Abstract
For people diagnosed with a mental illness, psychiatric hospitalization is one step in a long journey, consisting of clinical recovery such as removal of symptoms, and social reintegration involving resuming social roles and responsibilities, overcoming stigma and self-maintenance of the condition. Both clinical recovery and social reintegration need to go hand-in-hand for the overall well-being of individuals. However, research exploring social media for mental health has considered narrower, disjoint conceptualizations of people with mental illness – either as a patient or as a support-seeker. In this paper, we combine medical records with social media data of 254 consented individuals who have experienced a psychiatric hospitalization to address this gap. Adopting a theory-driven, Gaussian Mixture modeling approach, we provide a taxonomy of six heterogeneous behavioral patterns characterizing peoples’ mental health status transitions around hospitalizations. Then we present an empirically derived framework, based on feedback from clinical researchers, to understand peoples’ trajectories around clinical recovery and social reintegration. Finally, to demonstrate the utility of this taxonomy and the empirical framework, we assess social media signals that are indicative of individuals’ reintegration trajectories post-hospitalization. We discuss the implications of combining peoples’ clinical and social experiences in mental health care and the opportunities this intersection presents to post-discharge support and technology-based interventions for mental health.
Additional Key Words and Phrases: mental health, social media, psychiatric hospitalization, health status transitions, Facebook
1. INTRODUCTION
Emerging from the deinstitutionalization movement in the late 20th century, the recovery model has been the guiding principle of mental health policy in many countries [9]. It views recovery as “a personal journey rather than a set outcome, and one that may involve developing hope, a secure base and sense of self, supportive relationships, empowerment, social inclusion, coping skills, and meaning” [52]. In essence, recovery from mental illness not only involves removal of symptoms and restoration of functioning but also involves recovery from the stigma and negative stereotypes, from the lack of opportunities and finding a way of living a hopeful and contributing life despite the limitations caused by the illness [58, 69, 94, 131, 152]. It provides a holistic perspective arguing that people with mental illness face the complementary experiences of clinical recovery (i.e., reduction of symptoms), and social reintegration (i.e., restoration of social lives and community inclusion) hand-in-hand [78, 148, 155]. Importantly, per this model, peoples’ mental health states are temporally situated experiences that are part of their recovery and reintegration journeys themselves.
For mental health, work in the HCI and CSCW areas identify social media as an important tool serving as a mechanism to study peoples’ mood, communication, social interactions, and psychological states. However, despite the guidelines from the recovery approach, this body of work has considered mutually disjoint, discrete conceptualizations of the individual experiencing mental disorder. One line of work emphasizes the role of the individual as a patient, as someone with a validated diagnosis, receiving treatment, and on the road to clinical recovery from a mental illness. Work in this area leverages individuals’ social media data to explore the efficacy of predictions in supporting early diagnosis, evidence-based treatment, and deploying timely patient-provider interventions [27, 34, 54, 132]. Another line of work emphasizes the individual’s role as a support seeker who makes sensitive self-disclosures and participates in online health communities to maintain their mental health outside clinical care [7, 8, 45, 55, 122, 140].
However, as posited by the recovery approach, one’s role as a patient and as a support seeker are not dichotomous, and peoples’ experiences are often in transition along the course of illness. When we project narrow, oversimplified conceptualizations of the individual as either a patient or support seeker, and fail to understand the relationship between the two, we do not account for the contextualized, multiple, and heterogeneous experiences of people in reality. With emerging evidence about the potential of social media to support clinical diagnostic predictions and social support provisions [8, 27, 34, 54], it is timely to examine the intersection of these two perspectives.
In this paper, we ask, how can we study the different journeys of those with mental health conditions combining their experiences of clinical recovery and social reintegration? Anchoring on psychiatric hospitalizations as a liminality [154], during which people enter and leave the role as a patient to self-manage their condition, we focus on three research questions:
RQ1: What self-presentation and behavioral signals on social media characterize individuals’ mental health statuses around psychiatric hospitalizations?
RQ2: What trajectories on social media showcase transitions between these statuses surrounding the hospitalizations?
RQ3: What social media-based signals are indicative of social reintegration trajectories of individuals following hospitalizations?
To answer these questions, we combine data from medical records comprising clinical information related to diagnosis codes and hospitalization dates, with social media data from Facebook archives of 254 consented participants who have experienced at least one hospitalization for psychosis (N=142), mood disorders (N=106), or other mental health conditions (N=6). Across all participants, we compile over 980 thousand Facebook posts around 372 hospitalization events. Then towards answering RQ1, we adopt the Possible Selves framework [103] as a theoretical lens to capture and interpret peoples’ conceptions of self-knowledge and alternate versions of themselves in the future. With this framework, we use Gaussian Mixture Models (GMM) [108] to enumerate common behavioral patterns or “possible selves statuses” (PSS) on Facebook seen around participants’ hospitalizations: self-regulation, self-awareness, sociality, withdrawal, re-adjustment, and incorporation-focused. We validate the GMM components with qualitative interviews with clinical domain experts and define a taxonomy of six possible selves exhibited on Facebook surrounding psychiatric hospitalizations. Next, to address RQ2, we present a linear transition model between the derived PSS during the periods before and after hospitalizations to understand peoples’ clinical recovery and social reintegration trajectories, contributing an empirical framework of mental health transitions. Finally, for RQ3, to demonstrate the utility of the derived taxonomy and the framework of mental health status transitions, we define a PSS-based operationalization of social reintegration. We conduct regression analyses to assess signals on Facebook that are associated with successful social reintegration post-hospitalization.
Through a theory-driven modeling approach based on the possible selves framework and insights clinically-grounded in the recovery model, our work presents a first step towards understanding personalized and heterogeneous behaviors and self-presentations of people as they experience mental health status transitions around psychiatric hospitalizations. We discuss the theoretical implications of combining peoples’ clinical and social experiences in mental health care and the opportunities this intersection presents to post-discharge support, sensemaking in healthcare settings, and technology-based interventions for mental health. Finally, we put forth what it means to design social media platforms for online social reintegration after major life transitions.
2. BACKGROUND AND RELATED WORK
2.1. Clinical Studies of Psychiatric Hospitalization Experiences
Since the deinstitutionalization movement [10], the role of the psychiatric hospital has shifted from a place for long-term stay and treatment to a community-based system of care emphasizing reducing feelings of dependency, and supporting integration [139]. Today, when patients are admitted to a psychiatric bed, the goals of clinical care revolve around crisis stabilization, diagnosis, and initiation of appropriate treatment [139]. Once patients’ symptoms stabilize, this model encourages rapid discharge from the hospital so that individuals may continue receiving care in outpatient settings.
However, psychiatric hospitalizations are still life-altering, as the admission often implies that individuals are unequipped to manage their psychiatric needs and require removal from their existing environment to receive appropriate, urgent care [32]. When an individual is admitted to a hospital for mental illness, it is often due to an adverse event like self-harm or suicidal ideation, lack of insight or denial of illness, social crises such as relationship problems, or non-compliance with medication [89]. Based on the symptoms, treatment during hospitalization involves individual and group therapy, psychotherapy, pharmacotherapy, or other standing medication [162]. Such circumstances increase stress experienced by the patient and their caregivers, leading to perceptions of hospitalization-related anxiety, and fear of confinement [120]. Recovery journeys of people post-hospitalization are similarly challenging due to the high likelihood of re-hospitalization [153], lack of support, non-adherence and side effects to medication, and difficulty in managing the condition and reintegrating back to social life and roles [89]. Paksarian et al. [120] found 69% of participants reporting at least one of their hospitalizations as traumatic, with the most common experiences related to rigidity and involuntary hospitalization, being put on restraints, and being forced to take medications. Ådnanes et al. [3], on the other hand, found participants reporting re-hospitalizations to be less traumatizing than the first hospitalization, a necessary relief, as occurring by default and without progress, and as part of the recovery process.
Whether positive or negative, while re-hospitalizations reflect the clinical aspects of recovery journeys, social processes are found to be equally important. Based on a systematic review and narrative synthesis of the literature, Leamy et al. [94] identified five categories (CHIME): connectedness, hope and optimism about the future, identity, meaning in life, and empowerment to engender recovery processes. Hope, agency, opportunity for purposeful activity, and social inclusion are measured as outcomes of recovery in mental health [117]. In fact, successful social reintegration involving resuming “age, gender, and culture appropriated roles, statuses and activities” [47] and community participation [2] can help reduce stigma and improve overall well-being [155].
Underpinning this interplay of clinical and social processes is the recovery approach [9], as introduced in Section 1. Notable here is the work of Corey Keyes, who has advocated viewing recovery as flourishing in life despite having a mental illness and relying on two complementary reintegration experiences: the restoration from mental illness and the optimization of positive mental health [129]. These perspectives put the individual in the center and highlight the importance of understanding interrelationships over time and episodes like hospitalizations as part of “life course experiences with health” [146]. Combining medical records information (e.g., hospitalizations) and social media data of people suffering from mental distress, in this paper, we adopt the recovery and person-centered care approach in our characterization of mental health status transitions to capture social and clinical aspects of peoples’ hospitalization experiences.
2.2. Study of Mental Health Experiences in the Social Computing Literature
In the last decade, social media has emerged as an important tool in mental health, meeting various social, technical, public health, and clinical goals. The first category of this research includes computational and predictive approaches using social media data to infer peoples’ mental health states, targeting different conditions [15, 27, 35, 134], platforms [27, 141], and disciplines [16, 17, 34, 72]. Interest in social media data stems from the fact that it is readily available and can be unobtrusively gathered, overcoming challenges in state of-the-art clinical assessments of mental health that involves subjective recollection of historical facts – a method prone to retrospective recall bias [38]. We refer to these works appropriating social media data to inform clinical efforts around early diagnosis, tailoring treatment, or delivering patient-provider interventions as perspectives on clinical care in mental health.
In a second category, we find approaches to study people’s motivations, goals, and practices in using social media for support and help-seeking behaviors, often outside of clinical treatment. For instance, Andalibi et al. found that individuals struggling with negative emotions, such as that related to depression or self-harm, use Instagram to self-disclose and engage in storytelling about their stigmatized experiences [8]. Further relating to stigmatized experiences around mental health, both qualitative and quantitative studies have identified how platform interactions lead to self-disclosure, social capital and social support goals and outcomes [7, 44, 115, 119, 163]. We consider this body of research to provide perspectives on social care in mental health.
However, pathways to social care (relating to support, disclosure, stigma, etc.) and clinical care (relating to symptom management, etc.) are not dichotomous. Both social relationships and clinical care are required to improve the overall well-being of those with mental illnesses [155]. Despite this, current approaches in social computing to study mental health are heavily focused either on diagnostic interventions or management of the illness and social support, as noted above.
Ernala et al. [54] critiqued this disjoint consideration of the mental health experience in social computing literature. This work found that social media-based “proxy diagnostic signals” used to characterize people’s mental illness diagnoses on social media do not generalize to patient populations; thus revealing significant behavioral differences between patients with a valid clinical diagnosis who use social media, and those seeking help for their mental distress online. To realize the potential of social media in mental health, we argue that it is crucial to consider the mental health experience of an individual as a whole, intertwining their clinical and social recovery journeys. In this paper, we synthesize viewpoints from both clinical and social care perspectives to study how mental health related major life transitions – hospitalizations – are exhibited on social media. For this, we combine medical records comprising clinical information on diagnosis and hospitalizations with social information about online self-presentation and social interactions.
2.3. Social Media, Health Transitions and Liminality
“Transition” is a concept widely used in the social science literature and is most commonly defined as “a process of convoluted passage during which people redefine their sense of self and redevelop self-agency in response to disruptive life events [93].” While some conceptualize transitions as linear processes with a clear beginning and end [154], others note that transitions can be “complex, nonlinear, sometimes cyclical and potentially recurring” [65, 92].
2.3.1. Social Media Use around Major Life Transitions.
Technologies like social media play an important role during major life transitions and help individuals establish a “new normal” [73, 105], conduct identity work [46, 111] and reach out to similar others [136]. Prior research has examined the use of social media platforms like Facebook [22], MySpace, Tumblr [73] and Twitter [46] around several events marking major life transitions such as engagement [46], marriage [106], parenthood [64], loss of a job [22], divorce [160], the loss of a loved one [19, 63, 79, 104], and transition to college [144]. Research has also shown that people actively shape their digital footprints on these platforms by curating the self-presentation signals representative of a prior identity [73]. Researchers have also identified changes in language use [19] and behaviors on social media surrounding transitions [41, 43]. Our work contributes to this literature by examining psychiatric hospitalizations, an unexplored life event under the lens of life transitions. We build on the methods and findings in these existing studies to identify shifts in individuals’ self-presentation and behavioral signals during transitions, relative to a previous ‘normal.’
2.3.2. Modeling and Understanding Health Transitions.
Prior work in HCI and CSCW has explored different approaches to characterize and model health status transitions [81, 98, 121]. Relevantly, MacLeane et al. [101] developed a taxonomy of phases of addiction on Forum 77, an online health forum, using the transtheoretical model of behavior change [128]. Hayes et al. [76] defined the concept of a ‘personal cancer journey’ drawing from an in-depth study of cancer communities, while Jacobs et al. [86] presented a holistic framework describing the cancer journey from patient-centered perspectives (also see Levonian et al. [95]). Eschler and Pratt identified the tasks related to challenges and responses in different phases of young adult cancer during diagnosis, treatment and survivorship [57]. Wen and Rose [157] developed machine learning methods to extract cancer event trajectories from messages in online breast cancer support groups. Liu et al. [98] similarly combined domain knowledge and machine learning methods to form a hierarchical classification of Twitter data that resolves different stages of drinking behavior. Feuston et al. studied how people get back to their social lives following traumatic brain injury. and they introduced the concept of social re-emergence as “a non-linear process of developing a new social identity that involves withdrawing from social life, developing goals for social participation, disclosing health information for social support and acceptance, and attaining social independence.” [59]. Drawing on the notion of illness trajectory introduced by Strauss and colleagues [36, 149], Chen et al. discuss chronic care cycles, the repeated cycles between routine medical visit and subsequent homecare period [28]. Burgess et al. [21] studied how patient information work shifts over time and highlight two distinct but often overlapping phases, ‘learning’ and ‘living with’ a chronic condition.
In the case of mental health status transitions around hospitalizations, complex, cyclical and potentially recurring transitions are likely due to the high likelihood of relapse. As a first step into the study of recovery and reintegration transitions in mental health, we focus on individual hospitalization events in a person’s journey with mental illness. For easier interpretation, we propose a linear transition model to understand recovery and reintegration trajectories after hospitalization. Further, we expect multiple co-occurring self-presentational and behavioral changes related to clinical and social processes, per the recovery model [9] (Section 2.1). Therefore, we adopt the Possible Selves framework [103], described in Section 4.1, to guide our modeling approach and interpret findings.
2.3.3. Psychiatric Hospitalization as a Liminal Period.
Many major life transitions, including health transitions, are marked by rituals. Van Gennep’s [154] liminality framework refers to transitory processes as comprising preliminal, liminal, and postliminal stages, that relate to separating from a previous identity, making the transition, and incorporating back into the social world after transition, respectively. In the context of health transitions, Kaziunas and colleagues examined the interconnections between information and emotion work performed by bone marrow transplant caregivers by adopting a liminality lens [88]. The findings from this work highlight the usefulness of the liminality framework to make visible the work involved in navigating multiple social lives (as a part of everyday life and as a medical caregiver.) Following Van Gennep, hospitalizations for mental illnesses, the duration of which can range between a day to 4 months [107], can also be considered as institutionalized rituals and periods of liminality. While the individual transitions to their role as a patient in the hospital, there are many rules and rituals set by the hospital that they have to follow, including initially being in a locked ward that they cannot leave at will, and following a schedule for their meals, treatments, and activities. Importantly, in many cases, there is a lack of access to technology, social support, and offline connections [32, 120]. Finally, post-discharge from the hospital, individuals need to manage their new treatment plans and reintegrate back to professional, personal, or social lives [2].
3. DATA
3.1. Participant Recruitment and Data Collection
For this study, we utilized Facebook data of consented participants with a medical history of at least one hospitalization due to a mental health condition. This data was collected as a part of a broader research study involving the paper’s authors, aimed at identifying technology-based mental health information to provide early identification, intervention and treatment to patients with psychiatric disorders. The research protocol was approved by the Institutional Review Board (IRB) of the coordinating institution managing patient recruitment – a large healthcare organization in the north-east of the United States, as well as the local IRBs at collaborating sites.
Individuals over 15 years of age were recruited from various inpatient and outpatient psychiatric departments at the coordinating and partner institutions. Participants were eligible if they were diagnosed with a schizophrenia spectrum disorder, mood disorder with and without psychotic features, borderline personality disorder or anxiety disorder based on clinical assessment scales (e.g., the Psychiatric Diagnostic Screening Questionnaire or PDSQ [164]) and formal clinical examination conducted by a licensed clinical psychologist, and facilitated by the Structured Clinical Interview for DSM-5 (SCID) [145]. Participants also experienced at least one hospitalization for the mental health condition. Informed consent was obtained from participants after describing to them the research study, type of data to be collected, policies for storage and use, clinical risk mitigation protocols, and clarifying that their relationship with the medical institution would remain unaltered whether they chose to participate in the study or not. Consented participants included 142 psychiatric patients diagnosed with schizophrenia, 106 diagnosed with mood disorders, and 6 with other mental health conditions (Table 1). To answer the RQs, in downstream analyses, we combine participants with schizophrenia, mood disorders, and other mental health conditions into a single study population. While the objective outcomes of recovery, such as time taken for remission of symptoms and probability of relapse, vary across these conditions, clinical literature suggests commonalities in subjective recovery and reintegration experiences like a growing sense of agency and autonomy, quality of life, peer support, greater participation in normative activities, etc. [40]. As a formative investigation into transitions around hospitalizations, we focus on understanding the subjective experiences of recovery and reintegration transitions, thus, we combined analysis across conditions. All data collected from these participants were de-identified and stored in HIPAA compliant secure databases and servers, which were located at the coordinating institution with access privileges limited to only the core project personnel.
Table 1.
Descriptive statistics of participants.
| Variable | Statistics | Distribution |
|---|---|---|
| Demographics | ||
| Age | Mean = 24.0, Median = 22.4, Range = (15.1, 60.7) |
|
| Gender | Male | Female (55% Female) |
|
| Race | Native American/Indian, African American, White, Other |
|
| Ethnicity | Hispanic/Latino | Non-Hispanic/Latino (85% Non-Hispanic/Latino) |
|
| Diagnosis | Psychosis, Mood disorders, Other disorders |
|
| Facebook data | ||
| #Posts | Mean = 2596.3, Median = 1471.0, Range = (0, 11018.0) |
|
| Duration (days) | Mean = 1025.16, Median = 730.0, Range = (1, 3287) |
|
| Medical data | ||
| #Hospitalizations | Mean = 2.3, Median = 2.0, Std = 2.14, Range = (1, 17) |
|
| Duration (days) | Mean = 15.5, Median = 11, Std = 13.7, Range = (1, 104) |
|
| Gaps (days) | Mean = 365.2, Median = 175.5, Std = 513.9, Range = (2, 4179) |
|
3.1.1. Facebook Data.
Upon informed consent, all participants were requested to extract and share their Facebook data archives. This Facebook data comprised activity traces on the platform, specifically data on friend requests, messaging, updates to profile fields, adding new photos/cover photos, sharing feelings via status updates, shares, likes, co-tagging, as well as the linguistic content of timeline posts (status updates) made by participants. Descriptive statistics of this data are shown in Table 1.
3.1.2. Medical Records and Hospitalization Data.
We also collected medical history for each participant (following consent and adoption of HIPAA compliant policies). This included primary and secondary diagnosis codes, the total number of hospitalizations and admission and discharge dates per each hospitalization event. Note that in this data a hospitalization typically indicated that the participant had spent at least one day (more typically up to 30 days) in an inpatient facility within the target healthcare system, because a licensed clinician had assessed a significant symptomatic exacerbation, or a risk of self-harm/suicide/homicide, that needed 24×7 medical care, and that was not addressable via adaptions to the patient’s existing treatment plan if any. Across all patients, the medical records indicated 346 overall hospitalizations for schizophrenia patients, 230 hospitalizations for mood disorder patients and 9 hospitalizations for patients with other mental health conditions with 2.3 mean hospitalizations per participant (median = 2.0, std = 2.14).
3.2. Curating Facebook Data around Hospitalization Events
The goal of this paper is to identify different journeys of people during life transitions around a psychiatric hospitalization, as observed and expressed on Facebook. In doing so, we note that not all hospitalization events will have similar experiences, even for the same individual. If psychiatric hospitalizations are considered major life transitions, the effects of each hospitalization as experienced by individuals might be different. Therefore, in this work, we consider each hospitalization event per consented participant as a different observation.
To gather Facebook data surrounding each hospitalization, we first collate the admission dates for all hospitalization events in each participant’s medical history. Using the hospitalization admission dates as temporal markers, we center the participant’s Facebook data such that the day of admission to the hospital is treated as day 0. Then we extend the temporal window before and after the hospitalization (day 0) and stop only when we reach another hospitalization admission for the same individual. Note that for a participant with only one hospitalization, we include their entire Facebook archive from the earliest to most recent date. We repeat this process for every hospitalization event recorded per participant. Across all 254 participants, we have a total of 584 recorded hospitalization events; however, only 372 hospitalizations had some digital traces from Facebook archives during that time. Corresponding to each of the 372 hospitalizations, we gather and center the participant’s Facebook data around their admission date. The distribution of the number of posts surrounding each hospitalization is shown in Figure 1. The average number of posts surrounding each hospitalization event is 3162.44 (median = 670.0, std = 8503.81). Across all hospitalization events, the minimum and maximum number of Facebook posts are 1 and 86,465 respectively.
Fig. 1.
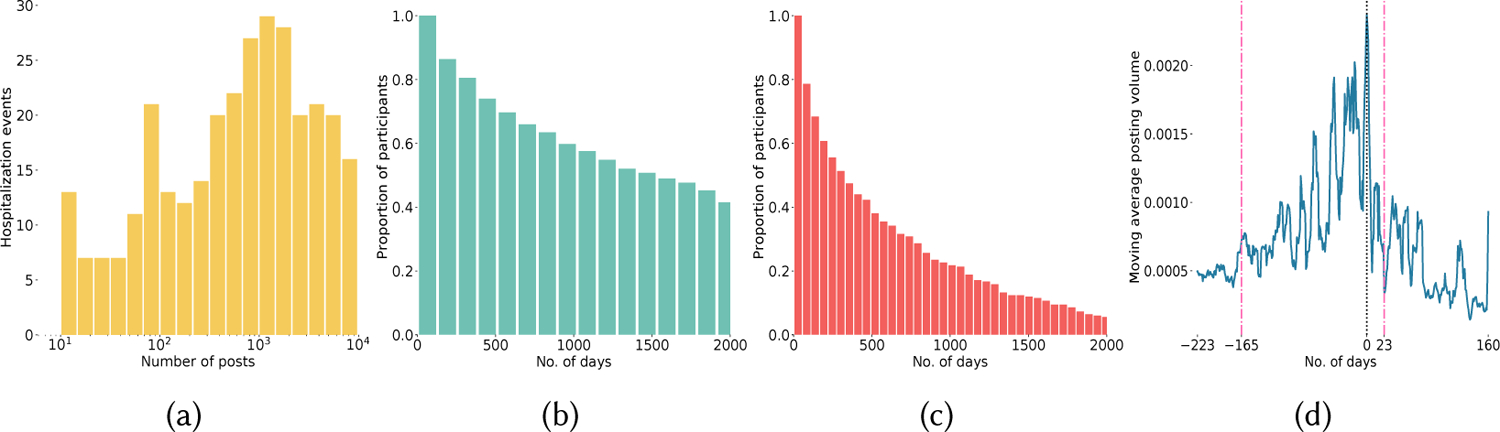
(a) Distribution of number of Facebook posts over hospitalization events (b) CDF of post distribution preceeding the hospitalization event (c) CDF of post distribution suceeding the hospitalization event (d) Temporal phases identified around the hospitalization using a moving average model of posting volume. The central vertical line indicates the hospitalization admission date, while the vertical lines on its two sides indicate the boundaries of the before and after hospitalization phases.
Next, to analyze data across all hospitalization events (which ranged from 2009–2019), we identify a fixed time period preceding and succeeding each hospitalization. We adopt an empirical approach by generating cumulative density functions (CDFs) of the number of posts1 before and after each hospitalization event. These CDFs are shown in Fig. 1. Based on these figures, we observe that most users (around 70–80%) have posts for at least 230 days before and 160 days after each hospitalization event. Therefore, we choose Facebook timeline data spanning 230 days before and 160 days after each hospitalization event as a fixed-length time period for downstream analyses.
4. CHARACTERIZING MENTAL HEALTH STATUSES AROUND HOSPITALIZATIONS
4.1. Theoretical Framework: Possible Selves
Corresponding to RQ1, our goal is to identify and understand patterns on Facebook that characterize peoples’ individualized mental health states around psychiatric hospitalizations. To do so, we adopt the Possible Selves framework [103], as introduced earlier. The possible selves concept is used in psychology to complement current conceptions of self-knowledge and to capture cognitive representations of alternative versions of the self in the future. In more detail, possible selves represent “individuals’ ideas of what they might become, what they would like to become, and what they are afraid of becoming, and thus provide a conceptual link between cognition and motivation” [103]. Possible selves are largely based on past experiences, but their essence lies in clear references to the future [103] – they are cognitive representations of hopes, fears, and fantasies regarding oneself. Thus, per the Possible Selves framework “an individual’s collection of self-conceptions and self-images can include the good selves (the ones we remember fondly), the bad selves (the ones we would just as soon forget), the hoped-for selves, the feared selves, the not-me selves, the ideal selves, the ought selves. They can vary dramatically in their degree of affective, cognitive and behavioral elaboration” [103].
As described in Section 2, we consider psychiatric hospitalizations to be major life transitions in an individual’s life. Psychotherapy research has argued that surrounding this liminality, it is important to consider the patient’s “possibilities” (i.e., the possible future states of the self) as an important instrument of effecting a change [80]. These possible selves can be understood as a kind of positive resource that the patient draws on when making desirable changes in their behavior or self-regulation to manage their underlying mental illness, around the hospitalizations. Prior clinical literature has studied individuals’ possible selves in relationship to their diagnosed mental health condition itself [31, 84, 87]. For instance, Janis et al. found that participants with borderline personality disorder were less likely than controls to endorse positive possible selves as current, but more likely to endorse negative possible selves as “current, probable, desired, and important” [87]. In [31], Clarke found that being positive about achieving possible selves was positively related to functional outcomes in first episode psychosis. We hypothesize that people’s language, behaviors and self-presentation signals surrounding hospitalization, as expressed on Facebook, may represent the various possible selves or “future-projected” aspects of self-knowledge, that they perceive as potentially possible.
Our rationale is grounded in the fact that existing behavior change theories (such as the Transtheoretical Model [128] or the Theory of Planned Behavior [4]), often used to capture health transitions (refer Section 2.3), have been criticized for their lack of adaptive capabilities as well as their inability to take into account an individual’s unique psychological state, social context, activity, and behavior patterns [77]. Furthermore, these models rarely match the reality of health transitions, due to differences between actual and perceived behaviors and assumptions related to homogeneity within behavioral change [127]. In contrast, our conceptualization of mental health statuses using the Possible Selves framework allows us to consider that the same individual can exhibit multiple possible selves on Facebook during a certain period before or after a hospitalization. Also, different individuals may express different possible selves on Facebook at any given time preceding or succeeding psychiatric hospitalizations because of their contrasting life situations. Finally, as one navigates the transition caused by the psychiatric hospitalization, these possible selves may evolve and change over time. In this paper, we refer to an individual’s diverse mental health statuses surrounding hospitalizations as a collection of their possible selves.
To operationalize and capture possible selves surrounding hospitalizations guided by this framework, we adopt the following empirical approach described in the remainder of this section.
4.2. Identifying Temporal Phases around Hospitalizations
Studying life transitions surrounding psychiatric hospitalizations necessitates identifying data spanning pre- and post-hospitalization phases where the self-presentation and behavioral changes are most likely to be manifested. Prior work in CSCW and HCI on behavioral changes during major life transitions found abrupt declines in posting activity on social media and noted it as a sign of social withdrawal [55]. For instance, in individuals challenged with postpartum depression, changes in sociality, and behavior on social media manifested through patterns of posting volume [41]. Other work has also noted a sudden increase in posting volume referred to as a “rush” of excitement for the future in the case of life transitions like engagement, starting a new job, or having a child [43]. Also, per clinical literature, we expect people to show markers of social withdrawal, which is known to be a notable risk marker around hospitalizations [97]. Therefore, we use measures of changes in posting volume of an individual (normalized number of posts per day) to identify temporal phases around psychiatric hospitalizations. Our phase identification approach is adopted from Ernala et al. [55] and includes the following two steps:
First, we calculate the daily posting volumes on Facebook timeline around each of the 372 hospitalization events spanning 230 days before and 160 days after the hospitalization. We computed the rates of change throughout the before and after hospitalization periods by employing a weekly moving average model on this posting volume time series data. This would allow us to smooth out local fluctuations and seasonality while allowing comparison between the posting volume at day t and that during the seven days preceding it.
Next, we compute the medians of the weekly rates of changes during the periods before and after hospitalization and use a median split method to define phase boundaries. Specifically, the first time point (day) in the pre-hospitalization data when the rate of change of posting volume becomes higher than the pre-hospitalization median rate of change is taken as a cutoff. Similarly, the first time point (day) in post-hospitalization data when the rate of change of posting volume becomes lower than the post-hospitalization median rate of change is taken to indicate another cutoff.
As shown in Figure 1, the median rate of change in posting volume pre-hospitalization was 0.0007 and 165 days prior to hospitalization (day 0) is the first time the rate of change surpassed this median. Similarly, the median rate of change in posting volume post-hospitalization is 0.0005 and 23 days after the hospital admission is when this rate is lower than the post-hospitalization median. Since the rates of changes in posting volume are computed weekly, we adopt the following day demarcations to define four temporal phases around hospitalization:
Bf_long or Long before hospitalization (N = 214): 223 to 165 days prior to hospitalization.
Bf_hosp or Before hospitalization (N = 271): 165 days prior to the hospitalization day.
Af_hosp or After hospitalization (N = 130): 23 days after the hospitalization admission.
Af_long or Long after hospitalization (N = 166): 23 to 160 days after the hospitalization.
Thus, segmenting each of the 372 hospitalization events into four phases, we obtain 781 phases.
4.3. Modeling Possible Selves Around Psychiatric Hospitalizations
Next, to define and identify people’s individualized mental health states, or their possible selves during the above identified four temporal phases surrounding psychiatric hospitalizations, we build a Gaussian Mixture Model [108]. This approach has been used in prior HCI research to capture the heterogeneity in people’s social roles and their evolution [159].
4.3.1. Gaussian Mixture Modeling Approach.
Gaussian Mixture Model (GMM) is a probabilistic model that clusters heterogeneous, multimodal data into a fixed number of coherent components [108]. Unlike traditional clustering algorithms like k-means that perform hard-clustering where each data point is assigned a single cluster, GMMs perform soft-clustering where each data point can belong to multiple clusters with different weights. Using the model we assume that each temporal phase surrounding hospitalization can be represented as a feature vector x having d behavioral features and there exists K components , one for each type of possible self status described by the features. Each of the K components ci is modeled using a multi-variate Gaussian distribution with an associated vector μi of average values for each feature x ∈ X. Each temporal phase is then generated from a mixture of these K components and co-variance (∑i), which gives the likelihood of each pair of possible selves. Mathematically, each temporal phase x is represented as a linear combination of these X Gaussians, with the probability function as:
| (1) |
Here, are called the mixing coefficients and denote the probability of each individual Gaussian. Learning a GMM involves learning the mean, co-variance and mixing coefficient of each Gaussian. We use a Gaussian Mixture Model to cluster the 781 temporal phases around hospitalizations into K components such that each component has its own single variance. Each component then describes a possible self status (PSS) representing common behavioral patterns seen across all observed patients and their Facebook data surrounding their hospitalization.
4.3.2. Operationalizing Linguistic and Behavioral Signals for the GMM Clusters.
Next, we propose a set of linguistic and behavioral signals that characterize individuals’ mental health status transitions. We operationalize these signals from Facebook data during each of the 718 temporal phases. Each temporal phase is represented by a d-dimensional feature (d = 43) vector x, consisting of features described in the following section. All feature values were converted to z-scores.
Psychological processes.
Affective measures that reflect one’s emotional response are expected to notably change around major life transitions [110]. We use affective words based on the Linguistic Enquiry and Word Count lexicon [151] (LIWC). We extract the normalized frequency of word occurrence in Facebook posts belonging to the following categories: positive affect, negative affect, sadness, anxiety, and anger. Cognitive measures also play an important role during transitions related to mental health by mediating the affective and attitudinal responses [18]. We calculate the normalized word frequency of the following LIWC categories in Facebook posts: insight, tentativeness, discrepancy, causation, certainty, differentiation.
Linguistic style.
The use of function words is known to provide a non-reactive way to explore social and personality processes [30]. We use LIWC to define linguistic style: personal pronouns (first-person singular and plural, second-person and third-person), impersonal pronouns, adverbs, auxiliary verbs, conjunctions, article, preposition, and negation.
Mental health related.
Beyond everyday activities shared on Facebook, individuals experiencing major life transitions such as a hospitalization are likely to share content specific to their experiences of symptoms of the condition. We adopt two sets of features to identify signals specific to the mental health symptoms and experiences. First, we use the LIWC measures related to health, sexual, body, and ingest categories to identify word usage around the specific health experiences. Second, we adopt validated machine learning classifiers of social media language indicative of depression, anxiety, stress, suicidal ideation, and psychosis from prior literature [135]. The classifiers have demonstrated linguistic equivalence across platforms and accuracy ranging from 0.82 to 0.92 (recall ranges 0.82 to 0.91 and precision between 0.85 and 0.92) on unseen test data in prior work. We ran these classifiers on Facebook timeline posts during each phase and calculated an aggregate proportion of posts that were predicted as indicative of different mental health concerns.
Temporal orientation.
Alongside affective, cognitive, and behavioral variations between an individual’s collection of self-conceptions, the theory of possible selves posits that they also vary in “tense” or “temporal sign” of the self, that is individuals holding notions of their past selves, present selves, and future selves [103, 142]. To capture the temporal signs in self-presentation on Facebook, we calculate normalized counts of word usage belonging to the following LIWC categories: focus on the past, focus on the present, and focus on the future.
Social and personal concerns.
The disruption caused by life transitions like mental health hospitalizations is often accompanied by stress [48]. The stressors brought about by mental health experiences are not only related to peoples’ psychological well-being but also their personal and social concerns such as work or employment [102], housing [5], social role changes and so on. To identify social and personal concerns during the phases surrounding hospitalization, we use the LIWC lexicon to calculate the proportion of words belonging to each of the following categories: home, religion, money, death, leisure, friend, and family.
Self-presentation on Facebook.
Transitions such as experiencing a psychiatric hospitalization involve people “redefining their sense of self and redevelop self-agency in response to disruptive life events” [52]. Identity work [111] and signaling social role changes [158] are important aspects of navigating such transitions. Drawing from literature of identity and major life transitions [137], we expect our participants to show changes in self-presentational signals on Facebook during the transitional phases surrounding hospitalization. To capture these signals, we measure the following assessment and conventional signals [49] derived from Facebook: updating profile fields, adding photos, adding cover photos, sharing feelings with status updates, and broadcasting behaviors using shares and likes on Facebook.
Social interactions.
Technologies like social media are known to play an important role during major life transitions by helping individuals establish a “new normal” [105], conduct identity work [111] and reach out to similar others [136]. Also, social functioning is a key marker for recovery in mental health conditions [14]. To capture aspects related to peoples’ social interactions and functioning during the temporal phases surrounding hospitalization, we consider the following features from Facebook data: number of friend requests sent or accepted on Facebook, one-one interactions measured via the number of distinct people with whom the participant shared messages, number of messages exchanged, number of posts where the participant was co-tagged with others, and an overall measure of posts and activities on Facebook.
4.3.3. GMM Parameter Tuning: Determining the Number of Components.
Training the GMM involves selecting the parameter K to indicate the number of components. We experimented with K from [2, 10] to empirically determine the optimal number of components/possible self statuses. To prevent over-tuning, we used the Akaike’s Information Criterion (AIC) and Bayesian Information Criterion (BIC) to determine the optimal fit. The lower the AIC and BIC values, the better the model is at predicting the underlying unknown distribution. Based on the values and the gradient of the AIC and BIC scores curve, we found that GMMs with K ∈ [4, 6] were a good fit on the phases data.
4.4. Clinical Validation and Grounding of the Possible Self Statuses: A Taxonomy
Validating the output of generative models like Gaussian Mixture Model components or Latent Dirichlet Allocation based topic models is typically done by human coding tasks [55], goodness of fit or predictive likelihood measures, performance on external tasks or validation of coherence [71]. However, qualitatively interpreting the derived components is challenging due to lack of contextual knowledge, difficulty in understanding the operationalization of features and researcher bias. Recent work has reflected on the convergence and divergence between statistical machine learning methods (especially unsupervised approaches) and grounded theory method [13] and suggests hybrid, iterative approaches that combine the two [13, 113] as possible alternatives. We take inspiration from this literature and prior work interpreting GMM components [159] to finalize the final setting of number of GMM components and their labels.
Using the approach in Section 4.3, we fit Gaussian Mixture Models for values of K that showed optimal fit based on the AIC, BIC scores. Then for each model’s extracted components, we find the top behavioral features that are representative of the component. To get the top features per component, we use two measures: 1) We take the feature means per component, which in the form of z-scores, shows whether the behavior was performed more or less than its average value. Based on the magnitude of z-scores, we filter the top features and their mean values per component. 2) We build a linear regression model on the probability of a phase belonging to the component and extract features that are statistically significant and predictive of membership to the component.
We presented the top features per component for each of the GMM models to 4 annotators and gathered their input to help interpret and name the extracted components as possible self statuses. To provide additional context for interpretation, we also provided them with the temporal periods during which the component was most prominent (for instance, whether most phases predicted to belong to a component were right before hospitalization). Using this information, we conducted individual semi-structured interviews and follow-up sessions with annotators to iterate over the component labels and reach the most theoretically grounded and clinically informed GMM setting that would capture the PSS surrounding the hospitalizations. The four annotators included one psychiatrist and two computer science researchers who were domain experts in mental health and social media studies and a graduate student familiar with the Facebook data. The first author conducted the sessions to iteratively build a shared vocabulary combining the annotators’ expertise in clinical care and behavioral analysis of social media data. Annotators compared different GMM model outputs based on the discernability of the components and whether the extracted components were comprehensive. Based on feedback from these sessions, we chose K = 6 as the final GMM configuration. Table 2 shows the names of the six PSS alongside the top representative features per PSS as well as example paraphrased Facebook posts, explaining the behaviors within the PSS. We used moderate levels of disguise [20] while paraphrasing posts in Table 2, i.e. identifying details (such as places) were changed and verbatim quotes were modified grammatically to safeguard privacy of participants. Fig. 2 shows the frequency of occurrence of each PSS in our data.
Table 2.
Derived possible self states (PSS) on Facebook surrounding psychiatric hospitalizations. The increasing behaviors indicate actions that are performed more as part of the PSS compared to its average level, while those decreasing indicate actions that are performed less as part of the PSS compared to its average level.
| PSS | Increase in behaviors | Decrease in behaviors | Example posts and behaviors |
|---|---|---|---|
| Self-regulation | Use of words indicative of positive emotions***. “I just wanted to say that everyone danced so well tonight. I really enjoyed the performance.” | All other actions. E.g., use of function words, pronouns, first-person singular pronouns, show focus on the present in language, post content indicative of mental health symptoms and experiences, use of impersonal pronouns, show focus on the past in language*, third-person plural pronouns, words related to anger, body, work, sadness, death, leisure*, words indicative of negative emotions**, words about friends*. “My roommate was watching OUAT, and I remember how quick Ruby was to condemn Regina” | “It is world humanitarian day. I’m doing something good, somewhere for someone else. Join me. #WHD2012 #IWASHERE” |
| Self-awareness | Use of function words, personal pronouns, first-person singular pronouns, words related to cognitive processes, first-person plural pronouns, words related to anger**, words related to money*, show focus on the present in language, show focus on the future in language*, posting content indicative of mental health symptoms or experiences. “I just can’t sleep, I watched American Horror Story for the whole day. I promised myself I would wake up early and clean my room” | Posts indicative of positive and negative emotions, sending messages to friends on FB, posting photos on FB, words related to leisure, one-on-one interactions on FB, words indicative of anxiety*, sharing feelings with status updates on FB**,shares on FB*. Number of FB shares relatively dropped by 100%. | “It’s just a slap in the face when you are your only sole motivation and advice giver… you have no one saying ‘keep going’, ‘i’m proud of you”‘, “You work hard on your mental health to the point your new psychiatrist doesn’t want you on meds anymore”, “Feeling accomplished and great”, “Hungry and bored again. blah!” |
| Sociality | Overall posts and activities on FB, uploading photos and cover photos on FB, sharing feelings via posts on FB, likes on FB, one-on-one interactions on FB, sending messages on FB, co-tagged with others on FB, use of informal words. Number of FB posts relatively increased by 341%. | Post content related to mental health symptoms and experiences, use of second-person pronouns, first-person plural pronouns, words indicative of negative emotions, showing focus on the past in language, use of words related to leisure, adding new friends on FB. “These winds are blowing down everything except the Trump tower” | “I have a lot of best friends lol so happy… national best friend day to everyone who are my best friend” |
| Withdrawal | No action. | Use of function words, pronouns, posting content indicative of mental health symptoms and conditions, posting content indicative of positive emotions**, use of person pronouns, showing focus on the present in language, use of first-person singular pronouns, anger, words related to body. “omg! You’ve got great hair styling skills sister.” | “[The user] went to [a certain music festival]”, “[The user] added education to his timeline”, “[The user] added [a city] to his current city” |
| Re-adjustment | Use of words related to leisure, sexual words, words related to work, ingestion***, pronouns, function words, informal words, co-tagging with others on FB, words related to anger, death, adding new friends on FB, use of words related to health***, showing focus on the past in language***, sending messages to friends on FB***, shares on FB***. “I’m on the verge of a manic episode. WHAT DO i DO?” | Only use of third-person singular pronouns. “Woot! commemorating my 7th good hair day in a row” | “Friends always: fight for you, include you, respect you… stand by you. People believe your actions more than your words”, “I am not my hair. I am not this skin. I am not your expectations. I am a soul that lives within”, “#oldclass-mates reunion”, “#fuckedup”, “#amen”. |
| Incoporation | Showing focus on the present in language*, words indicative of negative emotions***, posting content indicative of mental health symptoms and experiences, us of informal words**, function words, pronouns, sending messages to friends on FB, use of personal pronouns, first-person singular pronouns, words related to religion**, body one-on-one interactions on FB, use of words about friends***, health**, sharing feelings with status updates on FB***. “my girl.. I need your help pls get back to me as soon as possible” | Use of words indicating positive emotions, co-tagging with others on FB, overall posting and activities on FB, use of words related to anxiety*. “Aww! Thanks for the feel better card!” | “Anyone with a TV watching the movie Avengers I might be able to join?”, “Anyone coming from [a location] that might be able to give me a ride to [another location]?”, “Sorry I missed your show last night. Make sure you keep me posted with everything going on” |
Example increasing/decreasing behaviors for the same individual are indicated in blue.
All Facebook posts are paraphrased to protect participants’ privacy.
*** indicate p-values for behaviors that are predictive of membership to the PSS component.
p < 0.001
p < 0.01,
p < 0.05.
Fig. 2.
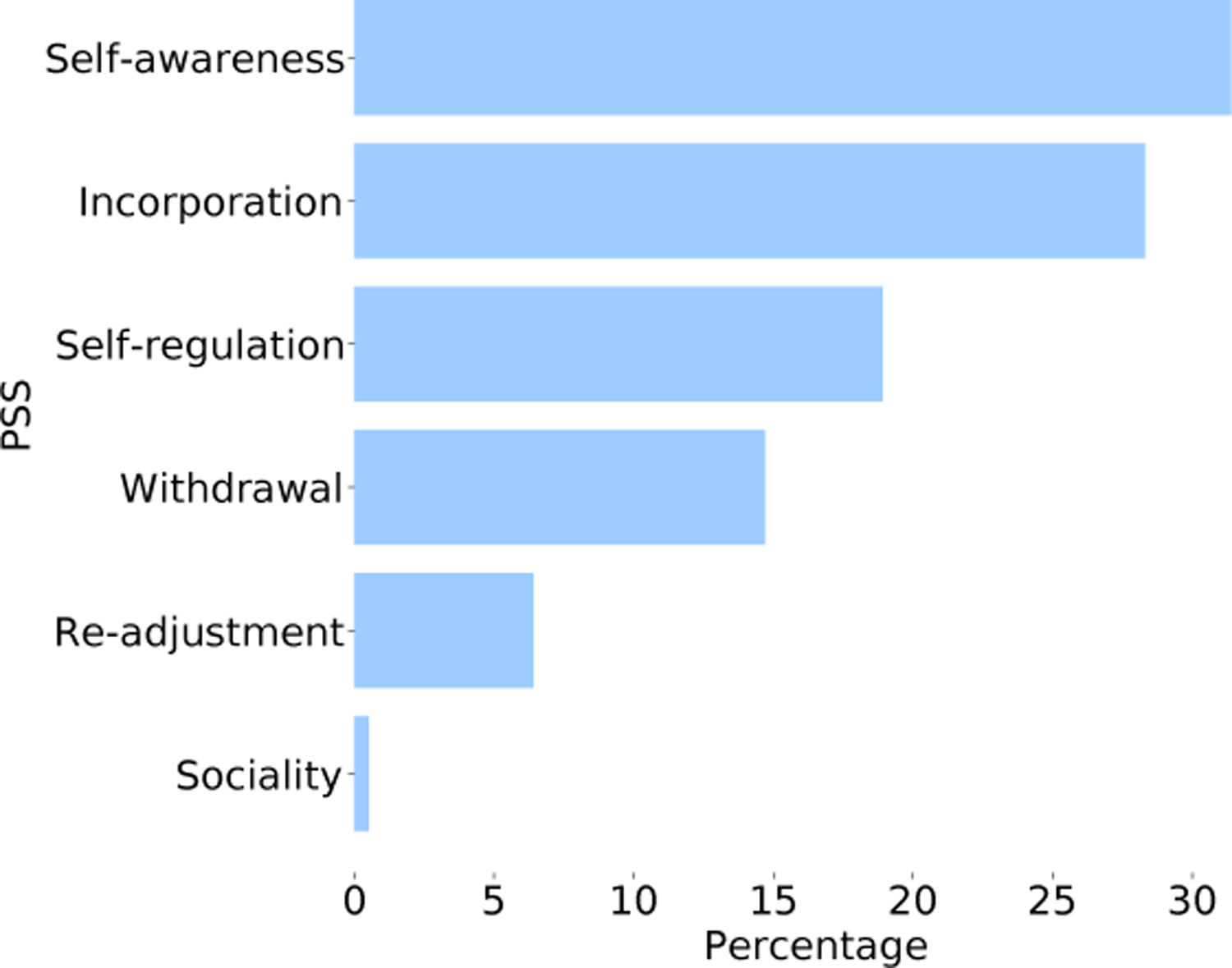
Frequency of the GMM-derived PSS
Self-regulation focused PSS: involving lower engagement, reduced posting, and activity signaling a detachment from the online social network with no indications of disclosure about their mental health status (indicated by lower use of pronouns). This PSS also suggests boundary regulation strategies [150] while only sharing positive content on Facebook. This PSS is seen most frequently during Bf_hosp and is presented with lower frequency during other periods.
Self-awareness focused PSS: involving high self-referential thinking and pre-occupation indicated by the increased usage of pronouns [1] and posting of content related to mental health symptoms and conditions. The higher use of words related to anger, work, and money and showing a focus on the present and future in language demonstrate an understanding of the transition and subsequent consequences. This PSS also has reduced social interactions and posting about emotional content. This PSS is most salient during Bf_hosp but also persists during Bf_long and Af_long indicating continued self-reflection surrounding psychiatric hospitalization events [126].
Sociality focused PSS: involving heightened sociality demonstrated by the greater volumes in posting status updates and photos, sending messages, one-on-one interactions, and other activities on Facebook. This PSS only appears during Bf_hosp.
Withdrawal focused PSS: involving an overall reduction in posting and activities on Facebook. As part of this PSS, people use significantly fewer function words and personal pronouns and reduce posting content indicative of mental health symptoms and experiences. The overall lack of activity and engagement shows that people are possibly withdrawing from the active use of social media. This PSS is most salient during Af_hosp.
Re-adjustment focused PSS: involving increased sociality, such as adding new friends, sending messages, and co-tagging others. But this PSS also reveals more self-attentional focus and expressive behaviors, shown by usage of words about anger, health, and death without inhibition. This PSS is most salient during Af_hosp and is less visible during other phases.
Incorporation focused PSS: involving the inclusion of experiences and narratives related to mental health transition into peoples’ online social lives. The increased use of emotional content and personal pronouns, showing a focus on the present and sharing content about their mental health status indicates self-focus, awareness and disclosure of experiences on Facebook. On the other hand, this PSS also shows signs of increased sociality demonstrated by messages shared and one-on-one interactions with others. This PSS is most salient during Af_hosp and persists with lower frequency before.
Fig. 3 shows a heatmap of membership probabilities of each PSS around the four periods surrounding the hospitalization. In essence, annotators found that the derived PSS captured the heterogeneity in peoples’ experiences along two main themes: symptomatic expression before hospitalization and social reintegration after hospitalization. Self-regulation, self-awareness, and sociality focused PSS that are most salient before hospitalization reveal different manifestations of peoples’ social media use and disclosure levels regarding their mental health condition online. While some people might choose to share their experiences related to mental health on Facebook (as in the self-awareness focused PSS), others might regulate and censor content regarding their mental health status transition (self-regulation focused PSS). This variability in social media use is also noted in prior work in people managing depression [56] and disclosures about schizophrenia diagnosis [54]. Our expert annotators also pointed out that the various PSS that are salient before hospitalization show varying levels of awareness and insights that people might have while experiencing mental health symptoms. For instance, during psychotic and manic episodes, that are most commonly experienced by individuals diagnosed with schizophrenia and mood disorders respectively (the majority of our study population), individuals are known to have distinctive levels of awareness, pre-occupation, and emotion regulation[24]. Annotators also identified the withdrawal, re-adjustment, and incorporation focused PSS that are most salient after hospitalization periods as different trajectories into social reintegration. While some people might withdraw themselves away from social technologies after discharge from the hospital to cope with the stigma and repercussions [69], others might increase activity on these platforms to get back to their online social lives and create a “new normal” [105].
Fig. 3.
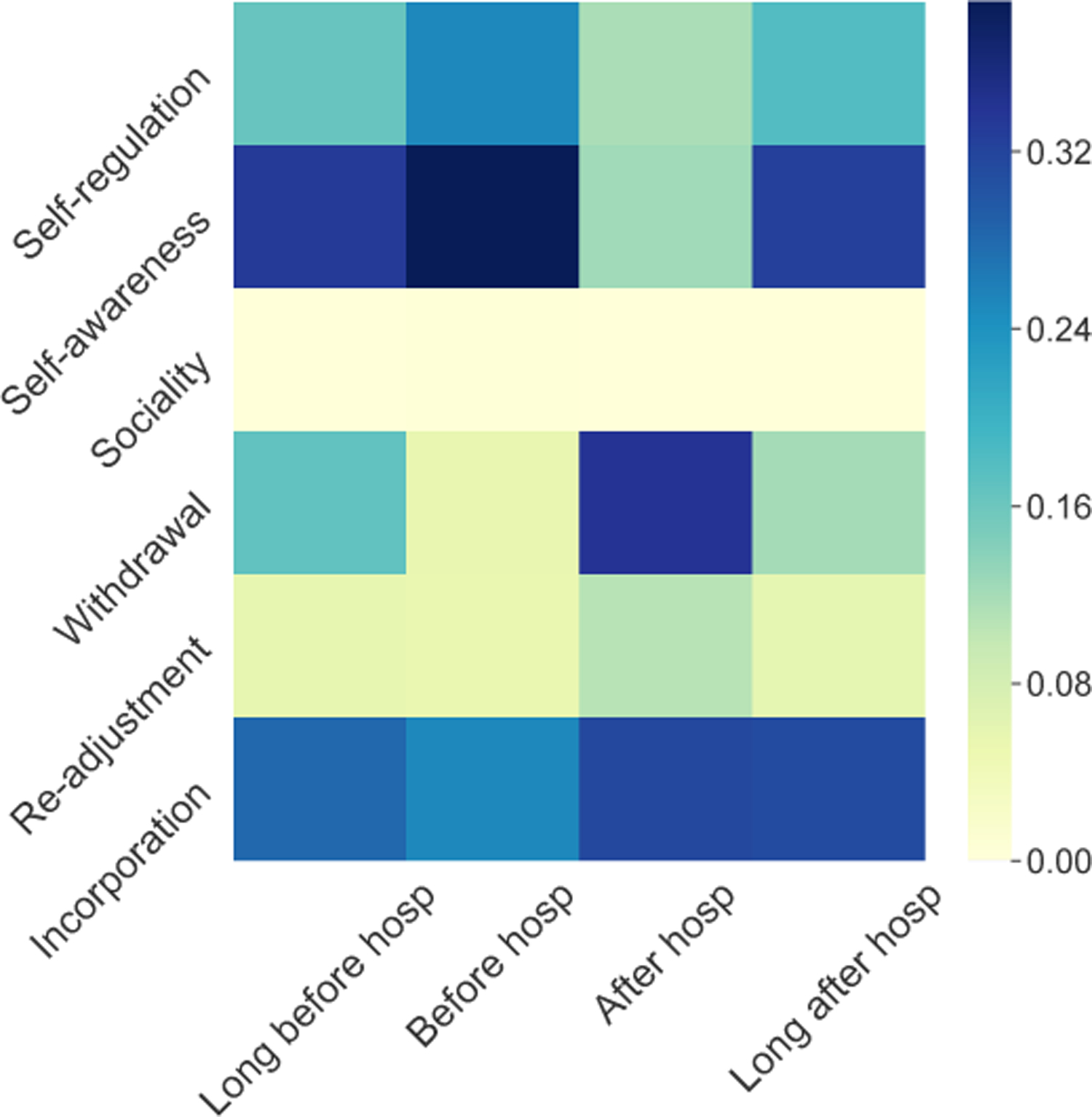
Proportion of each PSS in each temporal period surrounding the hospitalization events.
Although five of the six PSS occur with sizable frequencies, the sociality PSS occurs very infrequently. Examining the model, we found that the behaviors in this component were outliers and always captured as a separate cluster is all GMM models. We omit this PSS in subsequent analysis due to the infrequent occurrence and lack of discernable behaviors grounded in literature.
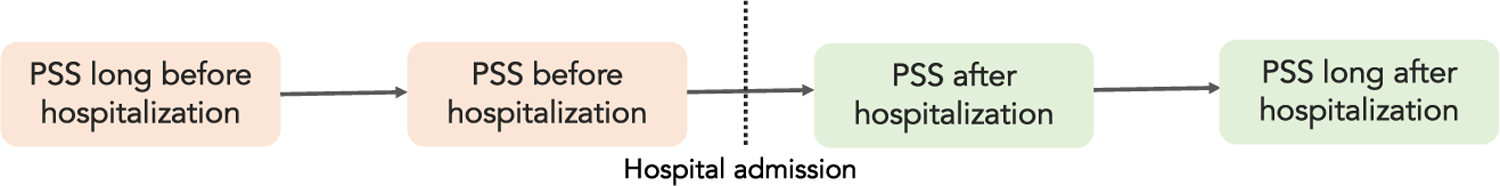
5. AN EMPIRICAL FRAMEWORK TO UNDERSTAND PSS TRANSITIONS
Per RQ2, we now study the different trajectories of transitions in PSS experienced by people surrounding psychiatric hospitalizations; for this, we use the above derived taxonomy of PSS. Prior work has noted that such transitions can be “complex, nonlinear, sometimes cyclical and potentially recurring” [92]. As an initial step, we focus on individual hospitalization events in a person’s entire journey with mental illness. We propose a framework that models linear transitions surrounding hospitalizations as a Markov process [53] with temporal chains generated to connect consecutive PSS (Fig. 4). Based on the temporal chains, we compute the transition probabilities, i.e., given a PSS is presented at time period t, the probability that the person would present any of the six PSS at time period t + 1. Here t indicates the four temporal periods surrounding hospitalization: long before (Bf_long), before (Bf_hosp), after (Af_hosp), and long after (Af_long). Each temporal phase is assigned a PSS if that PSS has the highest probability compared to others.
Fig. 4.
Temporal chains used to generate consecutive possible selves statuses for modeling transitions.
The top-10 likely PSS transitions across all four periods surrounding the hospitalization are shown in Fig. 5. First, we notice stability in the self-awareness (cond. probability = 0.48), self-regulation (cond. probability = 0.26) and incorporation focused PSS (cond. probability = 0.36), that are carried over from one temporal period to the next; those who present these PSS are more likely to maintain it in the future. The constancy in these PSS is also supported by the fact that self-awareness and incorporation focused PSS are the most common ones that people transition into – 37.5% of re-adjustment, 23.3% of self-awareness and 27% of self-regulation focused PSS transition into incorporation focused PSS, and 27.9% of incorporation, 23.9% of withdrawal and 28.1% of re-adjustment focused PSS transition into the self-awareness PSS.
Fig. 5.

Top 10 transitions between PSS that were likely to be seen around hospitalization periods.
Notably, those who exhibit the re-adjustment PSS have a conditional probability of 0.37, transition into the incorporation PSS. This transition shows individuals moving from a focus on the past to focusing on the present which is consistent with literature on major life transitions: reintegration is a process that first involves confronting life with the illness and then reconstructing life with the illness [93]. This transition also reflects a shift in boundary regulation practices [150]. While the re-adjustment focused PSS has heightened posting and activities on Facebook overall (every behavior is performed more than the average amount), people move past this PSS into the incorporation focused PSS which has moderate activity and posting on Facebook. Similar boundary regulation is also seen in people transitioning from the withdrawal focused PSS to self-regulation. Here, those who have completely disengaged from the platform (evident from the overall lower activity and posting), transition back into actively using the platform by posting positive content.
Next, we present a more in-depth analysis of transitions focusing on two important junctures around the psychiatric hospitalization. 1) The first involves recovery trajectories captured by the transitions from before to after the hospitalization (Bf_hosp to Af_hosp) revealing experiences related to clinical inpatient care. 2) The second centers around reintegration trajectories captured by those transitions that are from after to long after hospitalization (Af_hosp to Af_long) revealing experiences related to post-hospitalization social care and getting back to “normal” life outside of their clinical status. As noted in Section 2.1, a holistic understanding of clinical recovery and social reintegration is an essential aspect of understanding the mental health experience.
5.1. Using Possible Selves to Understand Recovery Trajectories
Fig. 6(a) shows the 10 most likely transitions seen around recovery trajectories i.e. the PSS exhibited before a hospitalization to the PSS exhibited after the hospitalization. First, we see stability in the presentation of withdrawal and incorporation-focused PSS; those who exhibit these PSS Bf_hosp are likely to maintain it Af_hosp. The stability of this PSS is also confirmed by the fact that withdrawal and incorporation focused PSS are the most common trajectories we see Af_hosp – 48.3% of self-regulation, 31% of incoporation and 28% of self-awareness focused PSS Bf_hosp transition into withdrawal focused PSS, and 56% of re-adjustment and 30% of self-awareness focused PSS transition into the incorporation focused PSS Af_hosp.
Fig. 6.
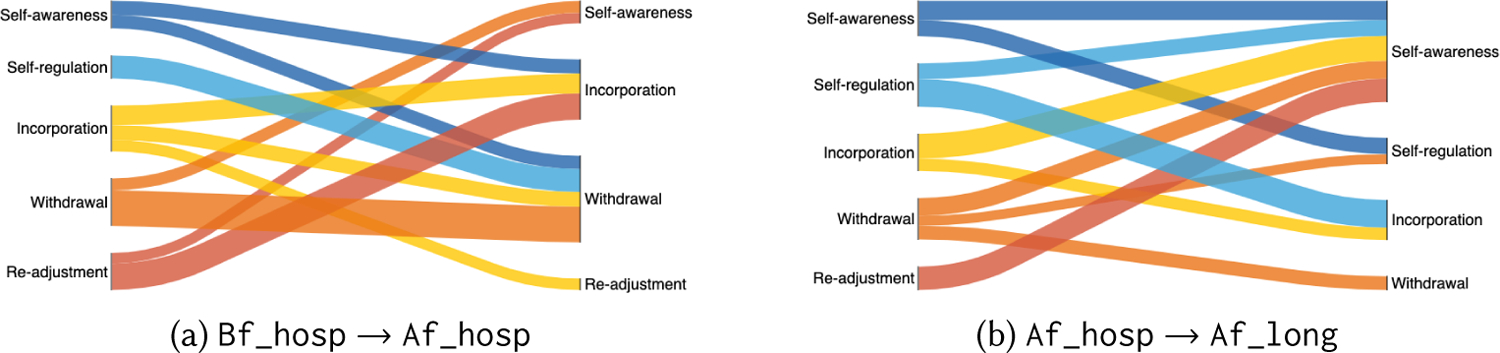
(a) Top 10 transitions between PSS likely to be seen around recovery i.e. transitions from Bf_hosp to Af_hosp. (b) Top 10 transitions between PSS likely to be seen around reintegration i.e. transitions between Af_hosp and Af_long. Nodes indicate PSS and width/thickness of the flow is proportionate to transition probability.
However, there is a difference between transitions that end in withdrawal focused PSS and those that end in the incorporation focused PSS. This depends on the whether the event was the first hospitalization experienced by the individual. Considering only those who have portrayed the incorporation focused PSS Bf_hosp, 66.6% of the transitions from incorporation to withdrawal focused PSS are seen during the first hospitalization events experienced by people. On the other hand, the majority of the cases where individuals remain in the incorporation focused PSS before and after the hospitalization (58.3%) are observed during subsequent hospitalizations (like the 2nd, 4th, or 5th hospitalization recorded for the individual). This reveals that while those who have been re-hospitalized can maintain an incorporation focused PSS, the first hospitalization experience leaves most people transitioning into the withdrawal focused PSS. This could be attributed to the stigma, isolation, or “other”-ing experience related to first time psychiatric hospitalizations [112]. This finding is also consistent with prior literature on mental health care that suggests that negative experiences associated with the first psychiatric hospitalisation remains significant even after many years have passed [3]. In a focus group study with participants from 6 countries, Ådnanes et al. note that psychiatric rehospitalizations encompassed some amount of familiarity; however, participants described the first hospitalization as “something shocking, intolerable, and terrible” [3]. For example, consider participant A whose recovery transition showed to shift from a self-awareness focused PSS to a withdrawal focused PSS after their first hospitalization. Participant A posted 15 status updates on Facebook during the two weeks prior to their hospitalization, such as the following paraphrased posts: “Live as if you were to die tomorrow and learn as if were to live forever; The only competition you’ll ever face is with your own ignorance.” However, since their hospitalization A made no posts on Facebook, except accepting new friends requests. In contrast, consider participant B. Around their fifth hospitalization B showed a recovery transition from re-adjustment focused PSS to reintegration focused PSS with paraphrased posts such as “Don’t lend people money because that person might be a *** and not pay you back.” before hospitalization to posts such as “my brother..the love we share is eternal. You live on in your loved ones memories and hearts.” after hospitalization.
5.2. Using Possible Selves to Understand Reintegration Trajectories
As a second deeper dive into recovery trajectories, Fig. 6(b) shows the top 10 transitions that begin after the hospitalization and end long after the hospitalization. The post-discharge period after hospitalization involves a shift in focus from institutionalized treatment, to coping and management of illness. This transition is accompanied by mechanisms to break inhibitions and stigma, open up about their experiences with intimate others, reach out for social support and improve overall well-being [78]. The two most common trajectories we observe during the post-hospitalization period end in the self-awareness or incorporation focused PSS. While both of these PSS involve self-referential thinking and self-reflection, only the incorporation focused PSS shows signals of social functioning (such as messaging friends, one-on-one interactions, co-tagging, etc.) that are considered positive signs of reintegration. Among people who transition into the incorporation focused PSS, 53.8% transition from the self-awareness focused PSS, and 24% are those who have maintained the incorporation focused PSS. Studies from the psychiatry literature report that the stigma related to hospitalization could be transitory in cases where people resume occupancy of normal societal roles [68]. This suggests that the transition from self-awareness focused PSS to incorporation PSS is a positive reintegration trajectory where people move past the uncertainty post-hospitalization and re-establish their online social connections as part of the incorporation-focused PSS.
Next, we find that every PSS exhibited immediately after the hospitalization (Af_hosp) has a transition ending in the “self-awareness” focused PSS long after the hospitalization (Af_long). While self-focus demonstrated by the awareness focused PSS is beneficial, excessive self-reflection is considered a central feature in mood and anxiety disorders [118], and greater focus on self-concept is also related to internalized stigma in mental health [99, 147]. In contrast to the social stigma about mental illness that entails discrimination, negative stereotypes, loss of opportunities, etc., self-stigma relates to awareness, agreement, and application [37] – a person with mental illness must first be aware of corresponding stereotypes before agreeing with them and then apply self-stigma to one’s self. A behavioral consequence of self-stigma is social avoidance [37, 100], that is the person may avoid situations where they might feel publicly disrespected because of self-stigma and low self-esteem. Awareness, reflection and social avoidance that are related to self-stigma are representative features of the self-awareness focused PSS, that most individuals are found to transition into long after hospitalization (Af_long). Based on this literature, the majority of reintegration trajectories we see ending in the self-awareness focused PSS might be reflective of the long term self-stigma, that happens as a consequence of psychiatric hospitalizations. For instance, participant C who transitioned into a self-awareness focused PSS long after their hospitalization posted on Facebook about the stigma they have been experiencing, saying (paraphrased): “I think the stigma about mental health really needs to be broken. I’m tired of every single person treating me like the plague. For the last year, I have been dealing with bi polar disorder. It was the scariest thing I ever dealt with but I learned that I’m not alone. People automatically treat you like your a different person, but don’t show me your sympathy. Treat me the same. I’m stronger than I’ve ever been.”
6. PREDICTIVE FRAMEWORK TO ASSESS REINTEGRATION
Given the importance of reintegration from both clinical and social perspectives (Section 2.3), in this section, per RQ3 we set up a prediction framework to assess how individuals reintegrate after psychiatric hospitalizations. By doing so, we demonstrate the utility of the taxonomy of PSS (RQ1) and the empirical framework capturing their transition trajectories on Facebook (RQ2).
We consider the incorporation focused PSS, which involves narratives related to mental health and people re-establishing social interactions after hospitalization, as a PSS-based operationalization of social reintegration. To examine the relationship between PSS trajectories and reintegration post-hospitalization, we consider models regressing on the probability of the phase long after hospitalization (Af_long) being predicted as the incorporation focused PSS by the GMM model. We choose Af_long as the focus of prediction, as we expect reintegration to be the final stage of mental health transitions experienced by the person. As covariates, we include the behavioral signals from the preceding phases (ref. Section 4.2.2), such that the model reveals how PSS-based behavioral signals in the past (before and after the hospitalization2) predict the probability of reintegration in the future (long after hospitalization or Af_long). We standardize all covariates and use the variance inflation factor (VIF) to eliminate multicollinearity. The dependent variables i.e., probability of belonging to the incorporation-focused PSS are log-transformed.
We consider several non-linear (decision tree regressor) and linear regression models with regularization (Lasso, Ridge and Elastic Net) and use grid search for parameter tuning. We use k-fold (k = 10) cross-validation approach to iteratively train the model and predict on held-out data. We collate the predictions, and obtain the pooled model performance measures – including Pearson’s correlation r and Mean Square Error (MSE) to evaluate predictive accuracy and R2 value to evaluate the model fit. For model performance comparison, we consider two baselines: first, an intercept only model (Null), which assumes a constant probability of reintegration irrespective of the covariates. As a second baseline (M_Hosp), we consider the probability of reintegration based on the likelihood that a person has exactly one hospitalization. This model assumes that a lack of re-hospitalization indicates successful reintegration. We regress covariates on probability = 1, for those with no re-hospitalizations based on medical records (and probability = 0 for those with re-hospitalizations).
Table 3a shows summaries of the best performing models. We find that the Ridge regression model has the best performance compared to other models. Compared to the Null model, the Ridge model provides considerable predictive power (shown statistically significant based on χ2 tests on model performance on held-out data). To reject the possibility that the performance of the Ridge model is by chance, we run permutation tests [6] to reject the null hypothesis that a randomly generated vector of reintegration probabilities will perform better than the Ridge model. We run 10,000 permutations of randomly generated dependent variables, and find that the probability (p-value) of improvement by a randomly generated vector is 0.003. This rejects the null hypothesis and reveals statistical significance in the observed improvement by the Ridge model.
Table 3.
(a) Summary of regression models. Null is the intercept-only model, the first baseline. M_Hosp is the second baseline deriving reintegration probabilities based on evidence of a future re-hospitalization. All comparisons are made with the Null model. p-values reported at p < 0.01. (b) Summary of covariates of best performing Ridge regression model on reintegration. p-values use Bonferroni correction
| Ridge | Lasso | D Trees | M_Hosp | Null | |
|---|---|---|---|---|---|
| Pearson’s r | 0.46 | 0.29 | 0.38 | 0.05 | <0.01 |
| MSE | 0.08 | 0.12 | 0.09 | 0.16 | 0.12 |
| R 2 | 0.35 | 0.19 | - | 0.20 | - |
| χ 2 | 82.80*** | 34.13 | 6.77 | 20.03 | - |
| (a) | |||||
| Covariate | Estimate |
|---|---|
| LIWC Category: Negative affect | 0.06* |
| LIWC Category: 1st P Sing Pronoun | 0.23** |
| LIWC Category: 2nd Person Pronoun | 0.18*** |
| LIWC Category: 3rd Person Pronoun | 0.16** |
| LIWC Category: Temporal Focus, Past | 0.05* |
| Facebook: Photos Shared | −0.06* |
| Facebook: Number of Shares | 1.35** |
| LIWC Category: Certainty | 0.12* |
| LIWC Category: Differ | −0.1* |
| (b) | |
p < 0.05
p < 0.01
p < 0.001
Next, we present findings about the most predictive covariates from a Ridge regression model,3 ref. Table 3b. First, sharing content that is emotional (negative emotion, estimate = 0.06**) and personal, including personal pronouns like ‘i’ (1st person singular, estimate = 0.24**), ‘you’ (2nd person, estimate = 0.18***), and ‘they’ (3rd person, estimate =0.16**) during the periods before and after hospitalization is predictive of reintegration long after hospitalization (Af_long). This finding is reflective of literature from the expressive writing paradigm that observed long term benefits of expressive writing in the form of both health outcomes (less stress related visits to the doctor, improved mood, lowered blood pressure, fewer post-traumatic intrusion and avoidance symptoms [123]) and social/behavioral outcomes [11]. Recent work has also revealed how social media is increasingly appropriated for sensitive disclosures related to mental health to obtain support and therapeutic benefits [55]. Although the level of disclosure might vary in our patient participants’ social media data compared to explicit, public disclosures of mental illness [54], we find that expressive behaviors on the platform are associated with reintegration. Next, we find that showing a focus on the past in posting language (estimate = 0.05*) during the hospitalization, is predictive of reintegration long after hospitalization (Af_long). Drawing from the Possible Selves framework [103], an emphasis on the past-selves could indicate a focus on getting back to what was “normal” in the past and creating a “new normal” after the transition due to hospitalization. Finally, certainty word usage (estimate = 0.12*) around the hospitalization, demonstrates heightened emotional stability and is predictive of reintegration after hospitalization.
We finally ask the question: what are the differences between those who show high reintegration signals on Facebook and those who do not? For this, we conduct post-hoc Kruskal Wallis and Mann Whitney tests to examine feature means between the two groups. We split observations into low and high reintegration based on the probability of belonging to the incorporation focused PSS being greater than chance (probability by chance is one in six PSS = 0.16. High reintegration = p > 0.16 and low reintegration = p < 0.16). Table 4 shows the statistically significant differences between the two groups. Those who have a higher likelihood of reintegration display more negative emotion and share content related to religion more than those who have a lower likelihood. Disclosure, emotional support, and faith are known to act as buffers against negative effects of stressful life events, which likely help with coping and reintegration after the event [33]. We also find that those who show reintegration signals stay in touch with friends on Facebook via messages. In contrast, those who reduce interactions via messages are less likely to show reintegration signals.
Table 4.
Differences in features between those who show high vs. low likelihood of reintegration. Reported measures are mean feature values per group, Kruskal Wallis test statistic H, Mann Whitney test statistic U, and effect size (Cohen’s d). p-values use Bonferroni correction
| Feature | Low | High | Kruskal Wallis H | Mann Whitney U | Cohen’s d |
|---|---|---|---|---|---|
| LIWC Category: Negative Affect | −0.13 | 0.05 | 7.93*** | 2226.5*** | −0.32 |
| LIWC Category: Home | 0.14 | −0.02 | 3.98* | 2449* | 0.10 |
| LIWC Category: Religion | −0.06 | 0.29 | 4.60* | 2405.5* | −0.38 |
| Facebook: Updates to Profile Fields | −0.05 | 0.02 | 6.67** | 2337.5** | −0.33 |
| Facebook: Number of Messages Shared | −0.16 | 0.05 | 3.94* | 2452* | −0.31 |
| Facebook: Number of Likes Received | −0.04 | −0.02 | 2.55 | 2576.5* | −0.05 |
| Facebook: Number of Shares | −0.06 | −0.05 | 3.77* | 2516* | −0.31 |
| LIWC Category: Negation | −0.07 | 0.02 | 2.48 | 2568* | −0.16 |
p < 0.05
p < 0.01
p < 0.001
7. DISCUSSION
7.1. Theoretical Implications
Anchoring on psychiatric hospitalizations as a liminality, in this paper, we combined clinical perspectives – around symptomatic expression and recovery, with social perspectives – around stigma and reintegration. Guided by the Possible Selves framework [103], we provided an empirically derived taxonomy to represent and then understand individuals’ mental health status transitions. Our approach thus enabled incorporating people’s heterogeneous experiences around recovery and reintegration in the computational modeling of mental health. By combining the two perspectives, we presented an exploration of the intersection and the significance of considering social and clinical perspectives on mental health. This illuminates important theoretical implications.
As noted in Section 2.2, computational approaches to study mental health within HCI, digital psychiatry, and machine learning frame the individual in two broad, distinct ways: as a patient who is receiving clinical care and institutionalized treatment for a validated diagnosis [15, 43], or as a vulnerable individual who is seeking social care and support for management of a mental health condition, such as from their networks of loved ones and peers, offline and online [7, 8, 119]. The word patient comes from the Latin “patiens,” from “patior,” meaning to suffer or bear. Scholars have expressed criticism of this conceptualization. It tends to objectify the person with mental illness [116], disregards their sufferings and identity outside of the clinical definition of the illness [85], and fails to consider the challenges people need to overcome beyond symptom management to get back to life following hospitalizations [129]. In contrast, when the clinical facet of one’s mental illness trajectory is ignored only to consider their vulnerability and self- and peer-supported management efforts, this latter conceptualization fails to account for the obstacles an individual faces in navigating a formalized treatment plan in concert with their own attempts. Research has shown that in some cases this lack of consideration of the relationship of social and clinical care can interfere with evidence-based treatment, create tensions in the patient-provider alliance, and even lead to detrimental mental health outcomes [117].
The repercussions of this disjoint consideration have been noted in recent social computing literature [60]. Chancellor et al. highlighted that the representation of people’s experiences and data in machine learning work on mental health – as a patient, disorder, data point or a person – may inadvertently risk dehumanization, poor and incomplete characterization of the mental health experience, and present serious consequences to scientific rigor [26]. Relatedly, as also mentioned in Section 2.2, Ernala et al.’s triangulation study on methods for predicting mental health states from social media data surfaced the differentiating uses of social media for mental health, showing that representations of people’s experiences who make disclosures on social media and seek social support for mental health, poorly generalize to those of patients receiving clinical care [54]. At the crux of these observations is the fact that peoples’ mental health statuses and needs are not isolated, discrete attributes, but are temporally situated experiences of the same person who is in transition, given the dynamic nature of their illness.
Framed in terms of Van Gennep’s liminality [154], using our derived taxonomy of PSS, we could examine the transitions of individuals as they enter and leave the role of a patient (Section 5). For example, an individual could move from the self-regulation focused PSS they expressed as a non-patient before hospitalization, to the withdrawal-focused PSS post-hospitalization, that is reminiscent of them being a patient at the hospital facility. Our taxonomy could further reveal the transitions that are indicative of reintegration after psychiatric hospitalizations (Section 6), such as those shifting from the self-awareness PSS immediately after they were a patient, to the incorporatation-focused PSS in the longer-term, as a way to embrace the non-patient identity again. This way, we showcased how a holistic view of an individual’s mental health state, as indicated in their clinical recovery and social reintegration can be derived by understanding their various possible selves surrounding hospitalizations. We did so by demonstrating a theoretically- and clinically-grounded computational approach that amalgamates insights from people’s medical histories as well as their social media data.
Drawing upon our work, future research leveraging digital traces for prediction of mental health states can benefit from noting that people’s mental health statuses and their exhibition on social media are heterogeneous, and contextualized within the individuals’ specific needs for clinical treatment and social support. Multimodal approaches, like Gaussian Mixture Models [108], that we adopt in RQ1, when formulated with theory (such as the Possible Selves framework [103]) and punctuated with clinical insights (Section 4), can reveal differentiating patterns of behaviors and use of social media within the same population. This way our work contrasts the theoretical models used to understand health transitions in prior CSCW research [101], which consider that the experiences of all individuals across the illness journey are the same, and that these transitions are largely uni-directional and permanent. Adopting a personalized approach, our taxonomy gives three distinct sets of behaviors that are dominant before psychiatric hospitalization – self-regulation, self-awareness, and sociality focused PSS. These characterizations of mental health statuses can enrich personalized predictive models for early interventions that consider an individual’s clinical as well as social pathways of care. Similarly, research primarily focusing on social support mechanisms for mental health could leverage how clinical aspects to care such as hospitalizations, medication adherence etc. impact support outcomes. For instance, in this study our proposed empirical framework of transitions revealed that first hospitalization experiences lead most people to transition into the withdrawal focused PSS, whereas those re-hospitalized are able to maintain the incorporation focused PSS. The support seeking goals and outcomes for the former group might be significantly distinct from the latter – insights that could contextualize how different individuals use of social media to find help and advice around their mental distress.
7.2. Clinical Implications
The taxonomy we discovered for RQ1 (Section 4) on distinct PSS, the empirical framework in Section 5 to capture mental health status transitions from RQ2, and the predictive models to assess recovery and reintegration in Section 6 (RQ3) can be useful to improve patient-provider interactions in treatment and management of mental illnesses. We discuss two such opportunities below.
7.2.1. Post-discharge care and support.
How one manages their illness outside of institutionalized clinical treatment strongly impacts both future clinical outcomes and overall well-being [78, 90]. But after discharge from the hospital, clinicians often lose timely contact with their patients which present challenges for continued care and support [91]. Even when patients adhere to clinical followup appointments, the emphasis is on treatment of symptoms and managing medication use and adherence, rather than on improvement in social well-being of the individual [2]. Clinical studies have highlighted the importance of social reintegration and community participation in avoiding re-hospitalizations and supporting the clinical goals of recovery [2]. However, reintegration is a complicated phenomenon to identify and existing instruments and validated measurements are limited [82]; often they are specific to the domain being investigated (such as incarceration [70], refugee migration [25] etc.). Importantly, reintegration in mental illness is poorly understood for the reasons above. The predictive assessment of reintegration from RQ3 revealing likelihood of reintegration after hospitalization can help clinicians better understand the outside-hospital, post-discharge experiences of people. Especially for young adolescent populations, who are one of the most affected demographic with mental disorders [61], social media is a significant part of their identity and social lives [125]. How people re-establish their online presence and social connections after stigmatizing hospitalization events can act as collateral information [124] for follow-up during clinical sessions, discharge practices and community care. Future work can conduct interview studies to get deeper insights into how social technology use supports (or challenges) people in reintegrating back to their lives after major transitions such as psychiatric hospitalizations.
7.2.2. Sensemaking in health care settings.
Making sense of health status transitions is of critical importance for people who are dealing with life disruptions, such as health-related challenges [62]. Clinical research suggests that individuals involve in a “laborious sense-making activity” to “create a new link between past, present, and future” [23] in their search for normality and self-regulation [23]. Godbold et al. [66, 67] found that people with compromised health bridged information gaps by orienting themselves to repeated themes and to notions of what is “normal” among a group of peers. Accordingly, the taxonomy and findings from RQ1 demonstrate how people’s embodiment in a combination of possible selves statuses surrounding psychiatric hospitalizations can act as new information in discursive therapy sessions and help in sensemaking of hospitalization experiences. Drawing from work in personal informatics and self-reflection [96, 114], the extracted PSS can act as questions that people pursue about their data to maintain awareness of their status relative to a goal (like social functioning or reintegration), or even for the purpose of self-experimentation to examine the efficacy of current treatment strategies. The Possible Selves framework [103] is also known to elicit behavioral change and has been adopted in psychotherapy [12], because the very conceptualization process of possible selves may lead the way toward more planned and intentional interventions. Supported by our taxonomy of PSS transitions, clinicians and therapists can encourage patients to discuss their recovery and reintegration trajectories. For instance, if a person was transitioning into a withdrawal-focused PSS in the long term (indicating an overall reduction in activity and engagement with others) clinicians can encourage them to discuss and address any challenges to social reintegration they might be facing after hospitalization. The derived transitions between PSS from RQ2 can further act as a component through which self-motivation and self-knowledge are influenced [80] in clinical care settings – after all, the essence of sensemaking for an individual with mental distress is often to embrace a positive change.
7.2.3. Ethical implications.
The introduction of insights from social media data into clinical settings, as discussed above, requires careful consideration of ethical implications concerning privacy, ethics, consent and clinical responsibility. First, consent procedures would not only need to include privacy and confidentiality with respect to data collection and data use, but also the clinical settings (in-patient, out-patient, therapy sessions) in which social media data might be incorporated. To elucidate this information, more research is needed from interdisciplinary teams of clinicians, researchers and patients to understand the efficacy and potential outcomes of introducing social media data into clinical contexts. When to seek consent from participants managing mental illness is also important. In this study, clinicians assessed potential participants’ symptomatic conditions before reaching out regarding study participation. Participants should also be given an option to opt-out of research programs without any consequences to their ongoing treatment and care at the facility. Lastly, the data used in this study were obtained from consenting participants who were fully informed of the risks and benefits of participation. For future work, the potential for this information to reveal sensitive clinical insights may motivate other parties to collect and analyze it without consent. Thus, it is important for clinicians and researchers to develop standards to protect the confidentiality and the rights of this sensitive population to avoid misuse of personal information and to maintain individual autonomy.
7.3. Design implications
7.3.1. Designing for online social reintegration.
In our work, we found evidence suggesting that Facebook can act as space for online social reintegration for individuals transitioning around psychiatric hospitalizations. Findings from RQ3 showed that emotional and personal sharing around hospitalization is predictive of reintegration in the future. Those who show a high likelihood of reintegration stay in touch with friends via messages more so than those who do not show these signals. So how can we design social media to support peoples’ reintegration journeys? Extensive literature shows that social media use is associated with social capital gains – both bonding capital in the form of emotional support received from strong ties [50], and bridging capital in the form of new information received from weak ties [130]. Social capital benefits are immensely helpful to individuals during post-hospitalization periods. Strong ties can provide relationship maintenance benefits [51] and emotional support [156] after the psychiatric hospitalization. Weak ties can similarly be helpful. Regaining employment, access to new information and resources, support for health-related stigma and community support are all important factors that support reintegration journeys that weak ties are known to provide [22, 39]. Consistent with prior work on identity transitions [73], we found that social media enables people to embody multiple, heterogeneous possible selves surrounding hospitalization. Prior work suggests that individuals attempt to manage the link between their previous and current identity by editing self-presentational data, and the configuration of the network itself [75]. In the case of transitions surrounding hospitalization, individuals may wish to draw on social capital benefits discussed above from a selective set of Facebook friends, while not disclosing to others on their network. They might embody multiple PSS, say both incorporation-focused and withdrawal-focused PSS after hospitalization. How can we design social media to support selective presentation of the PSS to different audiences? To support this multiplicity, it will be helpful if platforms provided better controls for audience segmentation and selection [143], so that the multiple possible selves can be presented to appropriate audiences without inhibition and negative repercussions like context collapse or compromised privacy.
Our findings in this paper are based on Facebook, one of the most widely used social media platforms that supports connections to people one knows in the offline context [50]. Other social media platforms with affordances for anonymity (like Twitter or Reddit) may also support disclosure of sensitive, personal topics about individuals’ mental health transition experiences [42]. Online mental health communities play a role in help-seeking behaviors and connections to other individuals with similar conditions and experiences [115]. Similarly, technology-mediated communication via SMS or phone calls may also characterize mechanisms for getting back to social lives after hospitalization. The social networks and the benefits that people draw across various social media and technology-mediated communication platforms are varied. How can we understand these contexts together and the role they play in supporting social reintegration for mental health? Future work can combine social and behavioral traces across these contexts with qualitative insights from hospitalized individuals to inform the design of new systems supporting social reintegration. Such future systems can potentially serve as reintegration resources to individuals after hospitalization, similar to rehabilitation programs [138].
However, we note an important caveat in these design suggestions. Unlike other life transitions such as parenthood [64] or gender identity transitions [74], transitions of mental health statuses could be cyclical or non-linear, rarely unidirectional, or permanent. Relapse and re-hospitalizations are exceptionally common for the conditions we study in this paper, like schizophrenia and mood disorders [133]. Therefore people undergo multiple transitions and possibly return to past selves several times along the course of the illness; this is unlikely the case with other life transitions explored in prior literature [73]. People may also choose to not use social media (or use it differently) during these major life transitions. Therefore, the above design suggestions cannot be uncritically followed without accounting for the complexities of the context. Further research is needed to uncover the specific ways and points in time that social media could support reintegration.
7.3.2. Personalized technology-based interventions for mental health.
Technology-based behavioral and psychological intervention strategies are increasingly applied to mental health for self-assessment and self-monitoring, psychoeducation, goal setting, and skill building [109]. To obtain desired outcomes, sustained client engagement and participation are crucial; however, technology-based interventions are known to have challenges with limited participation and high attrition rates [161]. Moreover, existing interventions consider different symptoms as distinct entities without taking into account the person’s social and ecological context. However, the clinical literature says that the boundaries between the presentation of different disorders are often not so strict [83]. One way to improve engagement and create room for representing individualized heterogeneity of mental health states and experiences could be factoring in the specific individual’s experiences into the intervention design and tailor support and care according to their context. The Possible Selves framework [103] and methodology we adopt in RQ1 can be applied to engagement data from intervention tools to uncover patterns of behaviors that can inform personalized delivery of support and care [29]. From RQ2, we found that after hospitalization two distinct prominent trajectories emerge: those who incorporate the illness and get back to social lives, and those who withdraw from active use of platforms. The support needs of these two groups might vary drastically and the intervention tools can account for these differences to maintain engagement from clients with varied experiences. In essence, we posit that such an approach to describe a person’s clinical and social care needs, as well as their mental health state aligns with the vision of NIMH’s Research Domain Criteria (RDoC) [83], that defines five ‘domains’ each reflecting a psychophysiological system in which a person’s functioning is impaired, to different degrees. The PSS-based recovery and reintegration trajectories can also inform out-patient programs or community integration programs that are traditionally referred to patients by social workers or staff during the time of discharge from the hospital. Specifically, this information might help contextualize how clinical treatment (as provided by the hospital), and social care (outside the hospital), including technology-mediated support, might contribute to a collaborative recovery and reintegration plan.
7.4. Limitations and Future Directions
Our work has some limitations. First, we note caveats in our data. The data on medical records comes from consented participants seeking treatment within a single healthcare system in a specific geography comprising English-speaking, Western populations. The demographics therefore, are skewed and we caution against sweeping generalizations. We also acknowledge that our examination of social media is limited to a single platform, Facebook. Moreover, we combined different mental health conditions into a single study population, to understand recovery and reintegration transitions surrounding hospitalization. Future work can extend the current findings to explore commonalities and differences in the transitions experienced by people with different illnesses and comorbid conditions. Second, we were able to capture aspects of clinical care based on hospitalization dates and social care based on digital traces from Facebook data. However, not all aspects of social care might be visible on social media. For instance, caregivers and offline connections, community integration programs and support groups both offline and online also contribute to social aspects of care in mental health. Future work can explore these offline facets. Similarly, the use of the PSS-based trajectories in clinical contexts (as discussed in section 7.2) requires additional rigorous validation in future work. Finally, for easier interpretation, we examined linear transitions that people experience around recovery and reintegration. However, literature suggests that transitions can be non-linear and cyclical [92]. Future work can explore modeling strategies and in-depth interviews to uncover these complex transitions, and pre- and post-hospitalization experiences.
8. CONCLUSION
In this paper we presented a theory-driven modeling approach to understand heterogeneous behaviors and self-presentations of people as they experience mental illness transitions. Through expert interviews and validation of the modeling approach, this paper contributes a taxonomy of six possible self statuses (PSS) exhibited on social media around psychiatric hospitalizations. Then, by studying how people transition from one PSS to another during the periods surrounding hospitalizations, we presented an empirical framework to understand clinical recovery and social reintegration trajectories of people. Finally, using the taxonomy of PSS and the framework elucidating their trajectories of transitions, we assessed social reintegration after psychiatric hospitalizations. Our work provides a first step towards combining peoples’ clinical and social experiences around psychiatric hospitalizations to extend the opportunities in leveraging social media for mental health.
CCS Concepts:
Human-centered computing → Computer supported cooperative work; Empirical studies in collaborative and social computing; Social media.
ACKNOWLEDGMENTS
We thank the members of the Social Dynamics and Well-Being Lab for their valuable feedback in preparing this manuscript. Part of this research was supported through a National Institutes of Health grant R01MH117172 to De Choudhury (PI), Birnbaum (Co-Investigator), and Kane (Co-Investigator), and a cooperative research agreement between Northwell Health and Georgia Tech, also to De Choudhury.
Footnotes
Overall number of posts includes status updates and activities such as check-ins on the timeline.
As information about the past PSS, we consider a weighted average of features before and after hospitalization.
Note that regression coefficients should be interpreted conditional on the penalty.
Contributor Information
SINDHU KIRANMAI ERNALA, Georgia Institute of Technology, USA.
KATHAN H. KASHIPAREKH, Georgia Institute of Technology, USA
AMIR BOLOUS, Georgia Institute of Technology, USA.
ASRA ALI, Zucker Hillside Hospital, Psychiatry Research, USA.
JOHN M. KANE, Zucker Hillside Hospital, Psychiatry Research, USA.
MICHAEL L. BIRNBAUM, Zucker Hillside Hospital, Psychiatry Research, USA
MUNMUN DE CHOUDHURY, Georgia Institute of Technology, USA.
REFERENCES
- [1].Abela John R. Z. and D’Alessandro David U.. 2002. Beck’s cognitive theory of depression: A test of the diathesis-stress and causal mediation components. British Journal of Clinical Psychology 41, 2 (2002), 111–128. [DOI] [PubMed] [Google Scholar]
- [2].Ådnanes M, Cresswell-Smith J, Melby L, Westerlund H, Šprah L, Sfetcu R, Straßmayr C, and Donisi V. 2019. Discharge planning, self-management, and community support: Strategies to avoid psychiatric rehospitalisation from a service user perspective. Patient Education and Counseling (2019). [DOI] [PubMed] [Google Scholar]
- [3].Ådnanes M, Melby L, Cresswell-Smith J, Westerlund H, Rabbi L, Dernovšek MZ, Šprah L, Sfetcu R, Straßmayr C, and Donisi V. 2018. Mental health service users’ experiences of psychiatric re-hospitalisation - an explorative focus group study in six European countries. BMC Health Services Research 18 (July 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ajzen Icek et al. 1991. The theory of planned behavior. Organizational behavior and human decision processes 50, 2 (1991), 179–211. [Google Scholar]
- [5].Alisky Joseph M. and Iczkowski Kenneth A.. 1990. Barriers to housing for deinstitutionalized psychiatric patients. Psychiatric Services 41, 1 (Jan 1990), 93–95. [DOI] [PubMed] [Google Scholar]
- [6].Anagnostopoulos Aris, Kumar Ravi, and Mahdian Mohammad. 2008. Influence and correlation in social networks. In Proceedings of the 14th ACM SIGKDD international conference on Knowledge discovery and data mining. ACM, 7–15. [Google Scholar]
- [7].Andalibi Nazanin, Haimson Oliver L, De Choudhury Munmun, and Forte Andrea. 2016. Understanding social media disclosures of sexual abuse through the lenses of support seeking and anonymity. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems. ACM, 3906–3918. [Google Scholar]
- [8].Andalibi Nazanin, Öztürk Pinar, and Forte Andrea. 2017. Sensitive self-disclosures, responses, and social support on Instagram: The case of #depression.. In CSCW. 1485–1500. [Google Scholar]
- [9].Anthony William A. 1993. Recovery from mental illness: the guiding vision of the mental health service system in the 1990s. Psychosocial rehabilitation journal 16, 4 (1993), 11. [Google Scholar]
- [10].Bachrach Leona L. 1975. Deinstitutionalization-an Analytical Review and Sociological Perspective. Number 4. US Department of Health, Education, and Welfare, Public Health Service …. [Google Scholar]
- [11].Baikie Karen A and Wilhelm Kay. 2005. Emotional and physical health benefits of expressive writing. Advances in psychiatric treatment 11, 5 (2005), 338–346. [Google Scholar]
- [12].Bak Waclaw. 2015. Possible selves: Implications for psychotherapy. International journal of mental health and addiction 13, 5 (2015), 650–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Baumer Eric PS, Mimno David, Guha Shion, Quan Emily, and Gay Geri K. 2017. Comparing grounded theory and topic modeling: Extreme divergence or unlikely convergence? Journal of the Association for Information Science and Technology 68, 6 (2017), 1397–1410. [Google Scholar]
- [14].Birchwood Max, Smith Jo, Cochrane Ray, Wetton Sheila, and Copestake Sonja. 1990. The social functioning scale the development and validation of a new scale of social adjustment for use in family intervention programmes with schizophrenic patients. The British Journal of Psychiatry 157, 6 (Dec 1990), 853–859. [DOI] [PubMed] [Google Scholar]
- [15].Birnbaum Michael Leo, Ernala Sindhu Kiranmai, Rizvi AF, Arenare Elizabeth, Van Meter AR, De Choudhury M, and Kane John M. 2019. Detecting relapse in youth with psychotic disorders utilizing patient-generated and patientcontributed digital data from Facebook. NPJ schizophrenia 5, 1 (2019), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Birnbaum Michael L, Ernala Sindhu Kiranmai, Rizvi Asra F, De Choudhury Munmun, and Kane John M. 2017. A collaborative approach to identifying social media markers of schizophrenia by employing machine learning and clinical appraisals. J. Med. Internet Res (2017). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Braithwaite Scott R, Giraud-Carrier Christophe, West Josh, Barnes Michael D, and Hanson Carl Lee. 2016. Validating machine learning algorithms for Twitter data against established measures of suicidality. JMIR mental health 3, 2 (2016). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Breckler Steven J.. 1984. Empirical validation of affect, behavior, and cognition as distinct components of attitude. Journal of Personality and Social Psychology 47, 6 (1984), 1191–1205. [DOI] [PubMed] [Google Scholar]
- [19].Brubaker Jed R, Kivran-Swaine Funda, Taber Lee, and Hayes Gillian R. 2012. Grief-stricken in a crowd: The language of bereavement and distress in social media. In Sixth International AAAI Conference on Weblogs and Social Media. [Google Scholar]
- [20].Bruckman Amy. 2002. Studying the amateur artist: A perspective on disguising data collected in human subjects research on the Internet. Ethics and Information Technology 4, 3 (2002), 217–231. [Google Scholar]
- [21].Burgess Eleanor R, Reddy Madhu C, Davenport Andrew, Laboi Paul, and Blandford Ann. 2019. “Tricky to get your head around” Information Work of People Managing Chronic Kidney Disease in the UK. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. 1–17. [Google Scholar]
- [22].Burke Moira and Kraut Robert. 2013. Using Facebook after losing a job: Differential benefits of strong and weak ties. In Proceedings of the 2013 conference on Computer supported cooperative work. 1419–1430. [Google Scholar]
- [23].Cardano Mario. 2010. Mental distress: Strategies of sense-making. Health 14, 3 (May 2010), 253–271. [DOI] [PubMed] [Google Scholar]
- [24].Carl Jenna R., Soskin David P., Kerns Caroline, and Barlow David H.. 2013. Positive emotion regulation in emotional disorders: A theoretical review. Clinical Psychology Review 33, 3 (Apr 2013), 343–360. [DOI] [PubMed] [Google Scholar]
- [25].Carr Helen. 2014. Returning ‘home’: Experiences of reintegration for asylum seekers and refugees. The British Journal of Social Work 44, suppl_1 (2014), i140–i156. [Google Scholar]
- [26].Chancellor Stevie, Baumer Eric PS, and De Choudhury Munmun. 2019. Who is the “Human” in Human-Centered Machine Learning: The case of predicting mental health from social media. Proceedings of the ACM on Human-Computer Interaction 3, CSCW (2019), 1–32.34322658 [Google Scholar]
- [27].Chancellor Stevie, Lin Zhiyuan, Goodman Erica L, Zerwas Stephanie, and De Choudhury Munmun. 2016. Quantifying and predicting mental illness severity in online pro-eating disorder communities. In Proceedings of the 19th ACM Conference on Computer-Supported Cooperative Work & Social Computing. ACM, 1171–1184. [Google Scholar]
- [28].Chen Yunan. 2011. Health information use in chronic care cycles. In Proceedings of the ACM 2011 conference on Computer supported cooperative work. 485–488. [Google Scholar]
- [29].Chikersal Prerna, Belgrave Danielle, Doherty Gavin, Enrique Angel, Palacios Jorge E, Richards Derek, and Thieme Anja. 2020. Understanding client support strategies to improve clinical outcomes in an online mental health intervention. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems. 1–16. [Google Scholar]
- [30].Chung Cindy and Pennebaker James W. 2007. The psychological functions of function words. Social communication (2007), 343–359. [Google Scholar]
- [31].Clarke Rachel. 2016. Possible Selves in First Episode Psychosis. A Mixed Methods Study. Ph.D. Dissertation. University of East Anglia. [Google Scholar]
- [32].Cohen Laura J. 1994. Psychiatric hospitalization as an experience of trauma. Archives of Psychiatric Nursing 8, 2 (1994), 78–81. [DOI] [PubMed] [Google Scholar]
- [33].Cohen Sheldon and Wills Thomas A. 1985. Stress, social support, and the buffering hypothesis. Psychological bulletin 98, 2 (1985), 310. [PubMed] [Google Scholar]
- [34].Coppersmith Glen, Dredze Mark, and Harman Craig. 2014. Quantifying mental health signals in twitter. In ACL Workshop on Computational Linguistics and Clinical Psychology. [Google Scholar]
- [35].Coppersmith Glen, Dredze Mark, Harman Craig, and Hollingshead Kristy. 2015. From ADHD to SAD: Analyzing the language of mental health on Twitter through self-reported diagnoses. NAACL HLT 2015 (2015), 1. [Google Scholar]
- [36].Corbin Juliet M and Strauss Anselm. 1991. A nursing model for chronic illness management based upon the trajectory framework. Scholarly inquiry for nursing practice 5, 3 (1991), 155–174. [PubMed] [Google Scholar]
- [37].Corrigan Patrick W., Larson Jonathon E., and Rüsch Nicolas. 2009. Self-stigma and the “why try” effect: impact on life goals and evidence-based practices. World Psychiatry 8, 2 (June 2009), 75–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Coughlin Steven S. 1990. Recall bias in epidemiologic studies. Journal of clinical epidemiology 43, 1 (1990), 87–91. [DOI] [PubMed] [Google Scholar]
- [39].Cutrona Carolyn E and Russell Daniel W. 1990. Type of social support and specific stress: Toward a theory of optimal matching. (1990). [Google Scholar]
- [40].Davidson Larry and White William. 2007. The concept of recovery as an organizing principle for integrating mental health and addiction services. The journal of behavioral health services & research 34, 2 (2007), 109–120. [DOI] [PubMed] [Google Scholar]
- [41].De Choudhury Munmun, Counts Scott, and Horvitz Eric. 2013. Major life changes and behavioral markers in social media: case of childbirth. In CSCW. ACM, 1431–1442. [Google Scholar]
- [42].De Choudhury Munmun and De Sushovan. 2014. Mental Health Discourse on reddit: Self-Disclosure, Social Support, and Anonymity.. In ICWSM. [Google Scholar]
- [43].De Choudhury Munmun, Gamon Michael, Counts Scott, and Horvitz Eric. 2013. Predicting depression via social media. In AAAI Conference on Weblogs and Social Media. [Google Scholar]
- [44].De Choudhury Munmun and Kiciman Emre. 2017. The language of social support in social media and its effect on suicidal ideation risk. In Eleventh International AAAI Conference on Web and Social Media. [PMC free article] [PubMed] [Google Scholar]
- [45].De Choudhury Munmun, Kiciman Emre, Dredze Mark, Coppersmith Glen, and Kumar Mrinal. 2016. Discovering shifts to suicidal ideation from mental health content in social media. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems. ACM, 2098–2110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].De Choudhury Munmun and Massimi Michael. 2015. “ She said yes”–Liminality and engagement announcements on Twitter. iConference 2015 Proceedings (2015). [Google Scholar]
- [47].Dijkers Marcel PJM, Whiteneck Gale, and El-Jaroudi Rana. 2000. Measures of social outcomes in disability research. Archives of physical medicine and rehabilitation 81 (2000), S63–S80. [DOI] [PubMed] [Google Scholar]
- [48].Dohrenwend Bruce P, Raphael Karen G, Schwartz Sharon, Stueve Ann, and Skodol Andrew. 1993. The structured event probe and narrative rating method for measuring stressful life events. (1993).
- [49].Donath Judith S. 2002. Identity and deception in the virtual community. In Communities in cyberspace. Routledge. [Google Scholar]
- [50].Ellison Nicole B, Steinfield Charles, and Lampe Cliff. 2007. The benefits of Facebook “friends:” Social capital and college students’ use of online social network sites. JCMC (2007). [Google Scholar]
- [51].Ellison Nicole B., Vitak Jessica, Gray Rebecca, and Lampe Cliff. 2014. Cultivating social resources on social network sites: Facebook relationship maintenance behaviors and their role in social capital processes. Journal of ComputerMediated Communication 19, 4 (Jul 2014), 855–870. [Google Scholar]
- [52].Elm Jessica HL, Lewis Jordan P, Walters Karina L, and Self Jen M. 2016. “I’m in this world for a reason”: Resilience and recovery among American Indian and Alaska Native two-spirit women. Journal of lesbian studies 20, 3–4 (2016), 352–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Ephraim Y and Merhav N. 2002. Hidden Markov processes. IEEE Transactions on Information Theory 48, 6 (Jun 2002). [Google Scholar]
- [54].Ernala Sindhu Kiranmai, Birnbaum Michael L, Candan Kristin A, Rizvi Asra F, Sterling William A, Kane John M, and De Choudhury Munmun. 2019. Methodological gaps in predicting mental health states from social media: triangulating diagnostic signals. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. [Google Scholar]
- [55].Ernala Sindhu Kiranmai, Rizvi Asra F, Birnbaum Michael L, Kane John M, and De Choudhury Munmun. 2017. Linguistic markers indicating therapeutic outcomes of social media disclosures of schizophrenia. Proc. ACM Hum.Comput.Interact (2017). [Google Scholar]
- [56].Eschler Jordan, Burgess Eleanor R., Reddy Madhu, and Mohr David C.. 2020. Emergent Self-Regulation Practices in Technology and Social Media Use of Individuals Living with Depression. In Proceedings of the 2020 CHI Conference on Human Factors in Computing Systems (CHI ‘20). Association for Computing Machinery, 1–13. [Google Scholar]
- [57].Eschler Jordan and Pratt Wanda. 2017. “ I’m so glad I met you” Designing Dynamic Collaborative Support for Young Adult Cancer Survivors. In Proceedings of the 2017 ACM Conference on Computer Supported Cooperative Work and Social Computing. 1763–1774. [Google Scholar]
- [58].Farkas Marianne. 1996. Recovery, rehabilitation, reintegration: Words vs. meaning. World Association of Psychosocial Rehabilitation Bulletin 8, 4 (1996), 6–8. [Google Scholar]
- [59].Feuston Jessica L, Marshall-Fricker Charlotte G, and Piper Anne Marie. 2017. The social lives of individuals with traumatic brain injury. In Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems. 182–194. [Google Scholar]
- [60].Feuston Jessica L and Piper Anne Marie. 2019. Everyday experiences: small stories and mental illness on Instagram. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. 1–14. [Google Scholar]
- [61].Florenzano Ramón U. 1991. Chronic mental illness in adolescence: A global overview. Pediatrician 18, 2 (1991). [PubMed] [Google Scholar]
- [62].Genuis Shelagh K. and Bronstein Jenny. 2017. Looking for “normal”: Sense making in the context of health disruption. Journal of the Association for Information Science and Technology 68, 3 (2017), 750–761. [Google Scholar]
- [63].Getty Emily, Cobb Jessica, Gabeler Meryl, Nelson Christine, Weng Ellis, and Hancock Jeffrey. 2011. I said your name in an empty room: Grieving and continuing bonds on Facebook. In Proceedings of the SIGCHI Conference on human factors in computing systems. 997–1000. [Google Scholar]
- [64].Gibson Lorna and Hanson Vicki L. 2013. Digital motherhood: How does technology help new mothers?. In Proceedings of the SIGCHI conference on human factors in computing systems. ACM, 313–322. [Google Scholar]
- [65].Glacken M, Kernohan G, and Coates V. 2001. Diagnosed with hepatitis C: A descriptive exploratory study. International journal of nursing studies 38, 1 (2001), 107–116. [DOI] [PubMed] [Google Scholar]
- [66].Godbold Natalya. 2006. Beyond information seeking: Towards a general model of information behaviour. Information Research: An International Electronic Journal 11, 4 (Jul 2006). [Google Scholar]
- [67].Godbold Natalya. 2011. An evolving normal: Making sense of renal dialysis via online discussion boards. Relational Concepts in Medicine (May 2011), 205–214. [Google Scholar]
- [68].Gove Walter R.. 1973. The Stigma of Mental Hospitalization: An Attempt to Evaluate Its Consequences. Archives of General Psychiatry 28, 4 (April 1973), 494. [DOI] [PubMed] [Google Scholar]
- [69].Gove Walter R and Fain Terry. 1973. The stigma of mental hospitalization: An attempt to evaluate its consequences. Archives of General Psychiatry 28, 4 (1973), 494–500. [DOI] [PubMed] [Google Scholar]
- [70].Griffiths Curt Taylor, Dandurand Yvon, and Murdoch Danielle. 2007. The social reintegration of offenders and crime prevention. Vol. 4. National Crime Prevention Centre; Ottawa, Ontario, Canada. [Google Scholar]
- [71].Grimmer Justin and Stewart Brandon M. 2013. Text as data: The promise and pitfalls of automatic content analysis methods for political texts. Political analysis 21, 3 (2013), 267–297. [Google Scholar]
- [72].Guntuku Sharath Chandra, Schwartz H Andrew, Kashyap Adarsh, Gaulton Jessica S, Stokes Daniel C, Asch David A, Ungar Lyle H, and Merchant Raina M. 2020. Variability in Language used on Social Media prior to Hospital Visits. Scientific Reports 10, 1 (2020), 1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [73].Haimson Oliver. 2018. Social media as social transition machinery. Proceedings of the ACM on Human-Computer Interaction 2, CSCW (2018), 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [74].Haimson Oliver L, Brubaker Jed R, Dombrowski Lynn, and Hayes Gillian R. 2015. Disclosure, stress, and support during gender transition on Facebook. In CSCW. ACM, 1176–1190. [Google Scholar]
- [75].Haimson Oliver L., Brubaker Jed R., Dombrowski Lynn, and Hayes Gillian R.. 2016. Digital Footprints and Changing Networks During Online Identity Transitions. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (CHI ‘16). Association for Computing Machinery, 2895–2907. 10.1145/2858036.2858136 [DOI] [Google Scholar]
- [76].Hayes Gillian R, Abowd Gregory D, Davis John S, Blount Marion L, Ebling Maria, and Mynatt Elizabeth D. 2008. Opportunities for pervasive computing in chronic cancer care. In International Conference on Pervasive Computing. Springer, 262–279. [Google Scholar]
- [77].Hekler Eric B, Michie Susan, Pavel Misha, Rivera Daniel E, Collins Linda M, Jimison Holly B, Garnett Claire, Parral Skye, and Spruijt-Metz Donna. 2016. Advancing models and theories for digital behavior change interventions. American journal of preventive medicine 51, 5 (2016), 825–832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Helliwell John F and Putnam Robert D. 2004. The social context of well-being. Philos. Trans. Royal Soc. B (2004). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [79].Hobbs William R and Burke Moira K. 2017. Connective recovery in social networks after the death of a friend. Nature Human Behaviour 1, 5 (2017), 0092. [Google Scholar]
- [80].Hoyle Rick H and Sherrill Michelle R. 2006. Future orientation in the self-system: Possible selves, self-regulation, and behavior. Journal of personality 74, 6 (2006), 1673–1696. [DOI] [PubMed] [Google Scholar]
- [81].Huang Tom, Elghafari Anas, Relia Kunal, and Chunara Rumi. 2017. High-resolution temporal representations of alcohol and tobacco behaviors from social media data. Proceedings of the ACM on human-computer interaction 1, CSCW (2017), 1–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [82].Huxley P, Evans SC, Madge S, Webber M, Burchardt T, McDaid D, and Knapp M. 2012. Social and community opportunities profile (SCOPE) Short Version. (2012). [DOI] [PubMed]
- [83].Insel Thomas R. 2014. The NIMH research domain criteria (RDoC) project: precision medicine for psychiatry. American Journal of Psychiatry 171, 4 (2014), 395–397. [DOI] [PubMed] [Google Scholar]
- [84].Iqbal Zaffer, Birchwood Max, Chadwick Paul, and Trower Peter. 2000. Cognitive approach to depression and suicidal thinking in psychosis: 2. Testing the validity of a social ranking model. The British Journal of Psychiatry 177, 6 (2000), 522–528. [PubMed] [Google Scholar]
- [85].Jacob KS. 2015. Recovery model of mental illness: A complementary approach to psychiatric care. Indian journal of psychological medicine 37, 2 (2015), 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [86].Jacobs Maia, Clawson James, and Mynatt Elizabeth D. 2016. A cancer journey framework: guiding the design of holistic health technology. In Proceedings of the 10th EAI International Conference on Pervasive Computing Technologies for Healthcare. 114–121. [Google Scholar]
- [87].Janis Irene Belle, Veague Heather Barnett, and Driver-Linn Erin. 2006. Possible selves and borderline personality disorder. Journal of clinical psychology 62, 3 (2006), 387–394. [DOI] [PubMed] [Google Scholar]
- [88].Kaziunas Elizabeth, Buyuktur Ayse G, Jones Jasmine, Choi Sung W, Hanauer David A, and Ackerman Mark S. 2015. Transition and reflection in the use of health information: the case of pediatric bone marrow transplant caregivers. In Proceedings of the 18th ACM Conference on Computer Supported Cooperative Work & Social Computing. 1763–1774. [Google Scholar]
- [89].Kent Suzanne and Yellowlees Peter. 1994. Psychiatric and social reasons for frequent rehospitalization. Psychiatric Services 45, 4 (1994), 347–350. [DOI] [PubMed] [Google Scholar]
- [90].Keyes Corey LM. 2005. Mental illness and/or mental health? Investigating axioms of the complete state model of health. Journal of consulting and clinical psychology 73, 3 (2005), 539. [DOI] [PubMed] [Google Scholar]
- [91].Kim Woorim, Jang Suk-Yong, Lee Tae-Hoon, Lee Joo Eun, and Park Eun-Cheol. 2018. Association between continuity of care and subsequent hospitalization and mortality in patients with mood disorders: Results from the Korea National Health Insurance cohort. PLOS ONE 13, 11 (Nov 2018), e0207740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [92].Kralik Debbie. 2002. The quest for ordinariness: transition experienced by midlife women living with chronic illness. Journal of advanced nursing 39, 2 (2002), 146–154. [DOI] [PubMed] [Google Scholar]
- [93].Kralik Debbie, Visentin Kate, and Van Loon Antonia. 2006. Transition: a literature review. Journal of advanced nursing 55, 3 (2006), 320–329. [DOI] [PubMed] [Google Scholar]
- [94].Leamy Mary, Bird Victoria, Boutillier Clair Le, Williams Julie, and Slade Mike. 2011. Conceptual framework for personal recovery in mental health: systematic review and narrative synthesis. The British Journal of Psychiatry 199, 6 (2011), 445–452. [DOI] [PubMed] [Google Scholar]
- [95].Levonian Zachary, Erikson Drew Richard, Luo Wenqi, Narayanan Saumik, Rubya Sabirat, Vachher Prateek, Terveen Loren, and Yarosh Svetlana. 2020. Bridging qualitative and quantitative methods for user modeling: Tracing cancer patient behavior in an online health community. In ICWSM. [Google Scholar]
- [96].Li Ian, Dey Anind K., and Forlizzi Jodi. 2011. Understanding my data, myself: supporting self-reflection with ubicomp technologies. In Proceedings of the 13th international conference on Ubiquitous computing - UbiComp ‘11. ACM Press. [Google Scholar]
- [97].Link Bruce G, Struening Elmer L, Neese-Todd Sheree, Asmussen Sara, and Phelan Jo C. 2001. Stigma as a barrier to recovery: The consequences of stigma for the self-esteem of people with mental illnesses. Psychiatric services 52, 12 (2001), 1621–1626. [DOI] [PubMed] [Google Scholar]
- [98].Liu Jiaxin, Weitzman Elissa R, and Chunara Rumi. 2017. Assessing behavior stage progression from social media data. In Proceedings of the 2017 ACM Conference on Computer Supported Cooperative Work and Social Computing. 1320–1333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [99].Lucksted Alicia and Drapalski Amy L. 2015. Self-stigma regarding mental illness: Definition, impact, and relationship to societal stigma. (2015). [DOI] [PubMed]
- [100].Lucksted Alicia and Drapalski Amy L.. 2015. Self-stigma regarding mental illness: Definition, impact, and relationship to societal stigma. Psychiatric Rehabilitation Journal 38, 2 (2015), 99–102. Place: US Publisher: Educational Publishing Foundation. [DOI] [PubMed] [Google Scholar]
- [101].MacLean Diana, Gupta Sonal, Lembke Anna, Manning Christopher, and Heer Jeffrey. 2015. Forum77: An Analysis of an Online Health Forum Dedicated to Addiction Recovery. In Computer-Supported Cooperative Work and Social Computing (CSCW). [Google Scholar]
- [102].Mannell Roger C, Iso-Ahola Seppo E, et al. 1985. Work constraints on leisure: a social psychological analysis. Work constraints on leisure: a social psychological analysis. (1985), 155–187. [Google Scholar]
- [103].Markus Hazel and Nurius Paula. 1986. Possible selves. American psychologist 41, 9 (1986), 954. [Google Scholar]
- [104].Massimi Michael and Baecker Ronald M. 2010. A death in the family: opportunities for designing technologies for the bereaved. In Proceedings of the SIGCHI conference on Human Factors in computing systems. ACM, 1821–1830. [Google Scholar]
- [105].Massimi Michael, Dimond Jill P, and Le Dantec Christopher A. 2012. Finding a new normal: the role of technology in life disruptions. In Proceedings of the acm 2012 conference on computer supported cooperative work. ACM, 719–728. [Google Scholar]
- [106].Massimi Michael, Harper Richard, and Sellen Abigail J. 2014. Real, but glossy: technology and the practical pursuit of magic in modern weddings. In Proceedings of the 17th ACM conference on Computer supported cooperative work & social computing. ACM, 854–865. [Google Scholar]
- [107].Masters Grace A, Baldessarini Ross J, Öngür Dost, and Centorrino Franca. 2014. Factors associated with length of psychiatric hospitalization. Comprehensive psychiatry 55, 3 (2014), 681–687. [DOI] [PubMed] [Google Scholar]
- [108].McLachlan Geoffrey J and Basford Kaye E. 1988. Mixture models: Inference and applications to clustering. Vol. 38. [Google Scholar]
- [109].Mohr David C., Burns Michelle Nicole, Schueller Stephen M., Clarke Gregory, and Klinkman Michael. 2013. Behavioral intervention technologies: Evidence review and recommendations for future research in mental health. General Hospital Psychiatry 35, 4 (Jul 2013), 332–338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Moos Rudolf H. 1982. Coping with acute health crises. In Handbook of clinical health psychology. Springer, 129–151. [Google Scholar]
- [111].Morioka Tsubasa, Ellison Nicole B, and Brown Michael. 2016. Identity work on social media sites: Disadvantaged students’ college transition processes. In Proceedings of the 19th ACM conference on computer-supported cooperative work & social computing. ACM, 848–859. [Google Scholar]
- [112].Moses Tally. 2014. Determinants of mental illness stigma for adolescents discharged from psychiatric hospitalization. Social Science & Medicine 109 (2014), 26–34. [DOI] [PubMed] [Google Scholar]
- [113].Muller Michael, Guha Shion, Baumer Eric PS, Mimno David, and Shami N Sadat. 2016. Machine learning and grounded theory method: convergence, divergence, and combination. In Proceedings of the 19th International Conference on Supporting Group Work. 3–8. [Google Scholar]
- [114].Murnane Elizabeth L, Cosley Dan, Chang Pamara, Guha Shion, Frank Ellen, Gay Geri, and Matthews Mark. 2016. Self-monitoring practices, attitudes, and needs of individuals with bipolar disorder: implications for the design of technologies to manage mental health. Journal of the American Medical Informatics Association 23, 3 (2016), 477–484. [DOI] [PubMed] [Google Scholar]
- [115].Naslund JA, Aschbrenner KA, Marsch LA, and Bartels SJ. 2016. The future of mental health care: peer-to-peer support and social media. Epidemiology and psychiatric sciences 25, 2 (2016), 113–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [116].Neuberger Julia and Tallis Raymond. 1999. We do need a new word for patients? British Medical Journal 318, 7200 (1999), 1756–1756.10381717 [Google Scholar]
- [117].Newman-Taylor Katherine, Garner Christie, Vernon-Wilson Elizabeth, Paas Karlien HW, Herbert Lesley, and Au-Yeung Sheena K. 2017. Psychometric evaluation of the hope, agency and opportunity (HAO); a brief measure of mental health recovery. Journal of Mental Health 26, 6 (2017), 562–568. [DOI] [PubMed] [Google Scholar]
- [118].Nolen-Hoeksema Susan. 2000. The role of rumination in depressive disorders and mixed anxiety/depressive symptoms. Journal of abnormal psychology 109, 3 (2000), 504. [PubMed] [Google Scholar]
- [119].Oh Hyun Jung, Lauckner Carolyn, Boehmer Jan, Fewins-Bliss Ryan, and Li Kang. 2013. Facebooking for health: An examination into the solicitation and effects of health-related social support on social networking sites. Computers in human behavior 29, 5 (2013), 2072–2080. [Google Scholar]
- [120].Paksarian Diana, Mojtabai Ramin, Kotov Roman, Cullen Bernadette, Nugent Katie L, and Bromet Evelyn J. 2014. Perceived trauma during hospitalization and treatment participation among individuals with psychotic disorders. Psychiatric Services 65, 2 (2014), 266–269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [121].Paul Michael J, White Ryen W, and Horvitz Eric. 2015. Diagnoses, decisions, and outcomes: Web search as decision support for cancer. In Proceedings of the 24th International Conference on World Wide Web. 831–841. [Google Scholar]
- [122].Pavalanathan Umashanthi and De Choudhury Munmun. 2015. Identity management and mental health discourse in social media. In Proceedings of the 24th International Conference on World Wide Web. 315–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [123].Pennebaker James W and Graybeal Anna. 2001. Patterns of natural language use: Disclosure, personality, and social integration. Current Directions in Psychological Science 10, 3 (2001), 90–93. [Google Scholar]
- [124].Perlman Helen Harris. 1951. The caseworker’s use of collateral information. Social Casework 32, 8 (1951), 325–333. [Google Scholar]
- [125].Perrin Andrew and Anderson Monica. 2019. Share of US adults using social media, including Facebook, is mostly unchanged since 2018. Pew Research Center 10 (2019). [Google Scholar]
- [126].Philippi Carissa L. and Koenigs Michael. 2014. The neuropsychology of self-reflection in psychiatric illness. Journal of psychiatric research 0 (Jul 2014), 55–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Povey Rachel, Conner Mark, Sparks Paul, James Rhiannon, and Shepherd Richard. 1999. A critical examination of the application of the Transtheoretical Model’s stages of change to dietary behaviours. Health Education Research 14, 5 (1999), 641–651. [DOI] [PubMed] [Google Scholar]
- [128].Prochaska James O and Velicer Wayne F. 1997. The transtheoretical model of health behavior change. American journal of health promotion 12, 1 (1997), 38–48. [DOI] [PubMed] [Google Scholar]
- [129].Provencher Helene L and Keyes Corey LM. 2013. Recovery: A complete mental health perspective. In Mental well-being. Springer, 277–297. [Google Scholar]
- [130].Putnam Robert D et al. 2000. Bowling alone: The collapse and revival of American community. Simon and schuster. [Google Scholar]
- [131].Ramon Shulamit, Healy Bill, and Renouf Noel. 2007. Recovery from mental illness as an emergent concept and practice in Australia and the UK. International Journal of Social Psychiatry 53, 2 (2007), 108–122. [DOI] [PubMed] [Google Scholar]
- [132].Resnik Philip, Garron Anderson, and Resnik Rebecca. 2013. Using topic modeling to improve prediction of neuroticism and depression. In Proceedings of the 2013 Conference on Empirical Methods in Natural. Association for Computational Linguistics, 1348–1353. [Google Scholar]
- [133].Robinson Delbert, Woerner Margaret G, Alvir Jose Ma J, Bilder Robert, Goldman Robert, Geisler Stephen, Koreen Amy, Sheitman Brian, Chakos Miranda, Mayerhoff David, et al. 1999. Predictors of relapse following response from a first episode of schizophrenia or schizoaffective disorder. Archives of general psychiatry 56, 3 (1999), 241–247. [DOI] [PubMed] [Google Scholar]
- [134].Saha Koustuv, Chan Larry, De Barbaro Kaya, Abowd Gregory D, and De Choudhury Munmun. 2017. Inferring mood instability on social media by leveraging ecological momentary assessments. Proceedings of the ACM on Interactive, Mobile, Wearable and Ubiquitous Technologies 1, 3 (2017), 95. [Google Scholar]
- [135].Saha Koustuv, Sugar Benjamin, Torous John, Abrahao Bruno, Kıcıman Emre, and De Choudhury Munmun. 2019. A Social Media Study on the Effects of Psychiatric Medication Use. In Proceedings of the International AAAI Conference on Web and Social Media, Vol. 13. 440–451. [PMC free article] [PubMed] [Google Scholar]
- [136].Semaan Bryan C, Britton Lauren M, and Dosono Bryan. 2016. Transition resilience with ICTs:’Identity awareness’ in veteran re-integration. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems. ACM, 2882–2894. [Google Scholar]
- [137].Sevin Elodie and Ladwein Richard. 2008. To Start Being….The anticipation of a social role through consumption in life transition: the case of the first-time pregnancy. ACR North American Advances NA-35 (2008). [Google Scholar]
- [138].Shankar Janki and Collyer Fran. 2004. Support needs of people with mental illness in vocational rehabilitation programs-the role of the social network. International Journal of Psychosocial Rehabilitation 7, a (2004), 15–28. [Google Scholar]
- [139].Sharfstein Steven S. 2009. Goals of inpatient treatment for psychiatric disorders. Annual Review of Medicine 60 (2009), 393–403. [DOI] [PubMed] [Google Scholar]
- [140].Sharma Eva and De Choudhury Munmun. 2018. Mental Health Support and its Relationship to Linguistic Accommodation in Online Communities. In Proceedings of the 2018 CHI Conference on Human Factors in Computing Systems. ACM, 641. [Google Scholar]
- [141].Shen Judy Hanwen and Rudzicz Frank. 2017. Detecting anxiety through Reddit. In Proceedings of the Fourth Workshop on Computational Linguistics and Clinical Psychology—From Linguistic Signal to Clinical Reality. 58–65. [Google Scholar]
- [142].Simons Joke, Vansteenkiste Maarten, Lens Willy, and Lacante Marlies. 2004. Placing motivation and future time perspective theory in a temporal perspective. Educational psychology review 16, 2 (2004), 121–139. [Google Scholar]
- [143].Skeels Meredith M. and Grudin Jonathan. 2009. When social networks cross boundaries: a case study of workplace use of facebook and linkedin. In Proceedings of the ACM 2009 international conference on Supporting group work (GROUP ‘09). Association for Computing Machinery, 95–104. 10.1145/1531674.1531689 [DOI] [Google Scholar]
- [144].Smith Madeline E, Nguyen Duyen T, Lai Charles, Leshed Gilly, and Baumer Eric PS. 2012. Going to college and staying connected: Communication between college freshmen and their parents. In Proceedings of the ACM 2012 conference on computer supported cooperative work. ACM, 789–798. [Google Scholar]
- [145].Spitzer Robert L, Williams Janet BW, Gibbon Miriam, and First Michael B. 1992. The structured clinical interview for DSM-III-R (SCID): I: history, rationale, and description. Archives of general psychiatry 49, 8 (1992), 624–629. [DOI] [PubMed] [Google Scholar]
- [146].Starfield Barbara. 2011. Is patient-centered care the same as person-focused care? The Permanente Journal 15, 2 (2011), 63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [147].ABP Staring, Van der Gaag Mark, Van den Berge Marcel, Duivenvoorden HJ, and Mulder CL. 2009. Stigma moderates the associations of insight with depressed mood, low self-esteem, and low quality of life in patients with schizophrenia spectrum disorders. Schizophrenia research 115, 2–3 (2009), 363–369. [DOI] [PubMed] [Google Scholar]
- [148].Sterling Evelina W, Silke A, Tucker Sherry, Fricks Larry, and Druss Benjamin G. 2010. Integrating wellness, recovery, and self-management for mental health consumers. Community mental health journal 46, 2 (2010), 130–138. [DOI] [PubMed] [Google Scholar]
- [149].Strauss Anselm Leonard. 1985. Social organization of medical work. University of Chicago Press. [Google Scholar]
- [150].Stutzman Frederic and Hartzog Woodrow. 2012. Boundary regulation in social media. In Proceedings of the ACM 2012 conference on Computer Supported Cooperative Work (CSCW ‘12). Association for Computing Machinery, 769–778. [Google Scholar]
- [151].Tausczik Yla R and Pennebaker James W. 2010. The psychological meaning of words: LIWC and computerized text analysis methods. Journal of Language and Social Psychology 29, 1 (2010), 24–54. [Google Scholar]
- [152].Tse Samson and Ng Roger MK. 2014. Applying a mental health recovery approach for people from diverse backgrounds: the case of collectivism and individualism paradigms. Journal of Psychosocial Rehabilitation and Mental Health 1, 1 (2014), 7–13. [Google Scholar]
- [153].Tulloch AD, David AS, and Thornicroft G. 2016. Exploring the predictors of early readmission to psychiatric hospital. Epidemiology and psychiatric sciences 25, 2 (2016), 181–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [154].Van Gennep Arnold. 1909. The rites of passage.
- [155].Viggiano Theresa, Pincus Harold A, and Crystal Stephen. 2012. Care transition interventions in mental health. Current opinion in psychiatry 25, 6 (2012), 551–558. [DOI] [PubMed] [Google Scholar]
- [156].Wellman Barry and Wortley Scot. 1990. Different strokes from different folks: Community ties and social support. American journal of Sociology 96, 3 (1990), 558–588. [Google Scholar]
- [157].Wen Miaomiao and Rosé Carolyn Penstein. 2012. Understanding participant behavior trajectories in online health support groups using automatic extraction methods. In Proceedings of the 17th ACM international conference on Supporting group work. 179–188. [Google Scholar]
- [158].Wheaton Blair. 1990. Life transitions, role histories, and mental health. American sociological review (1990), 209–223. [Google Scholar]
- [159].Yang Diyi, Kraut Robert E, Smith Tenbroeck, Mayfield Elijah, and Jurafsky Dan. 2019. Seekers, providers, welcomers, and storytellers: Modeling social roles in online health communities. In Proceedings of the 2019 CHI Conference on Human Factors in Computing Systems. 1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [160].Yarosh Svetlana, Chieh Yee, Abowd Gregory D, et al. 2009. Supporting parent–child communication in divorced families. International Journal of Human-Computer Studies 67, 2 (2009), 192–203. [Google Scholar]
- [161].Yeager Carolyn M. and Benight Charles C.. 2018. If we build it, will they come? Issues of engagement with digital health interventions for trauma recovery. mHealth 4 (Sep 2018). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [162].Zanarini Mary C, Frankenburg Frances R, Khera Gagan S, and Bleichmar Julieta. 2001. Treatment histories of borderline inpatients. Comprehensive psychiatry 42, 2 (2001), 144–150. [DOI] [PubMed] [Google Scholar]
- [163].Zhang Renwen. 2017. The stress-buffering effect of self-disclosure on Facebook: An examination of stressful life events, social support, and mental health among college students. Comput. Hum. Behav (2017). [Google Scholar]
- [164].Zimmerman Mark and Mattia Jill I. 2001. The psychiatric diagnostic screening questionnaire: development, reliability and validity. Comprehensive psychiatry (2001). [DOI] [PubMed] [Google Scholar]


