponin — as well as additional imaging studies confirmed RV Myocardial Contusion. While I believe the serial ECGs in today's case show variations of Brugada-1 and -2 Phenocopy — I suspect the BLUE arrows in Figure-1 highlight superimposed ST elevation from acute RV injury. That said, the "good news" — is that this patient should recover (and his ECG will most probably normalize as he does!).
-USE.png) |
Figure-1: Visual summary of ECG Patterns in Brugada Syndrome (adapted from the article by Brugada et al in JACC: Vol. 72; Issue 9; 2018) — A) Brugada-1 ECG pattern, showing coved ST-segment elevation ≥2 mm in ≥1 right precordial lead, followed by a negative T-wave. — B) Brugada-2 ECG pattern (the “Saddle-back” pattern) — showing concave-up ST-segment elevation ≥0.5 mm (generally ≥2 mm) in ≥1 right precordial lead, followed by a positive T-wave. — C) Additional criteria for diagnosis of a Brugada-2 ECG pattern (TOP: the ß-angle; BOTTOM: A Brugada-2 pattern is present if 5 mm down from the maximum r’ rise point — the base of the triangle formed is ≥4).
BELOW this summary of Brugada ECG Patterns — I've put together the V1,V2,V3 leads from the 3 serial ECGs obtained in today's case (See text). |
-USE.png)












-USE.png)






-USE.png)