Abstract
Research, development and testing of wearable robotic exoskeletons for gait training and improved mobility in children with cerebral palsy (CP) and other movement disorders has become increasingly prevalent in recent years. Broadly, these devices are split into two categories: fully wearable devices that are affixed to the lower limbs and/or pelvis and systems that include a mobile frame that moves with the user. The former systems have generally targeted more functional individuals who are independent walkers while the latter target more affected individuals who do not ambulate on their own. The best strategy for children in the middle of this mobility spectrum (GMFCS III), who can walk short distances using assistive instruments like crutches or walkers, is not clear. Yet, these children may benefit most from gait training because they are at the highest risk to lose their independent mobility. Here, we present a case study of a wearable robotic exoskeleton for overground walking in a child with CP at GMFCS III. Our results demonstrate that the exoskeleton was able to synchronize assistance to five discrete phases of the gait cycle during overground walking with forearm crutches. Peak knee extension improved on average by 10 degrees in the right leg and 7 degrees in the left leg when walking with exoskeleton assistance during early stance, mid-stance and late swing without reduction in muscle activity. Therefore, state-based control for providing robotic extension assistance to individuals with crouch from CP who walk with assistive instruments should be further investigated as a potential rehabilitation strategy.
I. Introduction
Wearable robotic exoskeletons offer a potentially promising new option for gait training in individuals with neurological disorders. Until recently, the majority of exoskeletons had been designed for use in adults, usually with spinal cord injury or stroke [1, 2]. However, in the past several years, there has been a surge in development of pediatric exoskeleton devices, and more specifically, for children with cerebral palsy (CP) [3–6]. These initial cohort studies have shown promise for exoskeletons as potential assistive and therapeutic tools in this population, including the ability to improve gait velocity and step length [4], reduce the metabolic cost of walking [5], and alleviate crouch by increasing knee extension [6].
These developments are welcome given the potential clinical impact. CP is the most common movement disorder occurring in childhood [7]. Gait rehabilitation remains challenging in this population and effective solutions are still needed to combat the functional decline that often occurs during growth and development. Almost half of children who were ambulatory as children lose the ability to walk in adulthood [8]. In particular, children with less functional ability, i.e., those with Gross Motor Function Classification System (GMFCS) levels III-V, are at elevated risk for loss of function during adolescence and young adulthood [9]. Therefore, exoskeletons which enable daily gait training at high intensity in this group of children may be even more impactful by preserving or increasing functional capability that may persist throughout the lifespan.
One challenge of exoskeleton design for individuals at GMFCS levels III and above is their use of handheld assistive devices, e.g., crutches, walkers, or canes, during walking. These devices may interfere with the ability of a wearable exoskeleton to track the user’s gait pattern and therefore, deliver effective assistance (or resistance) for gait training. The objective of this study was to evaluate the feasibility of using a wearable pediatric exoskeleton (P.REX), which was previously developed and evaluated in children with GMFCS I/II [6], during overground walking in a child with crouch from CP at the GMFCS III functional level.
II. Methods
A. Robotic Exoskeleton
The P. REX exoskeleton design was based on knee-ankle-foot orthosis architecture with a single actuated degree of freedom for assistance/resistance of knee flexion and extension (Figure 1). The ankle joint is a commercially available (ADR, Ultraflex Systems, Inc., Pottstown, PA) adjustable passive mechanism. The electromechanical design details of the exoskeleton have been described previously [10]. Briefly, a motor and inline planetary gearbox (51:1 reduction, Maxon Motors, Taunton, MA) are mounted on the lateral side of the thigh (Fig. 1). A custom bevel gear right angle transmission with a 3:1 reduction ratio transmits torque between the knee joint and motor with an inline reaction torque sensor (Transducer Techniques, Temecula, CA) mounted on the output shaft at the knee. An MR encoder (Maxon) is incorporated in the motor to measure knee angle and angular velocity. A force sensitive resistor (FSR, Interlink Electronics, Westlake Village, CA) is placed under the foot from the heel to the base of the metatarsal bones to measure foot-ground contact.
Figure 1:
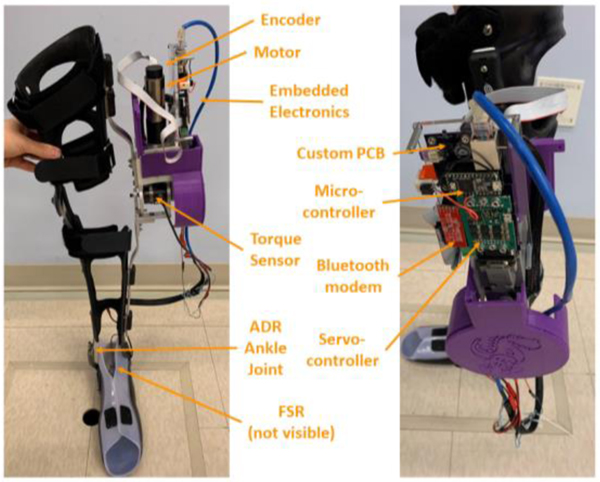
Frontal and sagittal views of the NIH P.REX wearable robotic exoskeleton for knee extension assistance.
The embedded control system including a custom designed printed circuit board (PCB) contains an ARM microcontroller (Teensy 3.2) for real-time control. The PCB also contains a wireless Bluetooth modem (BlueSMiRF, SparkFun Electronics, Niwot, CO) which uses Python code to wirelessly communicate and stream data from the exoskeleton to a host PC running a graphical user interface (GUI) [11]. The PCB also connects the motor to a commercially available servocontroller (ESCON 50/8, Maxon) which translates the command current into the motor output of the exoskeleton. The exoskeleton operates on 24V and can operate in a tethered, i.e., connected to a power supply, or untethered mode when connected to a lithium ion battery. An emergency switch is connected between the power supply to shut down the system at the push of a button.
B. Control System
The NIH P.REX implemented a hierarchical control system which consists of three layers. At the top, or supervisory, layer, a finite state machine (FSM) parses the gait cycle into discrete phases. The current design is adjustable and can split the gait cycle into 2 (stance and swing), 3 (stance, early swing and late swing), 4 (early stance, late stance, early swing and late swing) or 5 (early stance, mid-stance, late stance, early swing and late swing) states. The second layer activates the motor to provide knee extension assistance. This consists of three different modes: constant mode, impedance-trajectory mode, and adaptive mode. Constant mode allows a pre-tuned level of assistance to be specified for each state. This includes a transparent condition (zero mode) in which a net zero torque is imposed across the knee to account for system inertia and friction but no active knee assistance is provided. In impedance-trajectory mode, a target knee angle profile is specified in each state and assistance torque proportional to the difference between the target and actual knee angle is provided, subject to a maximum torque limit. In adaptive mode, assistive or resistive torque that is proportional to a real-time estimate of the user’s internal knee joint moment is provided [12]. The third layer consists of PID based feedback control combined with a feedforward loop to ensure the torque output from the motor matches the desired setting from the second layer. PID error is computed as the difference between the measured torque on the output shaft and the desired torque output from the second layer of the control system. The gains for this controller were tuned manually during bench top testing using the individual specific exoskeleton.
In this study, a 5-state FSM was used in combination with the constant control mode to provide assistance during overground walking with the P.REX. The FSM requires tuning of FSR and angular velocity thresholds to accurately segment the gait cycle into the discrete states. In this study, two different configurations of the 5 state FSM were used to provide constant knee extension assistance during overground walking: one in which constant assistance was provided during early stance, mid-stance and late swing (Est+Mst+Lsw) and one in which assistance was provided during mid-stance and late swing (Mst+Lsw). In both these conditions, assistance was implemented as a step function and the zero mode was active during states in which no assistance was provided to compensate for device friction and inertia. A third condition in which the zero mode was active during all 5 states (Zero) was also collected as a baseline.
C. Experimental Evaluation
A male participant (age: 15 years, height: 162 cm, weight: 39.9 kg) with crouch gait from bilateral spastic CP was recruited to evaluate the performance of the exoskeleton. Informed assent and consent were obtained from the participant and his guardian, respectively, prior to participation in our IRB-approved protocol (#13-CC-0210). The data presented here are part of a larger, multi-visit study evaluating the effects of robotic exoskeleton assistance in children with CP in which this participant is still active. The initial visit for the study included a medical history and physical, clinical examinations including assessment of motor function via Gross Motor Function Classification System (GMFCS) and spasticity via the modified Ashworth scale (MAS). The first visit also included measurements to enable fabrication of custom thermoplastic thigh, shank and foot shells for the P.REX exoskeleton.
The second visit was for initial fitting of the exoskeleton and tuning of the exoskeleton control system, including the thresholds for state transitions of the FSM and the assistive torque levels provided during early stance, mid-stance and late swing. The threshold settings were adjusted incrementally using the wireless GUI, which provided real-time visual feedback of the state transitions overlaid with sensor data (knee angle, angular velocity and FSR values) as the participant walked with the exoskeleton. After suitable performance of the FSM was achieved, the assistive torque during each phase was increased in 0.5 Nm increments to the maximum level at which the participant could walk while maintaining balance and reporting no discomfort. The passive ankle joint of the exoskeleton was adjusted to match the settings of the user’s AFO, which included limiting dorsiflexion to approximately 25 deg.
In the third visit, kinematic and electromyography (EMG) data were collected during overground walking with the exoskeleton for gait analysis. Two FSM walking conditions were completed as described above (Est+Mst+Lsw and Mst+Lsw) along with a third baseline condition in which no exoskeleton assistance was provided (Zero). A minimum of 5 walking bouts along the 5.5 meter overground pathway were completed for each condition. During all walking bouts, the participant used two forearm crutches for assistance, but otherwise walked independently. An overhead harness (ZeroG, Aretech, Ashburn, VA) was worn for safety in the event of a fall but did not provide body weight support. Kinematic data were collected at 100 Hz using a Vicon MX system with 12 cameras and a previously described custom marker set comprising 33 total markers placed on the feet, shank, thigh, and pelvis [6]. EMG (Trigno, Delsys, Boston, MA) was collected at 2000 Hz bilaterally from medial gastrocnemius, vastus lateralis, medial hamstrings, and rectus femoris. The exoskeleton orthosis contained pockets to prevent interference from the brace during EMG recording. A square pulse collected by the embedded exoskeleton control units and the Vicon system was used to synchronize data between the two systems. Each exoskeleton embedded controller was also operating at 100 Hz.
D. Data Analysis
Lower extremity joint angles were computed from the marker trajectories using Visual 3D software (Gaithersburg, MD). All other analysis was performed in Matlab (Mathworks, Natick, MA). Only data from steady state overground walking was analyzed. EMG data were band-pass filtered at 15–380 Hz, full wave rectified and low pass filtered at 7 Hz to create a linear envelope. Joint angles and EMG envelopes were split into gait cycles for each limb (heel-strike to heel strike) using motion capture data. Gait cycles were then time normalized using cubic spline interpolation and averaged across all cycles within a given walking condition. The primary kinematic outcome measure was the peak knee angle during stance phase, with a reduction in knee angle indicating increased knee extension. Owing to the single subject design, statistically significant differences between the baseline zero mode and the two exoskeleton modes were determined using the two standard deviation band method [13].
III. Results
A. Clinical Assessment
The participant met all inclusion criteria for the study and was assessed as GMFCS III. For daily mobility over short distances he wore AFOs and used forearm crutches for assistance. The participant had mild-moderate spasticity in the right limb (MAS scores: rectus femors: 1+; hamstring: 1; vastus lateralis: 1, gastrocnemius: 1) and left limb (MAS scores: rectus femoris: 1; hamstring: 1+; vastus lateralis: 1; gastrocnemius: 1).
B. FSM Validation during Overground Walking
Despite the use of forearm crutches for assistance during exoskeleton walking, the FSM was able to reliably parse the gait cycle into 5 discrete states during overground walking (Figure 2). The transition between stance and swing phase was dictated by an FSR threshold that was tuned separately for each limb, with the left threshold constituting ~78% of the FSR value during quiet stance while the right was ~84% of quiet stance. The transition from early to mid-stance and from early to late swing were both indicated by the transition from knee flexion to knee extension, which was identified when knee angular velocity exceeded 20 deg/sec in the extension direction. Finally, the transition from mid-stance to late stance was indicated when knee flexion velocity exceeded 20 deg/sec. The tuned knee extension assistance was set at 3 Nm (0.075 Nm/kg) for both the right and left legs (Figure 2).
Figure 2:
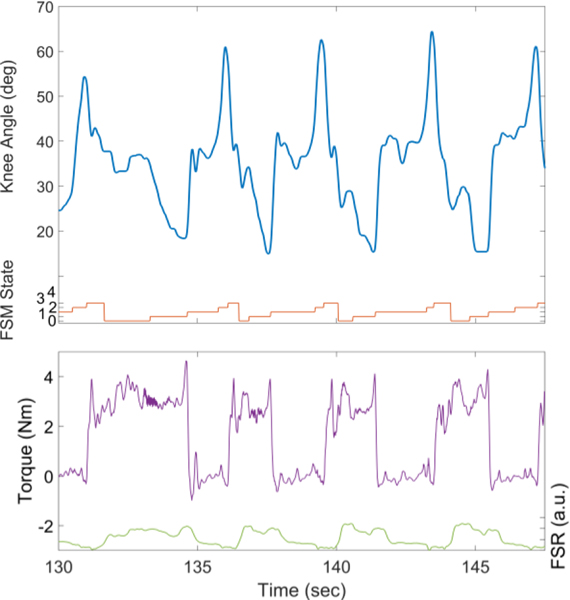
Exemplar data from walking with the exoskeleton in Est+Mst+Lsw assistance mode. In the top panel, the blue line shows knee angle measured by the exoskeleton sensors. The orange line shows the FSM state number, defined as: 0: Early stance; 1: Mid-stance; 2: Late stance; 3: Early swing; 4: Late swing. The lower panel shows knee torque (purple) and FSR (green) readings from the exoskeleton mounted sensors.
C. Effect of Robotic Assistance
There was a significant effect of robotic assistance on lower extremity kinematics during overground walking (Figure 3). As expected, the effect was most apparent at the knee joint in both limbs which each showed a shift toward knee extension during both the Est+Mst+Lsw and the Mst+Lsw exoskeleton walking conditions. Exoskeleton ssistance also appeared to have an effect on the hip. In both limbs, the hip was more extended during stance phase of both assistance conditions compared to baseline walking without assistance. There appeared to be less of an effect distally, however, as the ankle profiles were similar between exoskeleton walking with and without knee extension assistance, with the exception of the first half of mid-stance phase (10–20% gait cycle) on the right limb which showed slightly reduced dorsiflexion in the assistance conditions.
Figure 3:
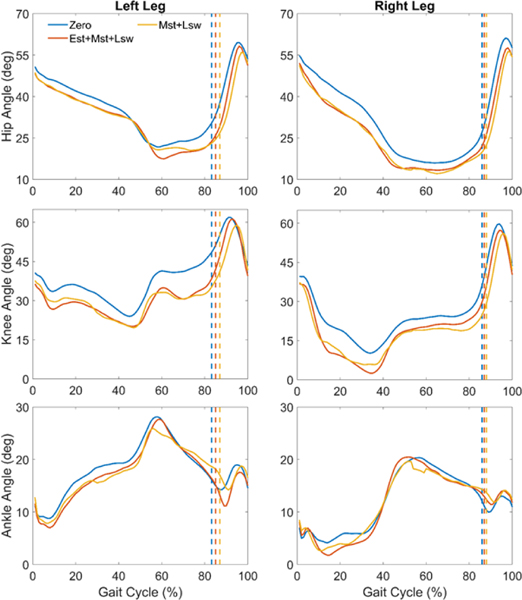
Mean lower extremity joint angles across the gait cycle during overground walking with exoskeleton assistance provided during early stance, mid-stance and late swing (orange), mid-stance and late swing (yellow) and a baseline condition with no extension assistance (zero). The vertical dashed lines indicate the median transition from stance to swing phase for each condition.
Across all 3 conditions gait speed was relatively slow, ranging from 0.17 – 0.23 m/s (Table I). Gait speed was slightly but significantly reduced in the Est+Mst+Lsw condition compared to zero mode (Table I) with no difference between Zero mode and Mst+Lsw or between the two assistance modes. Step length was asymmetric with the less crouched right leg showing greater step lengths than the left for all conditions. There was no difference in step length across the three exoskeleton conditions on the left leg, however step length was reduced in the right leg in the Est+Mst+Lsw condition compared to zero mode. No other statistically significant differences in step length were observed.
Table I.
Spatiotemporal and Knee Angle Outcomes during Exoskeleton Walking
| Condition | Zero | Est+Mst+LSw | Mst+Lsw | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Left | Right | Left | Right | Left | Right | |
|
|
||||||
| # of Strides | 16 | 19 | 17 | |||
|
| ||||||
| Gait Speed1 (m/s) | 0.23 (0.02) | 0.17* (0.02) | 0.20 (0.02) | |||
|
| ||||||
| Step Length (m) | 0.28 (0.03) | 0.43 (0.03) | 0.29 (0.04) | 0.37* (0.04) | 0.30 (0.03) | 0.39 (0.03) |
|
| ||||||
| Mean Stance Phase Knee Angle (deg) | 35.6 (7.1) | 22.3 (8.3) | 28.9 (6.2) | 16.3 (8.9) | 28.7 (5.4) | 16.7 (9.2) |
|
| ||||||
| Peak Knee Angle (deg) | 25.9 (2.5) | 13.1 (7.1) | 18.9* (4.1) | 2.9 (5.5) | 19.1* (1.1) | 5.8 (1.4) |
Data are presented as mean (standard deviation)
Significant difference with Zero condition
Robotic knee extension assistance significantly improved crouch gait (Table I). In both assistance modes peak knee extension was significantly greater than walking in the zero mode in the left leg. In the less crouched right leg, there was greater improvement in peak knee extension on average than the left leg, though the difference did not reach significance due to elevated variability in the zero mode. Similarly, mean knee extension during stance phase was increased by 7 degrees in the left leg and 6 degrees in the right leg when walking with exoskeleton assistance (Table I).
The improvement in knee extension posture occurred with minimal changes to muscle activity profiles over the gait cycle (Figure 4). Notably, there was no change in hamstring EMG in response to knee extension assistive torque in either assistance mode. In the right limb there appeared to be reduced vastus lateralis and gastrocnemius activity during the early stance phase (0–10% gait cycle). Vastus lateralis activity during late stance (50–70% gait cycle) was elevated during the assistance conditions in the right limb. Finally, gastrocnemius activity was slightly elevated during mid-stance phase (10–40% gait cycle) when walking with exoskeleton assistance.
Figure 4:
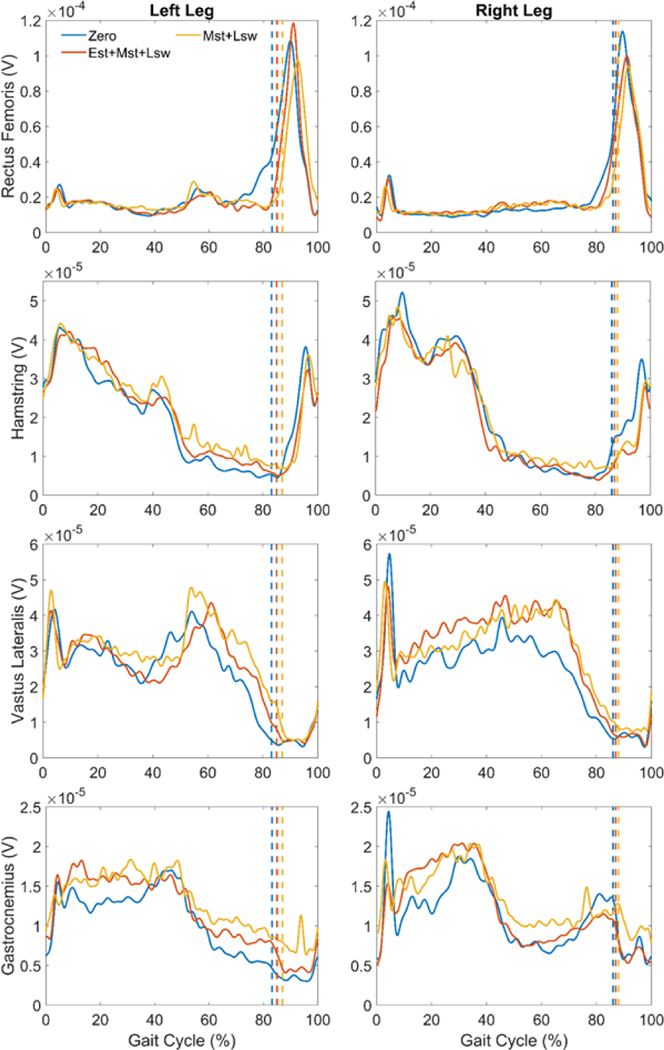
Mean EMG linear envelopes for rectus femoris, medial hamstring, vastus lateralis and gastrocnemius plotted vs. percent gait cycle during overground walking with exoskeleton assistance provided during early stance, mid-stance and late swing (orange), mid-stance and late swing (yellow) and a baseline condition with no extension assistance (zero). The vertical dashed lines indicate the median transition from stance to swing phase for each condition.
IV. Discussion
The results from this case study establish the initial feasibility of using state based closed loop control to provide targeted knee extension assistance to a child with crouch gait from CP during independent overground walking with concurrent use of forearm crutches for assistance. We previously validated this approach in more functional children who did not require assistive aids (GMFCS I/II) [6], albeit with only three states (stance, early swing and late swing). Here, the number of states was extended to five by splitting stance into early, mid- and late phases based on knee angular velocity with the goal to make knee extension assistance more synergistic with knee function during the gait cycle.
The FSR thresholds were tuned to a lower percentage of body weight than earlier studies, this likely was due to the upper extremity support provided by the forearm crutches. They were also asymmetric, a possible indicator that arm support was as well. Future studies with instrumented crutches could further elucidate the role of arm support in exoskeleton walking. Yet, symmetric knee angular velocity thresholds that governed state changes within stance and swing were sufficient for accurate state determination (Figure 2). The 20 deg/sec threshold magnitudes were identified as the minimum value that resulted in robust real-time state transitions given that velocity is computed from differentiated knee angle. Tuning of all thresholds was performed once, and these thresholds remained consistent between the second and third visits of the protocol. Future work will examine whether threshold stability remains consistent across additional sessions walking with the exoskeleton.
Both peak knee extension and mean knee extension during stance phase improved when walking with knee extension assistance compared to without. Providing extension assistance during early stance made no difference in knee angle outcomes in the more crouched left limb, and only slightly improved peak knee extension in the less affected right limb. A possible explanation for this is the relatively short duration of early stance phase, defined as the period of knee flexion after foot contact, in this participant (Figure 3). Although assistive torque was tuned for each leg individually, 3 Nm was the maximum tolerated by the participant after the initial session. Additional improvement in knee extension may be achieved in the future with greater extension assistance, particularly in the more crouched left limb.
We observed a slight reduction in gait speed, particularly in the Est+Mst+Lsw condition. In our prior study in children with crouch who were GMFCS I/II gait speed was reduced during the first data collection session but after 3 practice sessions gait speed returned to baseline levels [6, 14]. Knee extension assistance was provided during all of stance phase and late swing in the prior study, whereas it was only provided during early stance, mid-stance and late swing here because providing extension assistance during late stance/pre-swing could inhibit passive flexion in preparation for leg swing. Interestingly, the reduction in gait speed was lower when assistance was only provided during mid-stance and late swing, suggesting that this mode may be less disruptive, at least initially, to walking speed. A similar reduction in step length was observed in the less-affected right limb. The data for this case study were collected after only one initial tuning and practice session with the exoskeleton, and the protocol is ongoing with up to 10 total visits. Therefore, we hypothesize that similar to our earlier studies [6, 14] spatiotemporal measures will return to, or possibly even exceed, baseline levels after sufficient practice walking with the exoskeleton.
Similar to gait speed and step length, crouch reduction during exoskeleton walking also improved with practice in our previous study [6]. We saw immediate improvements in knee extension in this participant, despite a lower duty cycle of assistance compared to previous studies and the use of forearm crutches. There was a slight improvement when assistance was provided during early stance and mid-stance compared to mid-stance alone (Table I). Knee extension assistance also improved extension at the hip, but did not appear to have a significant effect distally at the ankle. Future work will investigate whether this effect persists after more practice time to accommodate to the exoskeleton. Further, given the effect on gait speed it may also be necessary to balance the assistance duty cycle with overall gait speed in more affected individuals who walk with assistance aides such as crutches.
Another notable observation was the lack of difference in EMG activity between walking with and without exoskeleton knee extension assistance (Figure 4). In prior studies we observed in some individuals increased knee flexor muscles activity in response to robotic extension assistance, especially during early and late stance [6]. Despite clinical presence of mild-moderate spasticity as assessed by modified Ashworth scale, no such response was observed in this participant. These results may therefore indicate that assistance which is more synergistic to knee function may reduce spastic response, although this needs to be confirmed in more participants and over multiple visits. Future work will also focus on comparing the different P.REX assistance modes, including impedance and adaptive, to determine which produces the best gait improvements for each user.
Acknowledgment
The authors thank K. Alter, J. Matsubara, B. Shideler and C. Stanley for assistance with data collection and analysis. The authors thank Chris Robbins and Mark DeHarde of Ultraflex Systems, Inc. for fabricating the custom orthotics for the exoskeleton.
This research was supported by the Intramural Research Program of the NIH Clinical Center.
References
- [1].Contreras-Vidal JL, et al. , “Powered exoskeletons for bipedal locomotion after spinal cord injury,” J. Neural Eng, vol. 13, 031001, 2016. [DOI] [PubMed] [Google Scholar]
- [2].Marchal-Crespo L. and Reinkensmeyer DJ, “Review of control strategies for robotic movement training after neurologic injury.” J. Neuroeng. Rehabil, vol. 6, 20, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Patané F, et al. , “WAKE-Up exoskeleton to assist children with cerebral palsy: design and preliminary evaluation in level walking,” IEEE Transactions on Neural Systems and Rehabilitation Engineering, vol. 25, no. 7, pp. 906–916, 2017. [DOI] [PubMed] [Google Scholar]
- [4].Bayón C, et al. , “Locomotor training through a novel robotic platform for gait rehabilitation in pediatric population: short report. J NeuroEngineering Rehabil vol. 13, 98, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Lerner ZF et al. , “An untethered ankle exoskeleton improves walking economy in a pilot study of individuals with cerebral palsy,” IEEE Trans Neural Syst Rehabil Eng, vol. 26, no. 10, pp. 1985–1993, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Lerner ZF, Damiano DL and Bulea TC, “A lower-extremity exoskeleton improves knee extension in children with crouch gait from cerebral palsy,” Sci. Transl. Med, vol. 9, no. 404, eaam9145, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Himpens E, et al. , “Prevalence, type, distribution, and severity of cerebral palsy in relation to gestational age: A meta-analytic review,” Develop. Med. Child Neurol, vol. 50, pp. 334–340, 2008. [DOI] [PubMed] [Google Scholar]
- [8].Bottos M. and Gericke C, “Ambulatory capacity in cerebral palsy: Prognostic criteria and consequences for intervention. Dev. Med. Child Neurol, vol 45, pp. 786–790, 2003. [DOI] [PubMed] [Google Scholar]
- [9].Hanna SE, et al. , “Stability and decline in gross motor function among children and youth with cerebral palsy aged 2 to 21 years,” Dev. Med. Child Neurol, vol. 51, no. 4, pp. 295–302, 2009. [DOI] [PubMed] [Google Scholar]
- [10].Chen J, et al. , “Design advancements toward a wearable pediatric robotic knee exoskeleton for overground gait rehabilitation.” 7th IEEE International Conference on Biomedical Robotics and Biomechatronics (Biorob), pp. 37–42, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Tucker L, et al. , “An open source graphical user interface for wearable robotic technology,” Journal of Rehab Assist Technologies Eng, under review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen J, et al. , “Validating model-based prediction of biological knee moment during walking with an exoskeleton in crouch gait: potential application for exoskeleton control,” 16th IEEE International Conference on Rehabilitation Robotics, pp. 778–783, 2019. [DOI] [PubMed] [Google Scholar]
- [13].Nourbakhsh MR and Ottenbacher K, “The statistical analysis of single-subject data: A comparative examination. Physical Therapy, vol. 74, pp. 768–776, 1994. [DOI] [PubMed] [Google Scholar]
- [14].Lerner ZF, Damiano DL and Bulea TC, “The effects of exoskeleton assisted knee extension on lower-extremity gait kinematics, kinetics and muscle activity in children with cerebral palsy,” Scientific Reports, vol. 7, 13512, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]


