Gangrene
21 likes16,121 views
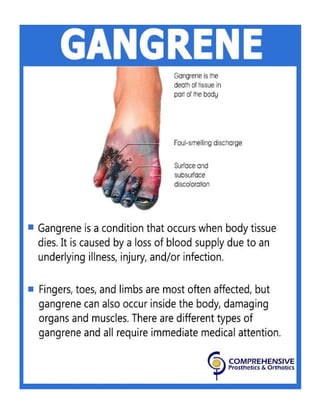
This document has information on gangrene, types of gangrene, symptoms of gangrene and treatment of gangrene,
1 of 7
Downloaded 343 times



Recommended
Oedema new edited by tareq chowdhury, has 30 slides with 40790 views.



Oedema new editedtareq chowdhury
30 slides•40.8K views
Edema is an excessive accumulation of fluid in the interstitial spaces or body cavities. There are several types and causes of edema. Cardiac edema is caused by congestive heart failure which increases venous pressure and hydrostatic pressure, pulling fluid from blood vessels into tissues. Renal edema can be caused by nephritic syndrome which causes salt and water retention, or nephrotic syndrome which decreases plasma protein levels. Hepatic edema manifests as ascites and is caused by portal hypertension or low plasma proteins in conditions like liver cirrhosis. Pulmonary edema can result from left heart failure or inflammation while cerebral edema includes cytotoxic edema from cell injury or vesogenic edema from blood brain barrier disruption.Edema & Haemorrhage by Girish Kumar K, has 30 slides with 5815 views.



Edema & HaemorrhageGirish Kumar K
30 slides•5.8K views
Edema and haemorrhage were presented. Edema is the abnormal accumulation of fluid in tissues, and can be localized or generalized. It can be transudate or exudate depending on protein content. Haemorrhage is bleeding from blood vessels. Bleeding can be arterial, venous, or capillary. Arterial bleeding is bright red and emitted in a jet; venous bleeding is darker and steady; capillary bleeding is bright red and oozing. Bleeding can be primary, reactionary, or secondary depending on timing relative to injury or surgery. The causes, effects, and types of edema and haemorrhage were described.Gas gangrene by Praful SonnePatil, has 16 slides with 22872 views.



Gas gangrenePraful SonnePatil
16 slides•22.9K views
This document discusses gas gangrene, a rapidly spreading, potentially fatal infection caused by Clostridium bacteria. It enters the body through wounds or injuries contaminated with soil or feces and releases toxins that cause tissue death. Symptoms include severe pain, swelling, brownish fluid draining from wounds with a foul odor, skin discoloration, and palpable gas in muscles. Diagnosis involves examining wound fluid under a microscope. Treatment requires urgent debridement of dead tissue, antibiotics like penicillin, oxygen therapy, and possibly amputation of infected limbs to save the patient's life. Homeopathic remedies like Arsenicum, Crotalus, and Secale may provide additional support.Small vessel vasculitis by iyad07, has 52 slides with 4606 views.



Small vessel vasculitisiyad07
52 slides•4.6K views
Wegener's Granulomatosis, Microscopic Polyangiitis, Churg-Strauss syndrome, ANCA, diagnosis, treatment, medications, labs, epidemiology.Gas gangrene 8 - 2- 16 by Durai Ravi, has 18 slides with 52370 views.



Gas gangrene 8 - 2- 16Durai Ravi
18 slides•52.4K views
Gas gangrene is caused by gas-producing bacteria such as Clostridium perfringens infecting crushed or puncture wounds in an anaerobic environment. It leads to localized muscle death and tissue necrosis. Symptoms include pain, fever, and swelling at the wound site with a foul odor. The infection can spread rapidly without prompt treatment which includes intravenous antibiotics, debridement of dead tissue, and possibly amputation of an affected limb. Untreated gas gangrene has high mortality rates due to sepsis and organ failure.Gangrene & amputation by Priyatham Kasaraneni, has 180 slides with 20632 views.



Gangrene & amputationPriyatham Kasaraneni
180 slides•20.6K views
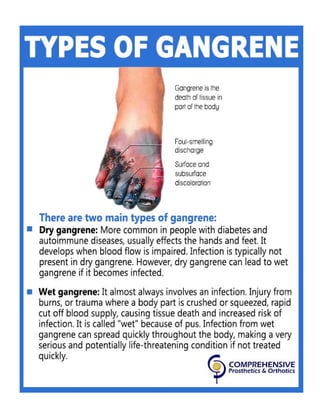
1) Gangrene is defined as macroscopic necrosis of tissues, and can be dry, wet, or gas gangrene. Dry gangrene is caused by reduced blood flow and progresses slowly, while wet gangrene develops rapidly due to blocked blood flow and favors bacterial growth. Gas gangrene is caused by Clostridium bacteria.
2) Amputation involves surgically removing a body extremity and is indicated for conditions like gangrene, trauma, tumors, and vascular insufficiency. The goals are to remove all infected tissue, achieve wound healing, and provide a stump that can accommodate a prosthesis.
3) Factors in determining the amputation level include the zone of injury, adequate tissue margins, circulationLymphangitis by Priya , has 13 slides with 3966 views.



LymphangitisPriya
13 slides•4K views
Lymphangitis is inflammation of lymphatic channels due to infectious or noninfectious causes. Potential pathogens include bacteria, mycobacteria, viruses, fungi, and parasites. Lymphangitis most commonly develops after cutaneous inoculation of microorganisms into the lymphatic vessels through a skin wound or a distal infection complication.Leg ulcers by Harsha Yaramati, has 99 slides with 24043 views.



Leg ulcers Harsha Yaramati
99 slides•24K views
This document discusses different types of leg ulcers including venous, arterial, diabetic neuropathic, and hypertensive ulcers. It provides information on:
1. The causes, risk factors, signs and symptoms, investigations and management for each type of ulcer.
2. Venous ulcers are the most common type, caused by venous insufficiency and reflux, and are typically treated with compression therapy and dressings.
3. Arterial ulcers are caused by peripheral arterial disease and present with dry necrotic wounds, often over bony prominences of the feet. Revascularization may be required for healing.
4. Diabetic and neuropathic ulcers occur due to loss of sensation fromHistory taking - For Surgical patients by Uthamalingam Murali, has 41 slides with 171617 views.



History taking - For Surgical patientsUthamalingam Murali
41 slides•171.6K views
This PPT is based on taking history from surgical patients for UG - Students. ( Based on History taking methods adopted by S.Das )Gangrene by Lazoi Lifecare Private Limited, has 8 slides with 26906 views.



GangreneLazoi Lifecare Private Limited
8 slides•26.9K views
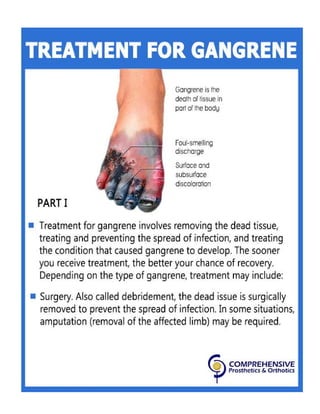
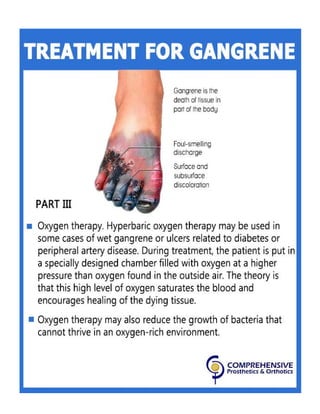
Gangrene occurs when tissues die due to lack of blood flow and oxygen. There are three main types: dry gangrene caused by lack of oxygen, wet gangrene caused by bacterial infection which is more dangerous, and gas gangrene caused by Clostridia bacteria. Symptoms include pain, swelling, discoloration and odor. Treatments depend on the type but may include antibiotics, surgery to improve blood flow, hyperbaric oxygen therapy, debriding dead tissue, and amputation of severely affected body parts.Robbins Basic Pathology - Tissue Repair by King Dietitian, has 18 slides with 8331 views.



Robbins Basic Pathology - Tissue RepairKing Dietitian
18 slides•8.3K views
Tissue repair involves the restoration of tissue architecture and function through regeneration of injured tissue or replacement by connective tissue scarring. It is a complex process that involves cell proliferation, interaction between cells and the extracellular matrix, angiogenesis, fibroblast migration and proliferation, and deposition of new extracellular matrix. Over time, the granulation tissue matures and remodels through synthesis and degradation of extracellular matrix components.Ulcer examination by Bhanwar Sharma, has 29 slides with 18763 views.



Ulcer examinationBhanwar Sharma
29 slides•18.8K views
This document discusses the classification, examination, and characteristics of ulcers. Ulcers can be classified clinically or pathologically, and can be nonspecific, specific, or malignant. During examination of an ulcer, aspects such as size, shape, edge, floor, discharge, and surrounding area should be evaluated. Characteristics such as induration, tenderness, and relations to deeper structures can help determine if an ulcer is healing, spreading, infected, or malignant.Wound healing by drmcbansal, has 58 slides with 57617 views.



Wound healingdrmcbansal
58 slides•57.6K views
The document discusses wound healing and classification. It describes the phases of wound healing as inflammatory, proliferative, and remodeling. The inflammatory phase begins immediately after wounding and lasts 2-3 days, involving vasoactive amines, growth factors, and inflammatory cells. The proliferative phase lasts from days 3 to 3 weeks, involving fibroblast activity, collagen production, angiogenesis, and re-epithelialization. The remodeling phase begins during proliferation and lasts up to 2 years, involving collagen remodeling and maturation. Healing is classified as primary intention for clean wounds or secondary intention for infected wounds. Factors like age, obesity, smoking, and malnutrition can affect wound healing.seminar on Leg swelling & its causes by Biswajit Deka, has 38 slides with 4194 views.



seminar on Leg swelling & its causesBiswajit Deka
38 slides•4.2K views
This document summarizes leg swelling (edema) and its various causes. It begins by defining edema and mechanisms that can cause it like increased capillary permeability or pressure. It then categorizes causes of edema as either central (bilateral) or local (unilateral). Specific conditions that can lead to edema like cardiac failure, nephrotic syndrome, filariasis, and deep vein thrombosis are described. The document provides details on clinical presentations and risk factors for different types of edema.Ulcers Basics by Dr. Valluri Mukesh, has 50 slides with 36568 views.



Ulcers BasicsDr. Valluri Mukesh
50 slides•36.6K views
A Basic Session on Ulcers, Classifications, Types, Clinical Examination, Investigations, Treatment & ManagementEdema by Kanav Bhanot, has 31 slides with 181824 views.



EdemaKanav Bhanot
31 slides•181.8K views
CONTENTS:
GENERAL
NORMAL FLUID CIRCULATION
EDEMA- INTRODUCTION
CAUSES
CLASSIFICATION
MAJOR TYPES
NOTE- Fonts may appear weird because the original fonts are different from the ones visible here.Vascular Ulcers Ppt - by Chukwuma-Ikem Okoye, has 31 slides with 4679 views.



Vascular Ulcers Ppt -Chukwuma-Ikem Okoye
31 slides•4.7K views
This document provides an overview of vascular ulcers, including their classification, etiology, pathophysiology, and management. The main types of vascular ulcers are venous ulcers, arterial ulcers, and mixed arteriovenous ulcers. Venous ulcers are the most common and are usually located over the medial gaiter region of the leg. Arterial ulcers are suggested by diminished or absent peripheral pulses and often have a gray or black wound base. Treatment involves conservative measures like compression therapy for venous ulcers and endovascular procedures or bypass grafts for arterial insufficiency. Proper wound care, infection control, and patient education are important for management.Gas gangrene by DrPoojaPandey4, has 21 slides with 1917 views.



Gas gangreneDrPoojaPandey4
21 slides•1.9K views
Gas gangrene is a life-threatening infection of subcutaneous tissue and muscle caused by clostridial bacteria such as Clostridium perfringens, which release toxins like alpha toxin that cause tissue necrosis. It is associated with wounds, surgery, or trauma and has a rapid onset of symptoms like pain, swelling, crepitus, and gangrenous changes in the skin. Aggressive surgical debridement and antibiotics such as penicillin are needed for treatment to prevent complications like sepsis, shock, and potential limb loss.Necrotizing fasciitis by imagesrl, has 51 slides with 3625 views.



Necrotizing fasciitisimagesrl
51 slides•3.6K views
1) The document summarizes a presentation on a skin-sparing approach to treating necrotizing fasciitis in children.
2) Key aspects of the approach include early and wide debridement of non-viable tissues while preserving viable skin, with a median skin to fascia excision ratio of 0.1.
3) Using this approach in 13 patients, there was no mortality and low morbidity, with no patients requiring skin grafting and a median time to closure of 5 days.Wound and wound healing by Jithin Mampatta, has 73 slides with 35821 views.



Wound and wound healingJithin Mampatta
73 slides•35.8K views
This document provides a summary of wounds and wound healing. It begins with definitions of wounds and various classification systems for wounds based on factors like cleanliness, thickness, involvement of structures, time elapsed, and surgical context. It then discusses the stages and phases of wound healing, including inflammation, proliferation, remodeling and epithelialization. Various factors that can affect wound healing are outlined. Finally, it covers wound management principles and common problems like infection, dehiscence, hypertrophic scarring and keloids.Haemorrhage by Dr. MD. Majedul Islam, has 25 slides with 19136 views.



HaemorrhageDr. MD. Majedul Islam
25 slides•19.1K views
1. Hemorrhage is defined as the escape of blood from blood vessels. It can be classified based on the type of vessel (arterial, venous, capillary), timing (primary, reactionary, secondary), visibility (revealed, concealed), duration (acute, chronic), and type of intervention (surgical, non-surgical).
2. Clinical features depend on the amount and speed of blood loss, and can include increasing pallor, pulse, restlessness, signs of shock like cold skin and reduced urine output. Acute blood loss is monitored through pulse, blood pressure, and urine output.
3. Control techniques include direct pressure, elevation, tourniquets, cauterizationContusions & abrasions by sshssomsen, has 17 slides with 33904 views.



Contusions & abrasionssshssomsen
17 slides•33.9K views
Contusions occur when tissue is injured from blunt force trauma, causing blood vessels to rupture and blood to flow into surrounding tissues. Common causes include contact sports, falls, or crushing the area against a hard surface. Symptoms include pain, bruising, swelling, and decreased mobility. Treatment involves rest, ice, compression, and elevation to reduce swelling. As bleeding and swelling subside, heat treatments can be used, and massage and stretching can aid recovery.Ulcer by prashant patil, has 27 slides with 26956 views.



Ulcerprashant patil
27 slides•27K views
This document provides an overview of ulcers, including their classification, clinical features, investigations, and management principles. Ulcers are classified based on duration (acute vs chronic), etiology (infectious, physical/chemical agents, circulation impairment), and location (Wagner's classification for foot ulcers). Clinical features include characteristics of the site, size, shape, edges, floor, base, discharge, pain levels, and surrounding lymph nodes. Investigations may include hematological and biochemical tests, imaging, and biopsies. Management principles focus on determining the underlying cause, correcting comorbidities, adequate drainage and debridement, treating any infection, and using appropriate dressings to promote healing.Healing and repair by dinesh, has 40 slides with 38417 views.



Healing and repair dinesh Healing occurs through regeneration or scar formation depending on the cell and injury type. Wound healing follows two main pathways: primary intention for clean surgical wounds where edges are approximated, or secondary intention for wounds with separated edges and more tissue death. The process involves inflammation, granulation tissue formation, re-epithelialization, wound contraction and ECM deposition. Several local and systemic factors can delay healing including infection, poor blood supply, drugs, and nutritional deficiencies.
Necrotising fasciitis.by.Yapa Wijeratne



Necrotising fasciitis.by.Yapa WijeratneYapa Necrotising fasciitis is a surgical emergency having mortality 30–50% even with the best care.
Therefore immediate diagnosis & management is a must.
Diabetic foot + gangrene



Diabetic foot + gangrenegroup7usmkk Diabetic foot complications are a major source of morbidity and health care costs. They result from a complex interplay of ischemia, ulceration, infection, and Charcot's joint due to diabetes-related changes. Hyperglycemia leads to nonenzymatic glycosylation of proteins and tissues, formation of advanced glycosylation end products, and accelerated atherosclerosis. This causes peripheral vascular disease, neuropathy, and foot deformities which impair sensation and blood flow, making the feet susceptible to infection, ulceration, and gangrene. Charcot's joint is a destructive foot arthropathy caused by loss of sensation from diabetic neuropathy.
OSCE dermatological history and examination



OSCE dermatological history and examinationMonther AL Gahafi The document provides guidance on conducting a dermatological history and examination. It outlines taking a thorough history including details of the presenting complaint, past medical history, medications, and social history. The examination section describes inspecting the skin lesions carefully, noting their characteristics, distribution, and secondary changes. The examiner is advised to obtain consent, ensure comfort, and summarize findings and differential diagnosis.
Non specific ulcers



Non specific ulcersDr KAMBLE This document provides an overview of various types of non-specific ulcers, including their causes, characteristics, and treatments. It discusses ulcers caused by trauma, arterial issues, venous issues, pressure, infection, tropical conditions, frostbite, hypertension, diabetes, mycobacteria, cancer, and more. For most ulcer types, it outlines key features like location, appearance, complications, investigations needed, and management approaches involving wound care, antibiotics, surgery, or other therapies.
Neuropathy



NeuropathyComprehensive Prosthetics & Orthotics Peripheral neuropathy is damage or disease affecting nerves that may impair sensation, movement, organ function, or other health aspects depending on the affected nerve. Common causes include diseases like diabetes or leprosy, vitamin deficiencies, medications, injuries, alcohol consumption, immune system diseases, infections, or inheritance. Symptoms include numbness, tingling, muscle weakness, reduced sense of position, pins and needles, itching. Treatments include amitriptyline, antiepileptics like gabapentin, cannabinoids, pregabalin, and electric nerve stimulation. Medical cannabis has uses for conditions like diabetes, cancer, dementia and epilepsy but more research is needed on adverse effects and potential conflicts of interest in research funding.
Healing Shoe Care and Use Guide



Healing Shoe Care and Use GuideComprehensive Prosthetics & Orthotics This document contains information on care and use for a healing shoe (for patients with diabetic ulcers on feet or open wounds on their feet).
More Related Content
What's hot (20)
History taking - For Surgical patients



History taking - For Surgical patientsUthamalingam Murali This PPT is based on taking history from surgical patients for UG - Students. ( Based on History taking methods adopted by S.Das )
Gangrene



GangreneLazoi Lifecare Private Limited Gangrene occurs when tissues die due to lack of blood flow and oxygen. There are three main types: dry gangrene caused by lack of oxygen, wet gangrene caused by bacterial infection which is more dangerous, and gas gangrene caused by Clostridia bacteria. Symptoms include pain, swelling, discoloration and odor. Treatments depend on the type but may include antibiotics, surgery to improve blood flow, hyperbaric oxygen therapy, debriding dead tissue, and amputation of severely affected body parts.
Robbins Basic Pathology - Tissue Repair



Robbins Basic Pathology - Tissue RepairKing Dietitian Tissue repair involves the restoration of tissue architecture and function through regeneration of injured tissue or replacement by connective tissue scarring. It is a complex process that involves cell proliferation, interaction between cells and the extracellular matrix, angiogenesis, fibroblast migration and proliferation, and deposition of new extracellular matrix. Over time, the granulation tissue matures and remodels through synthesis and degradation of extracellular matrix components.
Ulcer examination



Ulcer examinationBhanwar Sharma This document discusses the classification, examination, and characteristics of ulcers. Ulcers can be classified clinically or pathologically, and can be nonspecific, specific, or malignant. During examination of an ulcer, aspects such as size, shape, edge, floor, discharge, and surrounding area should be evaluated. Characteristics such as induration, tenderness, and relations to deeper structures can help determine if an ulcer is healing, spreading, infected, or malignant.
Wound healing



Wound healingdrmcbansal The document discusses wound healing and classification. It describes the phases of wound healing as inflammatory, proliferative, and remodeling. The inflammatory phase begins immediately after wounding and lasts 2-3 days, involving vasoactive amines, growth factors, and inflammatory cells. The proliferative phase lasts from days 3 to 3 weeks, involving fibroblast activity, collagen production, angiogenesis, and re-epithelialization. The remodeling phase begins during proliferation and lasts up to 2 years, involving collagen remodeling and maturation. Healing is classified as primary intention for clean wounds or secondary intention for infected wounds. Factors like age, obesity, smoking, and malnutrition can affect wound healing.
seminar on Leg swelling & its causes



seminar on Leg swelling & its causesBiswajit Deka This document summarizes leg swelling (edema) and its various causes. It begins by defining edema and mechanisms that can cause it like increased capillary permeability or pressure. It then categorizes causes of edema as either central (bilateral) or local (unilateral). Specific conditions that can lead to edema like cardiac failure, nephrotic syndrome, filariasis, and deep vein thrombosis are described. The document provides details on clinical presentations and risk factors for different types of edema.
Ulcers Basics



Ulcers BasicsDr. Valluri Mukesh A Basic Session on Ulcers, Classifications, Types, Clinical Examination, Investigations, Treatment & Management
Edema



EdemaKanav Bhanot CONTENTS:
GENERAL
NORMAL FLUID CIRCULATION
EDEMA- INTRODUCTION
CAUSES
CLASSIFICATION
MAJOR TYPES
NOTE- Fonts may appear weird because the original fonts are different from the ones visible here.
Vascular Ulcers Ppt -



Vascular Ulcers Ppt -Chukwuma-Ikem Okoye This document provides an overview of vascular ulcers, including their classification, etiology, pathophysiology, and management. The main types of vascular ulcers are venous ulcers, arterial ulcers, and mixed arteriovenous ulcers. Venous ulcers are the most common and are usually located over the medial gaiter region of the leg. Arterial ulcers are suggested by diminished or absent peripheral pulses and often have a gray or black wound base. Treatment involves conservative measures like compression therapy for venous ulcers and endovascular procedures or bypass grafts for arterial insufficiency. Proper wound care, infection control, and patient education are important for management.
Gas gangrene



Gas gangreneDrPoojaPandey4 Gas gangrene is a life-threatening infection of subcutaneous tissue and muscle caused by clostridial bacteria such as Clostridium perfringens, which release toxins like alpha toxin that cause tissue necrosis. It is associated with wounds, surgery, or trauma and has a rapid onset of symptoms like pain, swelling, crepitus, and gangrenous changes in the skin. Aggressive surgical debridement and antibiotics such as penicillin are needed for treatment to prevent complications like sepsis, shock, and potential limb loss.
Necrotizing fasciitis



Necrotizing fasciitisimagesrl 1) The document summarizes a presentation on a skin-sparing approach to treating necrotizing fasciitis in children.
2) Key aspects of the approach include early and wide debridement of non-viable tissues while preserving viable skin, with a median skin to fascia excision ratio of 0.1.
3) Using this approach in 13 patients, there was no mortality and low morbidity, with no patients requiring skin grafting and a median time to closure of 5 days.
Wound and wound healing



Wound and wound healingJithin Mampatta This document provides a summary of wounds and wound healing. It begins with definitions of wounds and various classification systems for wounds based on factors like cleanliness, thickness, involvement of structures, time elapsed, and surgical context. It then discusses the stages and phases of wound healing, including inflammation, proliferation, remodeling and epithelialization. Various factors that can affect wound healing are outlined. Finally, it covers wound management principles and common problems like infection, dehiscence, hypertrophic scarring and keloids.
Haemorrhage



HaemorrhageDr. MD. Majedul Islam 1. Hemorrhage is defined as the escape of blood from blood vessels. It can be classified based on the type of vessel (arterial, venous, capillary), timing (primary, reactionary, secondary), visibility (revealed, concealed), duration (acute, chronic), and type of intervention (surgical, non-surgical).
2. Clinical features depend on the amount and speed of blood loss, and can include increasing pallor, pulse, restlessness, signs of shock like cold skin and reduced urine output. Acute blood loss is monitored through pulse, blood pressure, and urine output.
3. Control techniques include direct pressure, elevation, tourniquets, cauterization
Contusions & abrasions



Contusions & abrasionssshssomsen Contusions occur when tissue is injured from blunt force trauma, causing blood vessels to rupture and blood to flow into surrounding tissues. Common causes include contact sports, falls, or crushing the area against a hard surface. Symptoms include pain, bruising, swelling, and decreased mobility. Treatment involves rest, ice, compression, and elevation to reduce swelling. As bleeding and swelling subside, heat treatments can be used, and massage and stretching can aid recovery.
Ulcer



Ulcerprashant patil This document provides an overview of ulcers, including their classification, clinical features, investigations, and management principles. Ulcers are classified based on duration (acute vs chronic), etiology (infectious, physical/chemical agents, circulation impairment), and location (Wagner's classification for foot ulcers). Clinical features include characteristics of the site, size, shape, edges, floor, base, discharge, pain levels, and surrounding lymph nodes. Investigations may include hematological and biochemical tests, imaging, and biopsies. Management principles focus on determining the underlying cause, correcting comorbidities, adequate drainage and debridement, treating any infection, and using appropriate dressings to promote healing.
Healing and repair 



Healing and repair dinesh Healing occurs through regeneration or scar formation depending on the cell and injury type. Wound healing follows two main pathways: primary intention for clean surgical wounds where edges are approximated, or secondary intention for wounds with separated edges and more tissue death. The process involves inflammation, granulation tissue formation, re-epithelialization, wound contraction and ECM deposition. Several local and systemic factors can delay healing including infection, poor blood supply, drugs, and nutritional deficiencies.
Necrotising fasciitis.by.Yapa Wijeratne



Necrotising fasciitis.by.Yapa WijeratneYapa Necrotising fasciitis is a surgical emergency having mortality 30–50% even with the best care.
Therefore immediate diagnosis & management is a must.
Diabetic foot + gangrene



Diabetic foot + gangrenegroup7usmkk Diabetic foot complications are a major source of morbidity and health care costs. They result from a complex interplay of ischemia, ulceration, infection, and Charcot's joint due to diabetes-related changes. Hyperglycemia leads to nonenzymatic glycosylation of proteins and tissues, formation of advanced glycosylation end products, and accelerated atherosclerosis. This causes peripheral vascular disease, neuropathy, and foot deformities which impair sensation and blood flow, making the feet susceptible to infection, ulceration, and gangrene. Charcot's joint is a destructive foot arthropathy caused by loss of sensation from diabetic neuropathy.
OSCE dermatological history and examination



OSCE dermatological history and examinationMonther AL Gahafi The document provides guidance on conducting a dermatological history and examination. It outlines taking a thorough history including details of the presenting complaint, past medical history, medications, and social history. The examination section describes inspecting the skin lesions carefully, noting their characteristics, distribution, and secondary changes. The examiner is advised to obtain consent, ensure comfort, and summarize findings and differential diagnosis.
Non specific ulcers



Non specific ulcersDr KAMBLE This document provides an overview of various types of non-specific ulcers, including their causes, characteristics, and treatments. It discusses ulcers caused by trauma, arterial issues, venous issues, pressure, infection, tropical conditions, frostbite, hypertension, diabetes, mycobacteria, cancer, and more. For most ulcer types, it outlines key features like location, appearance, complications, investigations needed, and management approaches involving wound care, antibiotics, surgery, or other therapies.
More from Comprehensive Prosthetics & Orthotics (20)
Neuropathy



NeuropathyComprehensive Prosthetics & Orthotics Peripheral neuropathy is damage or disease affecting nerves that may impair sensation, movement, organ function, or other health aspects depending on the affected nerve. Common causes include diseases like diabetes or leprosy, vitamin deficiencies, medications, injuries, alcohol consumption, immune system diseases, infections, or inheritance. Symptoms include numbness, tingling, muscle weakness, reduced sense of position, pins and needles, itching. Treatments include amitriptyline, antiepileptics like gabapentin, cannabinoids, pregabalin, and electric nerve stimulation. Medical cannabis has uses for conditions like diabetes, cancer, dementia and epilepsy but more research is needed on adverse effects and potential conflicts of interest in research funding.
Healing Shoe Care and Use Guide



Healing Shoe Care and Use GuideComprehensive Prosthetics & Orthotics This document contains information on care and use for a healing shoe (for patients with diabetic ulcers on feet or open wounds on their feet).
Diabetic Foot Care



Diabetic Foot CareComprehensive Prosthetics & Orthotics This document contains information on diabetic foot-care. It also has information on the care and use of diabetic shoes.
Care and Use Guide for Cervical Orthosis



Care and Use Guide for Cervical OrthosisComprehensive Prosthetics & Orthotics This document provides care instructions for a cervical orthosis (neck brace). It describes how to apply the brace, cleaning instructions, and tips for use. The brace is to be worn according to the physician's recommendations and any issues should be reported to the orthotist.
Spasticity



SpasticityComprehensive Prosthetics & Orthotics This is a document that contains information on spasticity, diagnosis, symptoms and treatment for spasticity.
Kyphosis



KyphosisComprehensive Prosthetics & Orthotics It is a document that contains information on types, symptoms and treatment for Kyphosis.
Scoliosis



ScoliosisComprehensive Prosthetics & Orthotics This is a document that contains information on scoliosis - symptoms, diagnosis, prognosis, types and treatment.
Spinal disc Herniation



Spinal disc HerniationComprehensive Prosthetics & Orthotics It is a document that contains information on causes, symptoms and treatment for Spinal Disc Herniation.
Club Foot



Club FootComprehensive Prosthetics & Orthotics This is a document that contains information on Club Foot.
Osteoarthritis



OsteoarthritisComprehensive Prosthetics & Orthotics It is a document on osteoarthritis. It contains information on causes, symptoms and treatment for osteoarthritis.
Spina Bifida



Spina BifidaComprehensive Prosthetics & Orthotics This is a document on Spina Bifida. It contains information on symptoms, types and treatment for Spina Bifida.
Muscular Dystrophy



Muscular DystrophyComprehensive Prosthetics & Orthotics It is a document on muscular dystrophy. It contains information on types, symptoms, causes and treatment of muscular dystrophy.
Cervical Spondylosis 



Cervical Spondylosis Comprehensive Prosthetics & Orthotics This document will provide you with information about symptoms, causes, diagnosis and treatment of Cervical Spondylosis.
Cerebral Palsy



Cerebral PalsyComprehensive Prosthetics & Orthotics It is a document that contains information on cerebral palsy.
Tips



TipsComprehensive Prosthetics & Orthotics 1. The document provides 10 tips for diabetic foot care, including checking your feet daily for issues, keeping your skin and nails well-maintained, wearing appropriate shoes and socks, and maintaining blood flow to your feet.
2. Key recommendations include monitoring blood glucose levels, being active after consulting your healthcare team, and asking your doctor about Medicare coverage for special shoes.
3. Taking good care of your feet daily is emphasized as important for diabetics, such as by setting aside time each day for a foot check.
Achilles Tendinitis



Achilles TendinitisComprehensive Prosthetics & Orthotics Gives you the what, why and what to do of Achilles Tendinitis
Mastectomy- Whats and Whys



Mastectomy- Whats and WhysComprehensive Prosthetics & Orthotics The slide gives information about mastectomy, types of mastectomy and breast prostheses.
Below Knee Amputation An Overview of Prosthetic Care 



Below Knee Amputation An Overview of Prosthetic Care Comprehensive Prosthetics & Orthotics A document from CPO discusses restoring mobility and quality of life for those with below knee amputations. CPO provides prosthetics to help amputees regain mobility and independence through their prosthetic devices and rehabilitation services. The website and date on the document suggest it contains information for marketing CPO's below knee prosthetics.
Above Knee Amputation An Overview Of Prosthetic Care 



Above Knee Amputation An Overview Of Prosthetic Care Comprehensive Prosthetics & Orthotics An above-knee amputation can impact mobility and quality of life. CPO (the company) aims to restore both through their prosthetic devices and rehabilitation support. Their website www.cpousa.com provides information for those who have undergone an above-knee amputation.
Recently uploaded (20)
FAO's Support Rabies Control in Bali_Jul22.pptx



FAO's Support Rabies Control in Bali_Jul22.pptxWahid Husein What is FAO doing to support rabies control programmes in Bali, Indonesia, using One Health approach with mass dog vaccination and integrated bite case management as main strategies
Research Problems - Nursing Research....



Research Problems - Nursing Research....Dr. Binu Babu Nursing Lectures Incredibly Easy Research Problems - Nursing Research
Eye assessment in polytrauma for undergraduates.pptx



Eye assessment in polytrauma for undergraduates.pptxKafrELShiekh University Eye assessment in polytrauma for undergraduates.
Public health 101 x health disinformation.pptx



Public health 101 x health disinformation.pptxTina Purnat Public health approaches to health disinformation
Digestive Powerhouses: Liver, Gallbladder, and Pancreas for Nursing Students



Digestive Powerhouses: Liver, Gallbladder, and Pancreas for Nursing StudentsViresh Mahajani This educational PowerPoint presentation is designed to equip GNM students with a solid understanding of the liver, pancreas, and gallbladder. It explores the anatomical structures, physiological processes, and clinical significance of these vital organs. Key topics include:
Liver functions: detoxification, metabolism, and bile synthesis.
Gallbladder: bile storage and release.
Pancreas: exocrine and endocrine functions, including digestive enzyme and hormone production. This presentation is ideal for GNM students seeking a clear and concise review of these important digestive system components."
Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...



Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...PVI, PeerView Institute for Medical Education Co-Chairs, Robert M. Hughes, DO, and Christina Y. Weng, MD, MBA, prepared useful Practice Aids pertaining to retinal vein occlusion for this CME activity titled “Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Specialty Care.” For the full presentation, downloadable Practice Aids, and complete CME information, and to apply for credit, please visit us at https://bit.ly/3NyN81S. CME credit will be available until March 3, 2026.
Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...



Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...PVI, PeerView Institute for Medical Education Co-Chairs and Presenters, Gerald Appel, MD, and Dana V. Rizk, MD, discuss kidney disease in this CME activity titled “Advancements in IgA Nephropathy: Discovering the Potential of Complement Pathway Therapies.” For the full presentation, downloadable Practice Aids, and complete CME information, and to apply for credit, please visit us at https://bit.ly/48UHvVM. CME credit will be available until February 25, 2026.
Characteristics and Criteria of Good Research.pptx



Characteristics and Criteria of Good Research.pptxDr. Binu Babu Nursing Lectures Incredibly Easy Characteristics and Criteria of Good Research
legal Rights of individual, children and women.pptx



legal Rights of individual, children and women.pptxRishika Rawat A legal right is a claim or entitlement that is recognized and protected by the law. It can also refer to the power or privilege that the law grants to a person. Human rights include the right to life and liberty, freedom from slavery and torture, freedom of opinion and expression, the right to work and education
Sudurpaschim logsewa aayog Medical Officer 8th Level Curriculum



Sudurpaschim logsewa aayog Medical Officer 8th Level CurriculumDr Ovels Sudurpaschim province psc ( lok sewa aayog) medical officer 8th level syllabus
Regulation of tubular reabsorption _AntiCopy.pdf



Regulation of tubular reabsorption _AntiCopy.pdfMedicoseAcademics Title: Regulation of Tubular Reabsorption – A Comprehensive Overview
Description:
This lecture provides a detailed and structured explanation of the mechanisms regulating tubular reabsorption in the kidneys. It explores how different physiological and hormonal factors influence glomerular filtration and reabsorption rates, ensuring fluid and electrolyte balance in the body.
🔍 Who Should Read This?
This presentation is designed for:
✔️ Medical Students (MBBS, BDS, Nursing, Allied Health Sciences) preparing for physiology exams.
✔️ Medical Educators & Professors looking for structured teaching material.
✔️ Healthcare Professionals (doctors, nephrologists, and physiologists) seeking a refresher on renal physiology.
✔️ Postgraduate Students & Researchers in the field of medical sciences and physiology.
📌 What You’ll Learn:
✅ Local Regulation of Tubular Reabsorption
✔️ Glomerulo-Tubular Balance – its mechanism and clinical significance
✔️ Net reabsorptive forces affecting peritubular capillaries
✔️ Role of peritubular hydrostatic and colloid osmotic pressures
✅ Hormonal Regulation of Tubular Reabsorption
✔️ Effects of Aldosterone, Angiotensin II, ADH, and Natriuretic Peptides
✔️ Clinical conditions like Addison’s disease & Conn Syndrome
✔️ Mechanisms of pressure natriuresis and diuresis
✅ Nervous System Regulation
✔️ Sympathetic Nervous System activation and its effects on sodium reabsorption
🩺 Clinical Correlations & Case Discussions
✔️ How renal regulation is altered in hypertension, hypotension, and proteinuria
✔️ Comparison of Glomerulo-Tubular Balance vs. Tubulo-Glomerular Feedback
This presentation provides detailed diagrams, flowcharts, and calculations to enhance understanding and retention. Whether you are studying, teaching, or practicing medicine, this lecture will serve as a valuable resource for mastering renal physiology.
📢 Keywords for Easy Search:
#Physiology #RenalPhysiology #TubularReabsorption #GlomeruloTubularBalance #HormonalRegulation #MedicalEducation #Nephrology
ISO 14155 Clinical investigation of medical devices for human subjects- Good ...



ISO 14155 Clinical investigation of medical devices for human subjects- Good ...ketakeephadnis Clinical investigation of medical devices for human subjects- Good clinical practices
plant fibres and surgical dressing. method of preparation



plant fibres and surgical dressing. method of preparationchandaniprasad Surgical dressing- The word surgical dressing is used to include all the materials
either used alone or in combination to cover the wound.
Addressing Unmet Needs for Better Outcomes in DLBCL: Leveraging Prognostic As...



Addressing Unmet Needs for Better Outcomes in DLBCL: Leveraging Prognostic As...PVI, PeerView Institute for Medical Education Chair, Grzegorz (Greg) S. Nowakowski, MD, FASCO, discusses diffuse large B-cell lymphoma in this CME activity titled “Addressing Unmet Needs for Better Outcomes in DLBCL: Leveraging Prognostic Assessment and Off-the-Shelf Immunotherapy Strategies.” For the full presentation, downloadable Practice Aid, and complete CME information, and to apply for credit, please visit us at https://bit.ly/49JdxV4. CME credit will be available until February 27, 2026.
Evidence - Based Practice - Nursing Research



Evidence - Based Practice - Nursing ResearchDr. Binu Babu Nursing Lectures Incredibly Easy Evidence-Based Practice - Nursing Research
Research Hyopthesis and Research Assumption



Research Hyopthesis and Research AssumptionDr. Binu Babu Nursing Lectures Incredibly Easy Research Hyopthesis and Assumption
E Book Daniya Sanal.pdf#healthy books.com



E Book Daniya Sanal.pdf#healthy books.comDaniyaSanal good health for good life good heart for safe and secure life..the good quality of life will makes good and #haelthy vibes...
Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...



Retinal Disease in Emergency Medicine: Timely Recognition and Referral for Sp...PVI, PeerView Institute for Medical Education
Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...



Advancements in IgA Nephropathy: Discovering the Potential of Complement Path...PVI, PeerView Institute for Medical Education
Addressing Unmet Needs for Better Outcomes in DLBCL: Leveraging Prognostic As...



Addressing Unmet Needs for Better Outcomes in DLBCL: Leveraging Prognostic As...PVI, PeerView Institute for Medical Education




