Abstract
Purpose
Polysaccharide Krestin (PSK) is a mushroom extract that has been long used in Asia and recently in Western countries as a treatment for cancer due to its presumed immune potentiating effects. Although there have been reports of clinical responses after patients have ingested PSK, the mechanism of action of the agent remains undefined. The current study was undertaken to investigate the mechanism of the anti-tumor actions of PSK.
Experimental Design
The immunostimulatory effect of PSK was first evaluated in vitro using splenocytes from neu transgenic mice and TLR2 knockout (TLR2−/−) mice. Then the immunostimualtory and anti-tumor effect of PSK was determined using tumor-bearing neu transgenic mice, TLR2−/− and wild type C57BL/6 mice.
Results
We demonstrate that PSK is a selective TLR2 agonist, and the activation of dendritic cells (DC) and T cells by PSK is dependent on TLR2. Oral administration of PSK in neu transgenic mice significantly inhibits breast cancer growth. Selective depletion of specific cell populations suggests that the anti-tumor effect of PSK is dependent on both CD8+ T cell and NK cells, but not CD4+ T cells. PSK does not inhibit tumor growth in TLR2−/− mice suggesting the anti-tumor effect is mediated by TLR2.
Conclusion
These results demonstrate that PSK, a natural product commonly used for the treatment of cancer, is a specific TLR2 agonist and has potent anti-tumor effects via stimulation of both innate and adaptive immune pathways.
Keywords: PSK, TLR2, breast cancer, CAM, cancer immunotherapy, medicinal mushrooms
Introduction
In the United States, it is reported that 42% to 69% of people with cancer use both conventional and complementary and alternative medicine (CAM) to combat their disease (1, 2). Annual expenditures associated with use of CAM are estimated to be approximately $13.7 billion (3). Mushroom extracts are among one of the most commonly used CAM therapies. Mushrooms are a popular cancer treatment in Asian countries for presumed immune potentiating and anti-tumor effects (4). Recently, a phase I/II trial of a polysaccharide extract from Grifola frondosa (Maitake mushroom) was performed in breast cancer patients in the United States and demonstrated that the oral intake of mushroom extract resulted in increased cytokine production (IL-2, TNF-α, and IL-10) by immune cells to more than 50% of baseline (5). However, the specific mechanism by which medicinal mushroom extracts modulate the immune system has not been defined.
Polysaccharide Krestin (PSK) is one of the most commonly used mushroom extracts (6). It was approved as a prescription drug for the treatment of cancer in Japan in 1977. By 1987, PSK accounted for more than 25% of total national expenditure for anticancer agents in Japan (7). It is a commercially available highly purified extract of Trametes (Coriolus) versicolor strain CM-101. The major component is beta-glucan compounds ranging in size from 94 to 100 kDa (6). Clinical trials have suggested that PSK may significantly extend survival in cancers of the stomach (8, 9), colorectum (10–12), and lung (13). A number of publications suggest PSK may be an immune modulator, inducing gene expression of IL-8 in peripheral blood mononuclear cells after oral administration (14), stimulating T cell proliferation (15), and improving the function of CD4+ T cells in gut-associated lymphoid tissue (16). The specific receptor/pathway via which PSK might stimulate immune cells remains unknown.
The current study was undertaken to determine whether PSK could directly stimulate immune system cells, to assess the anti-tumor activity of PSK in a transgenic mouse model of breast cancer, and to identify the mechanism of action of the extract.
Materials and Methods
Animals
A colony of neu transgenic mice harboring the non-transforming rat neu [strain name, FVB/N-TgN (MMTVneu)-202Mul] was established in our animal facilities from breeding pairs (Jackson Laboratory, Bar Harbor, ME) and maintained as previously described (17). TLR2−/− and TLR4−/− mice were originally obtained from Dr. Shizuo Akira (Osaka, Japan). Wild type C57BL/6 mice were obtained from Jackson Laboratory. Mice were maintained under strict inbreeding conditions. All of the procedures were performed in compliance with the University of Washington Institutional Animal Care and Use Committee guidelines.
Reagents
Reagents used included fetal bovine serum (FBS) (Gemini Bioproducts, Woodland, CA), RPMI 1640, PBS, penicillin-streptomycin, and L-glutamine (Invitrogen Life Technologies, Grand Island, NY), fluorochrome-conjugated monoclonal antibodies targeting CD3, CD4, CD8, CD11c, NK1.1, Foxp3, and TLR2 (eBiosciences, San Diego, CA), [3H]-Thymidine (PerkinElmer, Boston, MA), RNAqueous4PCR kit for RNA extraction (Ambion, Austin, TX), primers and probes and gene expression master mix for real time PCR (Applied Biosystems, Foster City, CA). PSK was purchased from Kureha Pharmaceuticals (Japan). PSK was dissolved in PBS at a stock concentration of 10 mg/ml. Aliquots of 100 µl were stored at −80 °C. The frozen aliquots were thawed immediately before use.
PSK activation of splenocytes in vitro
The proliferation of splenocytes from neu transgenic mice after in vitro PSK treatment was evaluated using a [3H]-thymidine incorporation assay in 96-well plates as previously described (18). In brief, splenocytes were cultured in 96-well plates (200,000 cells/well) in RPMI and incubated with PSK (1–200 µg/ml) for 96 hours. [3H]-thymidine (1 µCi/well) was included for the last 16 hours of culture. For time-course treatment, splenocytes were stimulated with PSK (100 µg/ml) for 24, 48, 72, or 96 hours. Cytokine levels in the culture supernatant were measured using a mouse Th1/Th2 cytokine kit according to the manufacture’s instructions. (Meso Scale Discovery, Gaithersburg, MD). To measure the percentage of each immune subset (CD4 and CD8 T cells, NK, and B cells), PSK or control PBS-treated splenocytes were stained with fluorochrome conjugated anti-CD4, CD8, NK1.1, and CD19 antibodies using standard procedures as previously described (17). To measure PSK-stimulated IFN-γ production from NK cells, splenocytes from TLR2−/− mice or WT C57BL/6 mice were treated with PSK (100 µg/ml) for 24 hours. Intracellular staining was used to evaluate IFN-γ production by NK cells, using similar method as described in our previous publication (19). To measure the expression of TLR2 on each immune subset, splenocytes were stained with anti-TLR2-PE mAb (eBiosciences) following the manufacture’s instructions and the cells were co-stained with mAbs against CD3, NK1.1, CD19, and CD11c. The expression of TLR2 on MMC tumor cells was measured using similar method.
PSK activation of DC in vitro
Cells were collected from the bone marrow of femurs of mice under aseptic conditions and cultured in 24 well plates in culture medium (RPMI with 10% FBS, 50 µM beta-mercaptoethanol, and penicillin/streptomycin) after lysing red blood cells. Recombinant mouse IL-4 and GM-CSF was included at a final concentration of 20 ng/ml after removal of non-adherent cells. On day 7, cells were split and cultured in the presence of PSK (200 µg/ml), LPS (100 ng/ml, positive control), or PBS (negative control). After a 48 hour treatment, culture supernatant from each well was collected for analysis of IL-12p40 and IL-12p70 using ELISA kits (eBiosciences). The adherent cells were detached and one million cells per well were stained with anti-CD11c-APC, anti-CD80-PE, and anti-CD86-PerCP, and analyzed on a FACS Canto analyzer. FACS data analysis was performed using FlowJo software (Tree Star, OR).
Assessment of TLR activation using HEK293 cell transfectants
Human embryonic kidney cells (HEK293) expressing TLR2, TLR3, TLR4, TLR5, TLR7, TLR8, or TLR9 (InvivoGen, San Diego, CA) were cultured in DMEM (Cambrex, Walkersville, MD) containing 4.5 g/liter L-glucose (Sigma-Aldrich, St. Louis, MO) and 10% FBS. To measure NF-κB activation, the TLR-transfected HEK cells were co-transfected with a plasmid that has NF-κB inducible reporter construct-secretary alkaline phosphatase (SEAP) activity. The cells were then incubated with different doses of PSK (0.5–1000 µg/ml) in 1:3 dilution or with serial dilutions of the known agonist for each TLR as a positive control (heat killed listeria monocytogenes (HKLM) for TLR2, poly (I:C) for TLR3, LPS for TLR4, flagellin for TLR5, resiquimod for TLR7 and 8, CpG ODN2006 for TLR9). After overnight incubation, the culture supernatant was collected and the SEAP activity in the supernatant was measured using a Quanti-blue assay (InvivoGen).
Treatment of tumor-bearing mice with oral PSK
The anti-tumor effect of PSK was evaluated in neu transgenic mice in both implanted tumor and spontaneous tumor setting, and in TLR2−/− and wild type C57BL/6 mice with implanted tumors. For implanted tumor in the neu transgenic mice, one million Mouse Mammary Carcinoma (MMC) cells, a syngeneic tumor cell line derived from a spontaneous tumor in these mice (18), was injected to the mice subcutaneously. PSK treatment was started at two week after the implantation when the implanted tumor just became palpable (average size = 50 mm3). For spontaneous tumors, neu transgenic mice with palpable tumors (average size = 50 mm3) were randomly assigned to be treated with PSK (2 mg/mouse, equivalent to 100 mg/kg, 3 times per week for 4 weeks) or control PBS (n=5 per group). For implanted tumors in C57BL/6 and TLR2−/− mice, the tumor was started by subcutaneous injection of 40,000 TC-1 cervical cancer cells (C57BL/6 background, originally obtained from ATCC, Manassas, VA). PSK or control PBS treatment was started at 10 days after the injection when tumors just became palpable. PSK was dissolved in PBS and given via oral gavage in 200 µl volume. Mice in the control group received oral gavage of PBS of the same volume. Tumors were measured every other day with Vernier calipers and tumor volume was calculated as the product of length × width × height × 0.5236. In vivo data are presented as mean±sem. In some experiments, mice were depleted of specific lymphocytes (CD4+, CD8+ T cells, or NK cells) during PSK treatment using standard procedure as described in our previous publication (19).
Evaluation of IL-12 production by DC using intracellular cytokine staining
Mesenteric and tumor draining lymph nodes were collected from control or PSK-treated mice. The lymph nodes were minced over a 70 µm cell strainer and washed in RPMI. Then the lymph node cells were stimulated with phorbol myristate acetate (50 ng/ml) and ionomycin (1 µM) for 16 hours in the presence of brefeldin A (10 µg/ml) before staining, as has been previously described (20). Cells were first stained with antibodies against surface antigen CD11c, then fixed and permeabilized with Perm/Fix solution (eBioscience). The cells were then stained with anti-IL-12-PE (clone 17.8, eBioscience). Samples were acquired on a FACS Canto analyzer and data was analyzed using FlowJo.
Measuring tumor-specific T cells using Enzyme-linked immunospot (ELISPOT) assay
IFN-γ ELISPOT assay was used to determine the frequencies of tumor-specific T cells in splenocytes from PSK and control PBS-treated mice using methods similarly as previously described (21). Splenocytes (200,000 cells/well) were stimulated in 6 well replicates using irradiated syngeneic tumor cells (MMC) or ConA (10 ng/ml) as positive control. The plates were cultured at 37°C in 5% CO2 for two days. On day 3, the cells were removed and addition of secondary antibody and plate development were carried out similarly as previously described (21). Dried plates were read on an ELISPOT reader (Cell Technology, Columbia, MD).
Evaluation of NK lytic activity using flow cytometry
Splenocytes from PSK or control PBS treated mice were isolated and tested for NK cell lytic activity against NK sensitive YAC-1 tumor target cells by a standard flow cytometry assay. YAC-1 cells were labeled with 3,3’-Dioctadecyloxacarbocyanine [DiOC18(3)] (Sigma, St. Louis, MO) and then cultured for 4 hours with splenocytes from PSK or PBS-treated mice in triplicate wells at 3 different E:T ratios (50:1, 25:1, and 12.5:1). At the end of 4 hour incubation, cells were harvested and stained with propidium iodide (PI) and washed. Dead target cells were detected as PI+DiOC3+ cells by flow cytometry. NK cell activity, defined as percent cytotoxicity of each sample, was calculated at each E:T ratio using the following formula: (%DiOC+, PI+ cells) Splenocytes+YAC-1 − (%DiOC+, PI+ cells) YAC-1 alone Lytic Unitis (LU) values were extrapolated from dose-response curves of percent specific lysis vs. log E:T ratio for each blood sample assayed using a software program provided by Dr. Theresa L. Whiteside, University of Pittsburgh School of Medicine (22, 23). Lytic units of NK cell activity, defined as the number of cells required to cause 20% target cell lysis relative to 107 effector cells, were determined by the equation: 107 / LU20.
Real time Reverse Transcription-PCR
Total RNA from PSK or control PBS-treated tumors was isolated using RNA4Aqueous kit (Ambion). The integrity of RNA was tested using an Agilent BioAnalyzer (Foster City, CA). Reverse transcription and real time PCR analysis was done similarly as previously described (17). Primer and probes for CD4 and CD8 were purchased from Applied Biosystems (Foster City, CA). Data analysis was performed using SDS 2.21 (Applied Biosystems). The mRNA expression level of the target gene was normalized to β-actin using the ΔCT method. Level of expression=2−ΔCT, where ΔCT=CT target gene−CT actin. CT is the cycle threshold at which the fluorescence signal crosses an arbitrary value.
Statistical analysis
Statistical analysis was performed using GraphPad (GraphPad Software, San Diego, CA). Data were analyzed using the two-tailed Student’s t test or ANOVA. A value of p<0.05 was considered statistically significant.
Results
PSK treatment stimulates T cell proliferation and Th1 cytokine secretion and induces DC maturation and IL-12 secretion
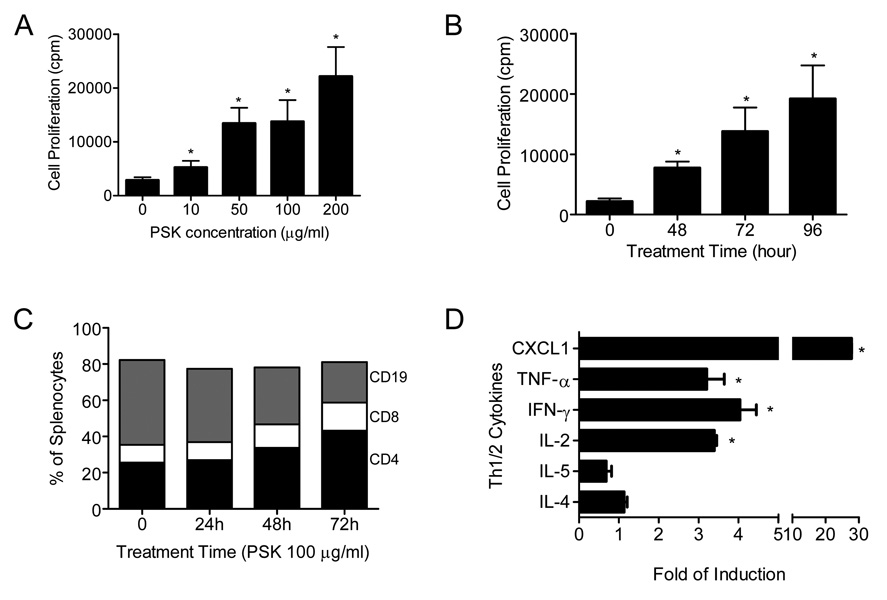
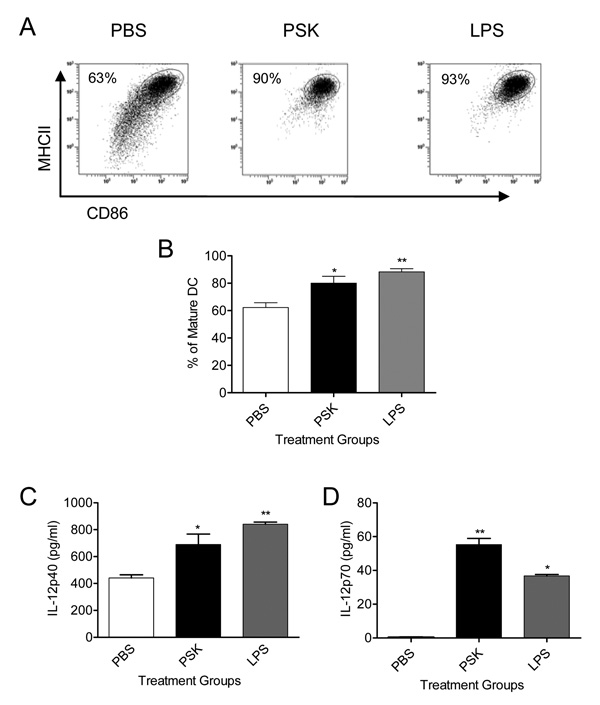
PSK treatment (10–200 µg/ml, 48–96 hours) significantly stimulated the proliferation of splenocytes in a dose- (Fig. 1A) and time-dependent manner (Fig. 1B). PSK treatment increased the percentages of CD4+ (25.5±1.5% in control vs. 43.2±3.9% after 72h PSK at 100 µg/ml, p=0.01) and CD8+ T cells (9.9±0.5% vs. 15.5±0.5%, p=0.0015) among total splenocytes and reduced the percentage of B cells (46.8±0.6% vs. 22.4±1.9%, p=0.0003) (Fig. 1C). B cell number also decreased, consistent with previous publication that PSK inhibits B cell growth (24). PSK treatment (10–200 µg/ml, 48–96 hours) also induced secretion of Th1 cytokines in a dose and time-dependent manner. After 96 h of PSK treatment (100 µg/ml), the level of IFN-γ was increased by 4.03±0.41 fold (p=0.001 from control). TNF-α was induced by 3.21±0.44 fold (p=0.0043 from control). IL-2 was induced by 3.40±0.06 fold (p=0.0002 from control). The levels of IL-4 and IL-5 were no different from controls (p=0.22, and 0.11 respectively) (Fig. 1D). None of the innate immune subsets we tested (monocytes (CD14+), macrophage (F4/80+), and DC (CD11c+)) was increased among total splenocytes after in vitro PSK treatment (p>0.05 as compared to control). Although the number of CD11c+ cells was not increased after PSK treatment, we questioned whether the phenotype and functional capacity of DC was impacted by PSK. Using BMDC, we found that PSK treatment (200 µg/ml, 48h) resulted in increased percentage of mature DC that that are CD86+MHCIIhigh (62.3±3.4% in PBS vs. 80.1±5.0% in PSK group, p=0.04) (Figs. 2A–B). PSK-treated DC also secreted significantly greater levels of IL-12p40 (441±24 pg/ml in PBS group vs. 689±78 pg/ml in PSK group, p=0.03) (Fig. 2C), and IL-12p70 (0.4±0.1 pg/ml in PBS vs. 55.3±3.6 pg/ml in PSK group, p<0.001) than controls (Fig. 2D).
Figure 1. PSK stimulates splenocyte proliferation and secretion of Th1 cytokines.
(A) Dose of PSK on the horizontal axis and cell proliferation in cpm on the vertical axis. * indicate where values were significantly different from control, p<0.05. The bars represent the mean±sem of triplicate wells in each treatment group. Similar results were observed from two independent experiments. (B) Time course of PSK-stimulated splenocyte proliferation. The bars represent the mean±sem of triplicate wells in each treatment group. *, significantly different from control, p<0.05. Similar results were observed from more than two independent experiments. (C) Shown are percentages of CD4+ (black bar), CD8+ (white bar), and CD19+ cells (grey bar) among total splenocytes at various treatment times (X axis). Values shown are representative of three replicates. (D) The columns represent the fold of induction in PSK-treated samples over untreated control for each cytokine. Shown is the mean±sem of duplicate wells in each treatment group. The experiment was repeated three times with similar results. *, p<0.05.
Figure 2. In vitro PSK treatment activates DC maturation and secretion of IL-12.
(A) Representative flow graphs of CD11c+ DC from PBS, PSK, and LPS-treated BMDC stained with anti-CD86 and anti-MHCII. The number in each graph indicates the percentage of mature DC (CD86+MHCIIhigh) in each sample. (B) The columns represents mean±sem of the percentage of mature DC in BMDC treated with PBS (white column), PSK (black column), and LPS (grey column); *, p<0.05; **, p<0.01. Similar results were observed in three independent experiments. (C–D) The columns represents mean±sem of the levels of IL-12p40 and IL-12p70 in culture supernatant of BMDC treated with PBS (white column), PSK (black column), and LPS (grey column); *, p<0.05; **, p<0.01. Similar results were observed in three independent experiments.
PSK is a selective TLR2 agonist and the Type I inflammatory response induced by PSK is dependent on TLR2 activation
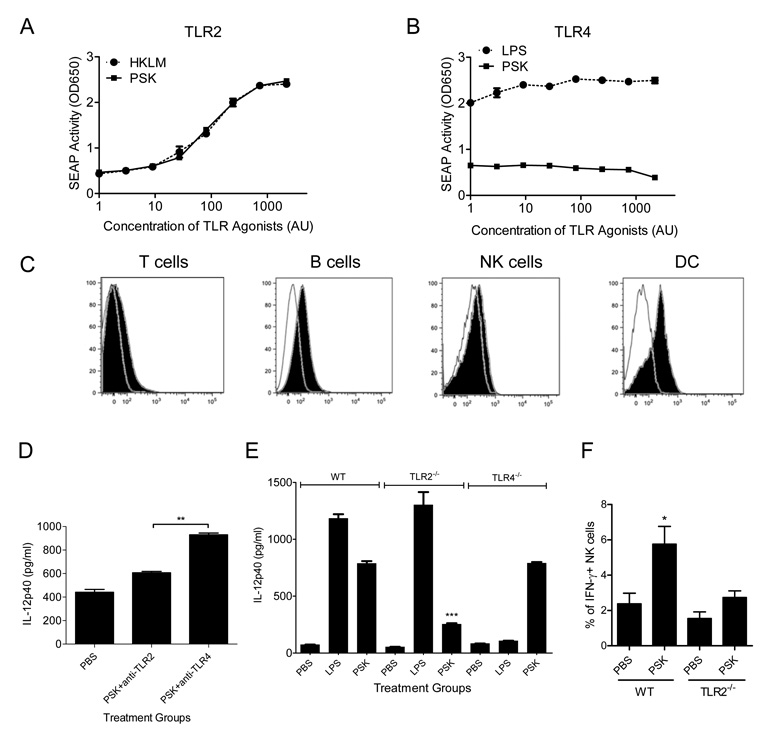
It has been shown that fungal pathogens can activate TLRs (25) so we questioned whether PSK, which is a fungal product, may induce type I immunity via TLR activation. PSK specifically activates TLR2 in a dose-dependent manner and demonstrated no activity against TLR 3, 4, 5, 7, 8 or 9 (Fig. 3A, B and Supplemental Figure 1). Evaluation of TLR2 expression in different subsets of splenocytes from neu transgenic mice showed that TLR2 is expressed at non-detectable or very low levels in CD3+ T cells and NK1.1+ NK cells. The expression was detectable in CD19+ B cells, and highly expressed in CD11c+ DC (Fig. 3C). TLR2 was not expressed in tumor cells from neu transgenic mice (data not shown). Pre-incubation with an anti-TLR2 mAb but not an anti-TLR4 mAb inhibited PSK-induced IL-12p40 production by BMDC (p<0.0001) (Fig. 3D). BMDC from TLR2−/− mice, when stimulated with PSK, secreted significantly less IL-12p40 compared to BMDC from WT or TLR4−/− mice (254±8 pg/ml vs. 787±21 pg/ml and 790±10 pg/ml, p<0.0001, Fig. 3E). Similarly, splenocytes from TLR2−/− mice did not secrete TNF-α upon PSK stimulation (Supplemental Figure 2). In vitro PSK stimulates NK cells from WT mice but not from TLR2−/− mice to secrete IFN-γ (Fig. 3F).
Figure 3. PSK selectively activates TLR2 and the stimulatory effect of PSK on DC is dependent on TLR2 activation.
(A–B) Shown are SEAP activity (Y-axis) in the culture supernatant of TLR2- and TLR4-transfected HEK-293 cells when stimulated with serial dilutions of PSK (0.5–1500 µg/ml, solid line with ■) or the positive control TLR agonists (HKLM for TLR2, and LPS for TLR4, shown as dotted line with ●). Each data point represents the mean±sem of triplicate culture wells at each concentration. Arbitrary units (AU): PSK 1 unit = 0.5 µg/ml; HKLM 1 unit = 4500 cells; LPS 1 unit = 0.05 ng/ml. Similar results were obtained from more than three experiments. (C) Histograms showing the expression of TLR2 in T cells, B cells, NK cells, and DC from neu transgenic mice. The filled histogram represents cells stained with anti-TLR2-PE; the unfilled histogram represents cells stained with an isotype control antibody. Experiments were repeated twice with similar results. (D) Shown are IL-12p40 levels (mean±sem) in BMDC isolated from neu transgenic mice pre-treated with anti-TLR2 or anti-TLR4 monoclonal antibody (10 µg/ml) for 1 hour prior to PSK treatment (100 µg/ml for 48 hours). **, p<0.01. (E) The columns represent average IL-12p40 levels (mean±sem) in PBS, PSK, or LPS-treated DC from WT, TLR2−/−, or TLR4−/− mice. ***, p <0.001 compared to PSK treatment group in WT. Experiments were repeated twice with similar results. (F) Shown are percentages of IFN-γ-positive NK cells in splenocytes from WT and TLR2−/− mice treated with PSK (100 µg/ml, 24 hour) or control PBS. *, p<0.05 from PBS control. Results are representative of 3 independent measurements.
Oral PSK administration significantly inhibits the growth of both implanted and spontaneous breast tumors in neu transgenic mice
PSK was administered via oral gavage to neu transgenic mice bearing implanted or spontaneous tumors. As shown in Figure 4, PSK treatment significantly inhibits the growth of both tumors. In the implant model, the tumor size after 3 weeks of treatment was 574±26mm3 in the PSK group and 1174±41mm3 in the PBS group (p<0.0001). In the spontaneous tumor setting, the tumor size after 3 weeks of treatment was 95±39mm3 in PSK group and 825±154mm3 in PBS group (p=0.0006). We have previously reported that spontaneous tumors are different from implanted tumors in these neu transgenic mice because spontaneous tumors grow slower, have more infiltrating immune cells, are more immunogenic, and usually responded better to immunotherapy (17, 19). However, since the mice don’t develop spontaneous tumors until approximately 5 months old, the implant model is still frequently used, especially when large number of mice is required.
Figure 4. Oral PSK inhibits the growth of implanted and spontaneous breast tumors in neu transgenic mice.
Shown are tumor growth curves in mice bearing implanted tumor (A) or spontaneous tumors (B) treated with PSK (●) or control PBS (□). Each data point represents the average tumor size (mean±sem) in each group (n=14/group for implanted tumor and n=13/group for spontaneous tumor). Results shown are representative of three independent experiments.
Oral PSK administration augments both T cell and NK cell activity and the anti-tumor effect of PSK is dependent on CD8+ T cells and NK cells and is mediated by TLR2
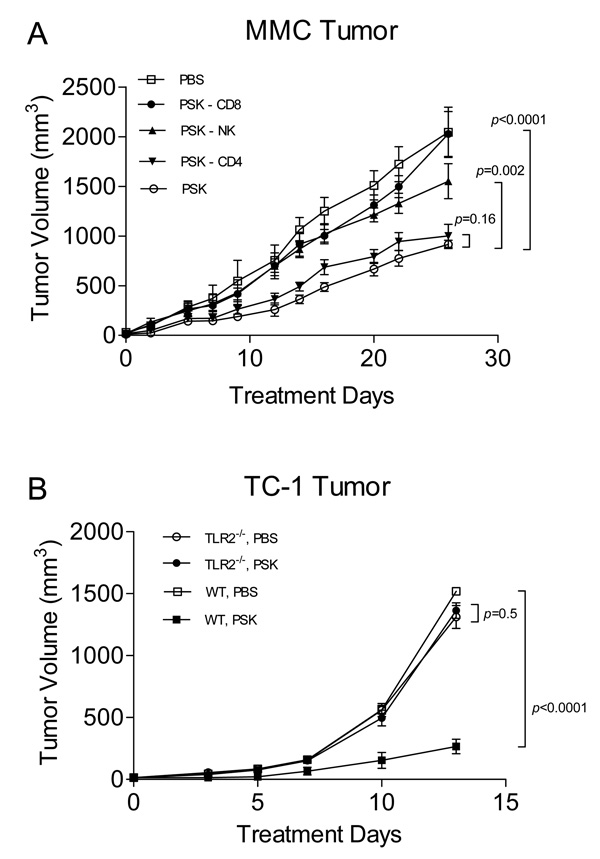
Oral PSK induced IL-12 secretion from DC in both local mesenteric LN (mLN, 1.3±0.3% vs. 3.5±0.9% IL-12+ DC, p=0.03) and DC in tumor draining LN (TDLN) (0.4±0.2% vs. 2.3±0.6% IL-12+ DC, p=0.04). Systemically, PSK not only increased the percentages of CD4+ (28.1±2.5% vs. 36.6±2.7%, p=0.04) and CD8+ T cells (7.5±0.6% vs. 9.6±0.4%, p=0.02) among total splenocytes in vivo, but augmented the number of tumor-specific T cells (37±21 vs. 160±32 tumor-specific T cells per million splenocytes, p=0.03, Fig. 5A). In addition to T cells, PSK-treated mice also demonstrate augmented NK cell activity as evidenced by increased lysing of YAC-1 tumor cells (1.6±0.5 LU vs. 9.8±2.0 LU, p=0.01, Fig. 5B). Evaluation of tumor infiltrating lymphocytes showed a significantly increased ratio of CD8/CD4 T cells at both the mRNA and protein level in PSK-treated mice (p=0.014 by RT-PCR and p=0.04 by FACS as compared to control, Fig. 5C–D). The percentage of CD4+Foxp3+ T regulatory cells among total TIL decreased from 2.73±0.60% to 1.02±0.16% in PSK-treated mice (p=0.01, Fig. 5E). To determine the role of different immune subsets in the anti-tumor effect of PSK, we selectively depleted CD4+, CD8+ T cells or NK cells during PSK treatment. As shown in Fig. 6A, selective depletion of CD8+ T cells and NK cells, but not CD4+ T cells, significantly inhibited the anti-tumor effect of PSK in mice with implanted breast tumors. Both NK cells and CD8 T cells are required as depletion of both sets during PSK treatment resulted in larger tumor than depleting either set alone (data not shown). To investigate whether the anti-tumor effect of PSK is mediated by TLR2 activation, we implanted the same amount of TC-1 tumor cells into TLR2 knockout mice and WT C57BL/6 mice. Then we treated the tumor-bearing TLR2−/− mice or WT mice with oral PSK or control PBS. As shown in Fig. 6B, PSK significantly inhibited tumor growth in WT mice (p<0.0001 between PBS and PSK group), but not in TLR2−/− mice (p=0.5 between PBS and PSK group), indicating that TLR2 is critical in mediating the anti-tumor effect of PSK.
Figure 5. Oral PSK augments T cells and NK cells in spleen of PSK-treated mice and increases CD8/CD4 ratio in TIL.
(A) Shown are numbers of IFN-γ-secreting tumor specific T cells (mean±sem) per million splenocytes in PBS (white column)- or PSK (black column)-treated mice (n=3/group). (B) Shown is NK activity (LU20) in splenocytes isolated from PBS (white column)- or PSK (black column)-treated mice (n=4–5/group). (C) The ratio of CD8/CD4 mRNA expression in tumors from PBS (white column)- or PSK (black column)-treated mice (n=4–5/group). (D) The ratio of CD8+/CD4+ T cells in TIL from PBS (white column)- or PSK (black column)-treated mice (n=4/group). (E) The percentage of T regulatory cells (CD4+Foxp3+) among total TIL in PBS (white column)- or PSK (black column)-treated mice (n=5–6/group). *, p<0.05. All results were repeated in two independent experiments.
Figure 6. The anti-tumor effect of PSK is dependent on CD8+ T cells and NK cells, and is mediated by TLR2.
(A) Selective depletion of CD8+ T cells or NK cells but not CD4+ T cells abolished the anti-tumor effect of PSK. Shown are the growth curves of implanted MMC tumors in neu transgenic mice having received PBS (□), PSK (○), PSK with CD4 depletion (▼), PSK with CD8 depletion (●), or PSK with NK depletion (▲). Data represent 5 mice in each treatment group. Similar results were observed in two independent experiments. (B) PSK inhibits the growth of implanted TC-1 tumors in WT C57BL/6 mice but not in TLR2−/− mice. Shown are the growth curves of implanted TC-1 tumors in WT mice receiving PBS (□), WT mice receiving PSK (■), TLR2−/− mice receiving PBS (○), and TLR2−/− mice receiving PSK (●). N=5 in each group.
Discussion
In the current study we have demonstrated that PSK is a potent and selective TLR2 agonist. Moreover, PSK treatment induces type I T cells potentially via its effect on the DC phenotype. Finally the anti-tumor effects observed with PSK treatment are dependent on both T cell and NK activity.
Data presented here is the first evidence that PSK selectively activates TLR2. TLRs are a family of evolutionarily conserved pathogen recognition receptors which play a pivotal role in host defense by regulating both innate and adaptive immune responses (26, 27). TLR agonists have been tested intensively in tumor immunotherapy in recent years and almost all of the studies exploring the anti-tumor effect of TLR agonists have focused on the ligands for TLR3, −7, −8, and −9 (28–30). TLR2 is a transmembrane protein receptor and can form a heterodimer with TLR1 or TLR6. The expression of TLR2 on T cells is shown to be up-regulated following T-cell activation and can act as a costimulatory receptor (31). Recently it has been found that this co-stimulation via TLR-2 is more responsible for proliferation and survival of CD8+ T cells than for that of CD4+ T cells (32). It has also been reported that TLR2 engagement on CD8+ T cells enables generation of functional memory cells in response to a suboptimal TCR signal, such as that seen against self tumor antigens (33). Moreover, engagement of TLR1/2 on ova-specific OT-1 CTLs increased cell proliferation and the expression of various effector molecules on T cells (34). These previous reports concerning TLR2 activation are consistent with our finding that the ratio of CD8/CD4 in TIL increased in PSK-treated mice (Fig. 5) and CD8+ T cells, together with NK cells, mediate the anti-tumor effect of PSK. In addition to the effect on CD8+ T cells, recent literature suggests that TLR2 can abolish the suppressive capacity of T regulatory cells or make effector T cells resistant to the suppression of T regulatory cells (35, 36). We observed a decrease in T regulatory cells in tumor after PSK treatment, which could also contributed to the anti-tumor effect of PSK.
The finding that TLR2 is minimally expressed on T cells but highly expressed on DC (Fig. 3C) suggests that the effect of PSK on T cells could be indirect via activation of DC, secretion of IL-12, and the polarizing of a tumor specific Th1 response. The ability of TLR agonists to augment anti-tumor immunity via stimulation of DC has been well described (37–39). For example, it has been shown that TLR8 primed DC can generate high avidity antitumor T cells via IL-12 production (37). Ligation of TLR9 by CpG converts tolerogenic DC into antigen presenting cells capable of stimulating antitumor immunity via activating Th1/Th17 and NK cell response (38). Our results suggest the potential of using PSK, a natural product with a demonstrated favorable safety profile, to augment anti-tumor immunity via stimulating DC. A recent study showed that a combination of 3 TLR ligands (TLR2/6, TLR3, and TLR9) greatly enhanced IL-15 production from DC and increased the generation of high avidity T cells after vaccination (40). Whether combining PSK with other TLR agonists will have enhanced anti-tumor effect remains to be investigated.
NK cells are also activated by PSK treatment and play an important role in the anti-tumor activity of PSK. It is noted that TLR2 expression on NK cells is very low, although significantly higher than the expression on T cells. Thus, the question remains whether the activation of NK cells by PSK is via direct activation of TLR2 on NK cells or indirect via activation of antigen presenting cells. It is reported that NK cell priming requires the presence of CD11chigh DC (41). However, direct TLR2 signaling on NK cells has also been reported (42). The cross talk between NK cells and DC has also been well described (43, 44). The finding that NK cells are activated by PSK indicates the potential of using this natural product to enhance the therapeutic effect of HER2-targeted monoclonal antibody (mAb) therapy by trastuzumab, which is currently a standard of care for patients with HER2 overexpressing breast cancer. The major mechanism of the anti-tumor effect of trastuzumab is antibody-dependent cell-mediated cytotoxicity (ADCC) in which the tumor cells are coated with the mAb and lysed by NK cells via binding of the Fc receptor. NK cell-stimulatory cytokines, such as IL-12, and IL-21, have been shown to enhance ADCC (45). The potential of using TLR agonists to enhance ADCC has also been suggested in publications (46–48). Our results suggest the potential of using PSK to augment the therapeutic effect of trastuzumab in breast cancer patients. Preliminary analysis using human PBMC showed that PSK has similar stimulatory effect on human immune cells and augments the ability of NK cell to lyse tumor targets (Lu et al, unpublished data).
It is noted that PSK-induced IL-12 production from BMDC was not completed abrogated in TLR2−/− mice. Thus it is possible that receptors other than TLR2 may also be stimulated by PSK and have contributed to IL-12 production in the knockout mice. It has been reported that C-type lectins such as dectin-1 and dectin-2 are involved in recognition of some fungal pathogens (49, 50). Whether PSK could also activate these lectin receptors remains to be investigated in future studies.
In summary, results from the current study demonstrate that PSK is a selective TLR2 agonist. The effect of PSK on DC and T cells is dependent on TLR2 activation. Oral PSK inhibits breast cancer growth in neu transgenic mice and the anti-tumor effect is dependent on both CD8+ T cells and NK cells. Results from this study elucidate the mechanism of action of this mushroom based natural product and may lead to more effective methods of therapeutically exploiting the anti-tumor effects of PSK.
Translational Relevance
It has been reported that more than half of cancer patients have tried both conventional and complementary and alternative medicine (CAM) to combat their disease, yet the mechanism of CAM therapies remain poorly understood. In this study, we demonstrated that polysaccharide krestin (PSK), a highly purified mushroom extract, is a potent and selective TLR2 agonist. PSK activates dendritic cells (DC) and T cells in a TLR2-dependent manner. In vivo administration of PSK in a mouse model of breast cancer has potent anti-tumor effect that is dependent on CD8+ T cells and NK cells. PSK is a natural product with a proven safety profile. Results from this study provide important information for future clinical trials testing the anti-tumor potential of this novel TLR2 agonist.
Supplementary Material
Acknowledgement
This work was supported by NIH grants R01CA138547, R01AT004314, and U19AT001998.
Abbreviations
- ADCC
antibody-dependent cell-mediated cytotoxicity
- CAM
complementary and alternative medicine
- BM
bone marrow
- BMDC
bone marrow derived dendritic cells
- CTL
cytotoxic T lymphocyte
- DC
dendritic cells
- DiOC18(3)
3,3’-Dioctadecyloxacarbocyanine
- ELISA
Enzyme-linked immunosorbant assay
- ELISPOT
Enzyme-linked immunospot assay
- FBS
Fetal bovine serum
- HEK
human embryonic kidney cells
- HKLM
heat killed listeria monocytogens
- IFN-γ
interferon gamma
- IL
interleukin
- LPS
lipopolysaccharide
- LU
lytic unit
- mAb
monoclonal antibody
- MLN
Mesenteric lymph node
- PI
propidium iodide
- PSK
Polysaccharide Krestin
- SEAP
secretory alkaline phosphatase
- TDLN
Tumor draining lymph node
- TGF-β
Transforming growth factor beta
- TIL
tumor infiltrating lymphocyte
- TLR
Toll-like receptor
- TNF-α
Tumor necrosis factor alpha
- Treg
T regulatory cell
Reference
- 1.Eisenberg DM, Davis RB, Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA. 1998;280(18):1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 2.Richardson MA, Sanders T, Palmer JL, Greisinger A, Singletary SE. Complementary/alternative medicine use in a comprehensive cancer center and the implications for oncology. J Clin Oncol. 2000;18(13):2505–2514. doi: 10.1200/JCO.2000.18.13.2505. [DOI] [PubMed] [Google Scholar]
- 3.Eisenberg DM, Kessler RC, Foster C, Norlock FE, Calkins DR, Delbanco TL. Unconventional medicine in the United States. Prevalence, costs, and patterns of use. N Engl J Med. 1993;328(4):246–252. doi: 10.1056/NEJM199301283280406. [DOI] [PubMed] [Google Scholar]
- 4.Kidd PM. The use of mushroom glucans and proteoglycans in cancer treatment. Altern Med Rev. 2000;5(1):4–27. [PubMed] [Google Scholar]
- 5.Deng G, Lin H, Seidman A, et al. A phase I/II trial of a polysaccharide extract from Grifola frondosa (Maitake mushroom) in breast cancer patients: immunological effects. J Cancer Res Clin Oncol. 2009;135(9):1215–1221. doi: 10.1007/s00432-009-0562-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fisher M, Yang LX. Anticancer effects and mechanisms of polysaccharide-K (PSK): implications of cancer immunotherapy. Anticancer Res. 2002;22(3):1737–1754. [PubMed] [Google Scholar]
- 7.Sullivan R, Smith JE, Rowan NJ. Medicinal mushrooms and cancer therapy: translating a traditional practice into Western medicine. Perspect Biol Med. 2006;49(2):159–170. doi: 10.1353/pbm.2006.0034. [DOI] [PubMed] [Google Scholar]
- 8.Nakazato H, Koike A, Saji S, Ogawa N, Sakamoto J. Efficacy of immunochemotherapy as adjuvant treatment after curative resection of gastric cancer. Study Group of Immunochemotherapy with PSK for Gastric Cancer. Lancet. 1994;343(8906):1122–1126. doi: 10.1016/s0140-6736(94)90233-x. [DOI] [PubMed] [Google Scholar]
- 9.Oba K, Teramukai S, Kobayashi M, Matsui T, Kodera Y, Sakamoto J. Efficacy of adjuvant immunochemotherapy with polysaccharide K for patients with curative resections of gastric cancer. Cancer Immunol Immunother. 2007;56(6):905–911. doi: 10.1007/s00262-006-0248-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torisu M, Hayashi Y, Ishimitsu T, et al. Significant prolongation of disease-free period gained by oral polysaccharide K (PSK) administration after curative surgical operation of colorectal cancer. Cancer Immunol Immunother. 1990;31(5):261–268. doi: 10.1007/BF01740932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ohwada S, Ikeya T, Yokomori T, et al. Adjuvant immunochemotherapy with oral Tegafur/Uracil plus PSK in patients with stage II or III colorectal cancer: a randomised controlled study. Br J Cancer. 2004;90(5):1003–1010. doi: 10.1038/sj.bjc.6601619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sakamoto J, Morita S, Oba K, et al. Efficacy of adjuvant immunochemotherapy with polysaccharide K for patients with curatively resected colorectal cancer: a meta-analysis of centrally randomized controlled clinical trials. Cancer Immunol Immunother. 2006;55(4):404–411. doi: 10.1007/s00262-005-0054-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hayakawa K, Mitsuhashi N, Saito Y, et al. Effect of krestin (PSK) as adjuvant treatment on the prognosis after radical radiotherapy in patients with non-small cell lung cancer. Anticancer Res. 1993;13(5C):1815–1820. [PubMed] [Google Scholar]
- 14.Kato M, Hirose K, Hakozaki M, et al. Induction of gene expression for immunomodulating cytokines in peripheral blood mononuclear cells in response to orally administered PSK, an immunomodulating protein-bound polysaccharide. Cancer Immunol Immunother. 1995;40(3):152–156. doi: 10.1007/BF01517346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hirai R, Oguchi Y, Sugita N, Matsunaga K, Nomoto K. Enhancement of T-cell proliferation by PSK. Int J Immunopharmacol. 1993;15(6):745–750. doi: 10.1016/0192-0561(93)90147-q. [DOI] [PubMed] [Google Scholar]
- 16.Harada M, Matsunaga K, Oguchi Y, et al. Oral administration of PSK can improve the impaired anti-tumor CD4+ T-cell response in gut-associated lymphoid tissue (GALT) of specific-pathogen-free mice. Int J Cancer. 1997;70(3):362–372. doi: 10.1002/(sici)1097-0215(19970127)70:3<362::aid-ijc19>3.0.co;2-h. [DOI] [PubMed] [Google Scholar]
- 17.Lu H, Knutson KL, Gad E, Disis ML. The tumor antigen repertoire identified in tumor-bearing Neu transgenic mice predicts human tumor antigens. Cancer Res. 2006;66(19):9754–9761. doi: 10.1158/0008-5472.CAN-06-1083. [DOI] [PubMed] [Google Scholar]
- 18.Knutson KL, Lu H, Stone B, et al. Immunoediting of cancers may lead to epithelial to mesenchymal transition. J Immunol. 2006;177(3):1526–1533. doi: 10.4049/jimmunol.177.3.1526. [DOI] [PubMed] [Google Scholar]
- 19.Lu H, Wagner WM, Gad E, et al. Treatment failure of a TLR-7 agonist occurs due to self-regulation of acute inflammation and can be overcome by IL-10 blockade. J Immunol. 2010;184(9):5360–5537. doi: 10.4049/jimmunol.0902997. [DOI] [PubMed] [Google Scholar]
- 20.Kryczek I, Banerjee M, Cheng P, et al. Phenotype, distribution, generation, and functional and clinical relevance of Th17 cells in the human tumor environments. Blood. 2009;114(6):1141–1149. doi: 10.1182/blood-2009-03-208249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park KH, Gad E, Goodell V, et al. Insulin-like growth factor-binding protein-2 is a target for the immunomodulation of breast cancer. Cancer Res. 2008;68(20):8400–8409. doi: 10.1158/0008-5472.CAN-07-5891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bryant J, Day R, Whiteside TL, Herberman RB. Calculation of lytic units for the expression of cell-mediated cytotoxicity. J Immunol Methods. 1992;146(1):91–103. doi: 10.1016/0022-1759(92)90052-u. [DOI] [PubMed] [Google Scholar]
- 23.Whiteside TL, Bryant J, Day R, Herberman RB. Natural killer cytotoxicity in the diagnosis of immune dysfunction: criteria for a reproducible assay. J Clin Lab Anal. 1990;4(2):102–114. doi: 10.1002/jcla.1860040207. [DOI] [PubMed] [Google Scholar]
- 24.Liu A, Arbiser JL, Holmgren A, Klein G, Klein E. PSK and Trx80 inhibit B-cell growth in EBV-infected cord blood mononuclear cells through T cells activated by the monocyte products IL-15 and IL-12. Blood. 2005;105(4):1606–1613. doi: 10.1182/blood-2004-06-2406. [DOI] [PubMed] [Google Scholar]
- 25.Netea MG, Gow NA, Munro CA, et al. Immune sensing of Candida albicans requires cooperative recognition of mannans and glucans by lectin and Toll-like receptors. J Clin Invest. 2006;116(6):1642–1650. doi: 10.1172/JCI27114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wang RF, Peng G, Wang HY. Regulatory T cells and Toll-like receptors in tumor immunity. Semin Immunol. 2006;18(2):136–142. doi: 10.1016/j.smim.2006.01.008. [DOI] [PubMed] [Google Scholar]
- 27.Pandey S, Agrawal DK. Immunobiology of Toll-like receptors: Emerging trends. Immunol Cell Biol. 2006;84(4):333–341. doi: 10.1111/j.1440-1711.2006.01444.x. [DOI] [PubMed] [Google Scholar]
- 28.Schon MP, Schon M. TLR7 and TLR8 as targets in cancer therapy. Oncogene. 2008;27(2):190–199. doi: 10.1038/sj.onc.1210913. [DOI] [PubMed] [Google Scholar]
- 29.Krieg AM. Therapeutic potential of Toll-like receptor 9 activation. Nat Rev Drug Discov. 2006;5(6):471–484. doi: 10.1038/nrd2059. [DOI] [PubMed] [Google Scholar]
- 30.Rakoff-Nahoum S, Medzhitov R. Toll-like receptors and cancer. Nat Rev Cancer. 2009;9(1):57–63. doi: 10.1038/nrc2541. [DOI] [PubMed] [Google Scholar]
- 31.Komai-Koma M, Jones L, Ogg GS, Xu D, Liew FY. TLR2 is expressed on activated T cells as a costimulatory receptor. Proc Natl Acad Sci U S A. 2004;101(9):3029–3034. doi: 10.1073/pnas.0400171101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lee SM, Joo YD, Seo SK. Expression and Function of TLR2 on CD4 Versus CD8 T Cells. Immune Netw. 2009;9(4):127–132. doi: 10.4110/in.2009.9.4.127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mercier BC, Cottalorda A, Coupet CA, Marvel J, Bonnefoy-Berard N. TLR2 engagement on CD8 T cells enables generation of functional memory cells in response to a suboptimal TCR signal. J Immunol. 2009;182(4):1860–1867. doi: 10.4049/jimmunol.0801167. [DOI] [PubMed] [Google Scholar]
- 34.Asprodites N, Zheng L, Geng D, Velasco-Gonzalez C, Sanchez-Perez L, Davila E. Engagement of Toll-like receptor-2 on cytotoxic T-lymphocytes occurs in vivo and augments antitumor activity. Faseb J. 2008;22(10):3628–3637. doi: 10.1096/fj.08-108274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Oberg HH, Ly TT, Ussat S, Meyer T, Kabelitz D, Wesch D. Differential but direct abolishment of human regulatory T cell suppressive capacity by various TLR2 ligands. J Immunol. 2010;184(9):4733–4740. doi: 10.4049/jimmunol.0804279. [DOI] [PubMed] [Google Scholar]
- 36.Liu H, Komai-Koma M, Xu D, Liew FY. Toll-like receptor 2 signaling modulates the functions of CD4+ CD25+ regulatory T cells. Proc Natl Acad Sci U S A. 2006;103(18):7048–7053. doi: 10.1073/pnas.0601554103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Xu S, Koldovsky U, Xu M, et al. High-avidity antitumor T-cell generation by toll receptor 8-primed, myeloid- derived dendritic cells is mediated by IL-12 production. Surgery. 2006;140(2):170–178. doi: 10.1016/j.surg.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 38.Zhang X, Munegowda MA, Yuan J, Wei Y, Xiang J. Optimal TLR9 signal converts tolerogenic CD4-8- DCs into immunogenic ones capable of stimulating antitumor immunity via activating CD4+ Th1/Th17 and NK cell responses. J Leukoc Biol. 2010;88 doi: 10.1189/jlb.0909633. 000- [DOI] [PubMed] [Google Scholar]
- 39.Zheng R, Cohen PA, Paustian CA, et al. Paired Toll-like receptor agonists enhance vaccine therapy through induction of interleukin-12. Cancer Res. 2008;68(11):4045–4049. doi: 10.1158/0008-5472.CAN-07-6669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Zhu Q, Egelston C, Gagnon S, et al. Using 3 TLR ligands as a combination adjuvant induces qualitative changes in T cell responses needed for antiviral protection in mice. J Clin Invest. 120(2):607–616. doi: 10.1172/JCI39293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Lucas M, Schachterle W, Oberle K, Aichele P, Diefenbach A. Dendritic cells prime natural killer cells by trans-presenting interleukin 15. Immunity. 2007;26(4):503–517. doi: 10.1016/j.immuni.2007.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Martinez J, Huang X, Yang Y. Direct TLR2 signaling is critical for NK cell activation and function in response to vaccinia viral infection. PLoS Pathog. 2010;6(3):e1000811. doi: 10.1371/journal.ppat.1000811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gerosa F, Baldani-Guerra B, Nisii C, Marchesini V, Carra G, Trinchieri G. Reciprocal activating interaction between natural killer cells and dendritic cells. J Exp Med. 2002;195(3):327–333. doi: 10.1084/jem.20010938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Walzer T, Dalod M, Robbins SH, Zitvogel L, Vivier E. Natural-killer cells and dendritic cells: "l'union fait la force". Blood. 2005;106(7):2252–2258. doi: 10.1182/blood-2005-03-1154. [DOI] [PubMed] [Google Scholar]
- 45.Roda JM, Joshi T, Butchar JP, et al. The activation of natural killer cell effector functions by cetuximab-coated, epidermal growth factor receptor positive tumor cells is enhanced by cytokines. Clin Cancer Res. 2007;13(21):6419–6428. doi: 10.1158/1078-0432.CCR-07-0865. [DOI] [PubMed] [Google Scholar]
- 46.Moreno M, Mol BM, von Mensdorff-Pouilly S, et al. Toll-like receptor agonists and invariant natural killer T-cells enhance antibody-dependent cell-mediated cytotoxicity (ADCC) Cancer Lett. 2008;272(1):70–76. doi: 10.1016/j.canlet.2008.06.028. [DOI] [PubMed] [Google Scholar]
- 47.Damiano V, Caputo R, Garofalo S, et al. TLR9 agonist acts by different mechanisms synergizing with bevacizumab in sensitive and cetuximab-resistant colon cancer xenografts. Proc Natl Acad Sci U S A. 2007;104(30):12468–12473. doi: 10.1073/pnas.0705226104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Damiano V, Garofalo S, Rosa R, et al. A novel toll-like receptor 9 agonist cooperates with trastuzumab in trastuzumab-resistant breast tumors through multiple mechanisms of action. Clin Cancer Res. 2009;15(22):6921–6930. doi: 10.1158/1078-0432.CCR-09-1599. [DOI] [PubMed] [Google Scholar]
- 49.Saijo S, Fujikado N, Furuta T, et al. Dectin-1 is required for host defense against Pneumocystis carinii but not against Candida albicans. Nat Immunol. 2007;8(1):39–46. doi: 10.1038/ni1425. [DOI] [PubMed] [Google Scholar]
- 50.Saijo S, Ikeda S, Yamabe K, et al. Dectin-2 recognition of alpha-mannans and induction of Th17 cell differentiation is essential for host defense against Candida albicans. Immunity. 2010;32(5):681–691. doi: 10.1016/j.immuni.2010.05.001. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.