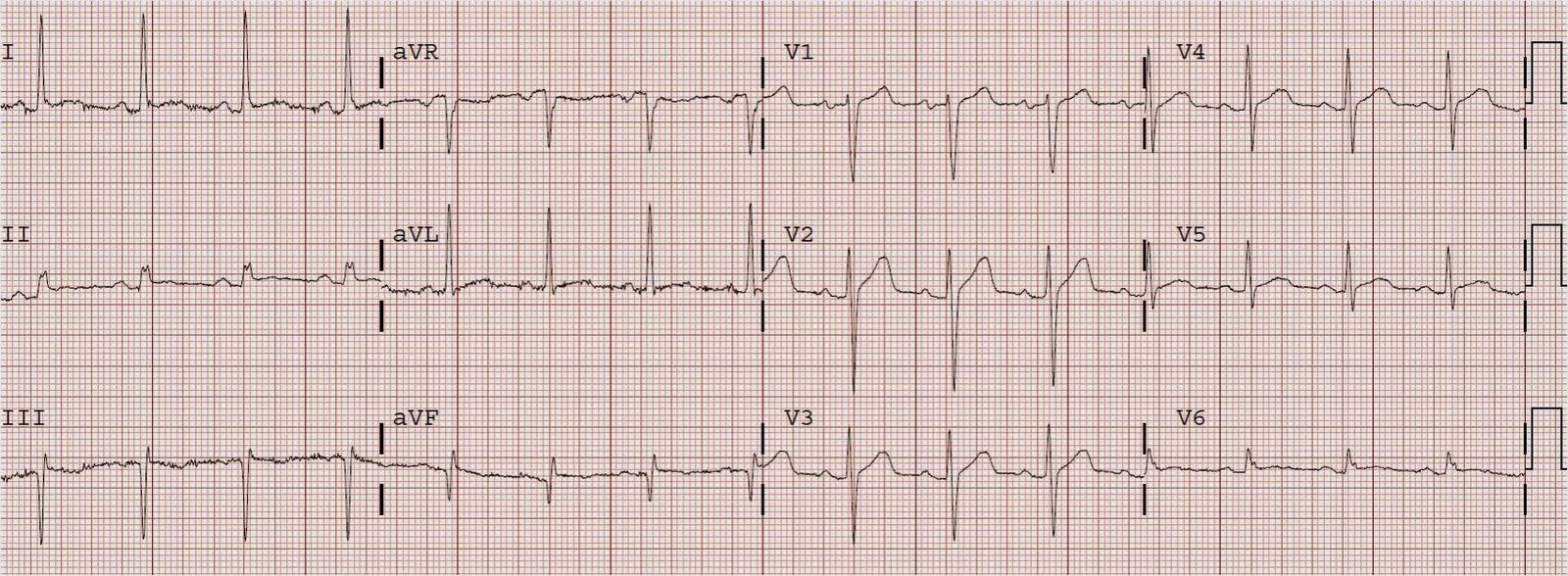
An 80 yo male presented with chest pain onset 1130 AM. The prehospital ECG was reported to have some "ST depression", but is unavaliable. His pain resolved with nitroglycerine. Here is the first ED ECG, while still pain free, was at 1350:
 |
| There is 1.5 mm of STE in V2 and about 1 mm in V1. There is an abnormal Q-waves (QR-wave) in V2 (a QS-wave in V1 may be normal). The Q-wave in V2 is one clue that this ST elevation is not normal variant. The other is some very subtle ST depression in V5 and V6. The Q-wave could be due to old MI, but they prove that MI is present and thus one can NEVER diagnose "early repolarization." |
At 1400, a second ECG was recorded:
 |
| There is now less STE in V2, 0.5 mm in V3, and a new Q-wave in V3. The ST depression is almost gone. |
Another ECG was recorded at 1418: it was identical to 1400. First troponin I returned at 0.6 ng/ml (elevated).
The cath lab was activated. A cardiologist came to assess. He opined that the ST elevation was not due to ischemia. The patient was admitted to the CCU.
At 3PM, an echocardiogram confirmed anterior wall motion abnormality.
Another ECG was recorded at 2257 that evening:
 |
| Now there is a PVC, and there are more prominent Q-waves, loss of R-wave in V2, and the T-wave has begun to invert. |
This one at 0027 is not much different:
The next AM this was recorded at 0703:
And at 0855
He was taken to the cath lab on the day after (48 hours) and had a 99% stenosis of the LAD. Max troponin was 44 ng/ml.
Convalescent echo 3 weeks later showed normal EF and no wall motion abnormality.
Is it an ongoing STEMI?
There was at least one ECG with 2 leads having at least 1 mm of ST elevation, so by some definitions, it was STEMI. We don't have an old ECG, so we can't prove at the time of presentation that the STE is new. But we do have subsequent evolution, with T-wave inversion. This proves retrospectively that the STE was new.
T-wave inversion proves reperfusion, but we don't know when that happened: some time between 1418 and 2257. Persistent ST elevation at later ECGs suggests
He did have a large amount of troponin (large MI), but we don't know if all that damage occurred before presentation.
He was pain free at presentation, so probably all the damage was done, but in some cases pain can be gone although ischemia continues.
He did have a significant wall motion abnormality (anterior); that can also happen with non-STEMI or reperfused STEMI, with an open artery.
The artery was open at angio 2 days later, but the TIMI flow was not listed in the cath report.
Is is STEMI, reperfused STEMI, or non-STEMI? At presentation, I would classify it as a reperfused STEMI. Many would classify it as a non-STEMI. The important question is: does he need immediate, emergent cath lab activation? That is to say: will more myocardium die if he does not go to the cath lab immediately? This can only be answered for certain in retrospect, not prospectively; even in retrospect, it will only be known for certain after a convalescent (weeks later) echo is done. In non-STEMI or reperfused STEMI, the wall motion should recover over time.
In fact, an echo was done 3 weeks later and showed no wall motion abnormality and normal EF, so the delay apparently was not harmful. There was no later ECG done, so I can't say if the Q-waves resolved or not.
Thus, in RETROSPECT, it was not a true, ongoing, STEMI, defined as ST elevation MI that portends continued imminent loss of viable myocardium unless there is immediate reperfusion.
Since at presentation the T-waves were still upright, the best clue to this is the absence of chest pain, but I believe it is a big risk to count on this: 1) pain can be misleading and 2) such an unstable plaque can occlude at any time.
So what would I do?? I think there is some question on the initial ECG as to whether the ST elevation is definitely new (though I would highly suspect that it is). I would get serial ECGs for a longer time, get an immediate formal echo, and ultimately I believe that these would be convincing of acute (probably reperfused) STEMI. The positive initial trop would help, but this would be positive in a nonSTEMI also. Once convinced that the STE is new, I would activate the cath lab because
acute anterior STEMI, even if reperfused, is extremely unstable and dangerous.