TRACHOMA- DIAGNOSIS AND MANAGEMENT
- 1. Dr. Arvind K. Morya, MBBS, MS(Gold Medalist),MNAMS Glaucoma,Phaco(MICS), Cornea and refractive, Strabismus Paediatric Ophthalmology and Medical Retina Services Department of Ophthalmology, AIIMS Jodhpur
- 2. Introduction Trachoma comes from Greek word trachoma (τράχωμα) meaning “roughness”. Trachoma was well known as an infectious ocular disease and documented as “ophthalmia”. The history of this disease began as early as 8000 B.C.
- 3. Trachoma Trachoma, one of the oldest infectious eye diseases, is the world’s leading cause of preventable blindness. Repeated infections of the conjunctivae with Chlamydia trachomatis can lead to trichiasis, corneal opacity and blindness. An estimated 325 million people live in at-risk areas. Trachoma blinds one person every 15 minutes.
- 4. EPIDEMIOLOGY Endemic in 42 countries - causing visual impairment in 1.9 million people. Leading cause of infectious Blindness globally Infective Trachoma (TF/TI) – Follicles in upper tarsal conjunctiva – upto10 years of age Trachomatous Trichiasis(TT) – Scarring leading to Trichiasis – After 15 years of age Spread- direct contact/ through flies
- 5. CAUSITIVE ORGANISM: •Chlamydia trachomatis bacteria •11 serotypes recognized Etiology
- 6. SOURCE OF INFECTION: •Conjunctival discharge •Superimposed bacterial infection speed up the process
- 7. MODES OF INFECTION: •Direct spread by air-borne or water-borne modes •Vector transmission by flies •Material transfer through contaminated fingers, clothes, bedding etc
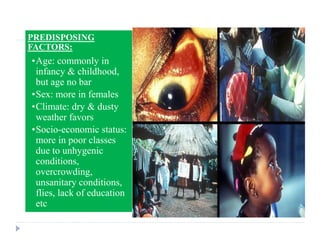
- 8. PREDISPOSING FACTORS: •Age: commonly in infancy & childhood, but age no bar •Sex: more in females •Climate: dry & dusty weather favors •Socio-economic status: more in poor classes due to unhygenic conditions, overcrowding, unsanitary conditions, flies, lack of education etc •Environmental: exposure to dust, irritants, smoke,
- 9. CLINICAL PROFILE • Incubation period: 5-21 days, mostly insidious onset • Clinical course: • Pure trachoma is mild & symptomless, often neglected • If superimposed with bacterial infection, presents with typical bacterial conjunctivitis
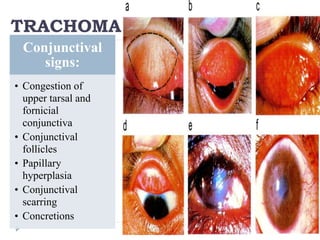
- 10. Conjunctival signs: • Congestion of upper tarsal and fornicial conjunctiva • Conjunctival follicles • Papillary hyperplasia • Conjunctival scarring • Concretions TRACHOMA
- 11. Corneal signs: • Superficial keratitis • Herbert follicles • Pannus • Corneal ulcer • Herbert Pits • Corneal opacity
- 12. • Active disease, predominantly follicles • At least 5 or more follicles in upper palpebral conjunctiva TF (Trachomatous Inflammation – Follicular) • Pronounced inflammatory thickening of upper palpebral conjunctiva obscures > half of normal deep tarsal vessels TI (Trachomatous Inflammation – Intense) • Presence of scarring in tarsal cunjunctiva • Seen as white bands or sheets of fibrosis TS (Trachomatous Scarring) • When at least 1 eyelash rubs the ocular surface • Evidence of recently removed trichiatic eyelashes TT (Trachomatous Trichiasis) • Easily visible corneal opacity present in pupillary area • Causes significant visual impairment CO - Corneal Opacity WHO Classification (FISTO)
- 13. TS
- 14. Active Trachoma Infection among Participants aged 1-9 years
- 15. Looking for TF
- 16. Looking for Sequelae ( >=15 years)
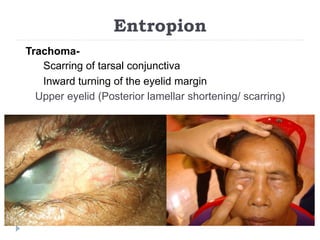
- 17. Entropion Trachoma- Scarring of tarsal conjunctiva Inward turning of the eyelid margin Upper eyelid (Posterior lamellar shortening/ scarring)
- 18. Grade for upper eyelid Entropion Minimal Apparent migration of meibomian glands Conjunctivalization of lid margin Lash-globe contact on up gaze Moderate Lash-globe contact in primary position Thickening of tarsal plate Lid retraction Severe Lid retraction causing incomplete closure Gross lid distortion Metaplastic lashes Presence of keratin plaques
- 19. Microbiological Investigations Conjunctival swabbing- children with active infection Direct Immuno-fluroscence assay analysis by the ocular microbiology dept.
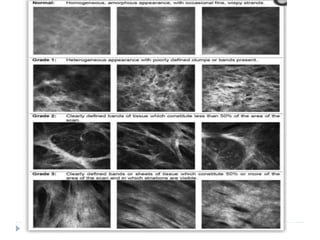
- 20. Investigations Accurate estimation of infection 1. DNA based NAAT 2. rRNA based NAAT In-vivo confocal microscopy : Hu et al IVCM GRADING FOR INFLAMMATORY AND SCARRING CHANGES
- 21. Nucleic acid amplification tests Nucleic acid amplification test (NAAT) that targets the cryptic DNA plasmid of chlamydia (Amplicor; Roche Diagnostics, Indianapolis, IN). A second-generation rRNA-based NAAT with an additional target capture step (Aptima Combo 2; Gen-Probe, San Diego, CA) has been shown to be among the most sensitive and specific of the NAATs for the detection of chlamydia. Because of its superior sensitivity, the RNA test is a logical gold standard test against which to compare other tests for their ability to predict ocular chlamydia.
- 23. A.INFLAMMATORY INFILTRATE : SEEN AS MULTIPLE BRIGHT WHITE NUCLEI. THE MEAN INFLAMMATORY CELL DENSITY OF 3 RANDOMLY SELECTED VOLUME SCANS IS CALCULATED B.B. DENDRITIFORM CELLS ( DCs) : present or absent , present when >/= 1 dcs per volume scaned C.C . Tissue oedema : present or absent D.D papillae : present or absent .
- 25. Trachoma Recurrent infection in childhood (1-9 years) Trichiasis in adulthood (>15 years) Corneal opacity/ blindness (painful) A,F,E S- surgery
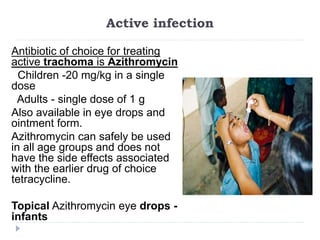
- 26. Active infection Antibiotic of choice for treating active trachoma is Azithromycin Children -20 mg/kg in a single dose Adults - single dose of 1 g Also available in eye drops and ointment form. Azithromycin can safely be used in all age groups and does not have the side effects associated with the earlier drug of choice tetracycline. Topical Azithromycin eye drops - infants
- 27. TT- Trachoma Trichiasis Trichiasis- misdirected eyelashes touching the globe (other signs of trachoma present) May be associated with Cicatricial entropion- inward turning of the eyelid margin
- 29. How to treat? Minor Trichiasis: 5 or less trichiatic lashes, not threatening cornea Epilation- Mechanical epilation is usually the first-line treatment, especially for a few isolated lashes. Recurrence is common.
- 30. Electrolysis Involves inserting a probe into each individual follicle under slit lamp or operating microscope magnification. After local anesthetic is infiltrated into the eyelid, the probe is inserted along a hair shaft . Electrical charge is applied until bubbling is seen at the root of the hair shaft. If the hair shaft and bulb pull freely, the treatment is successful.
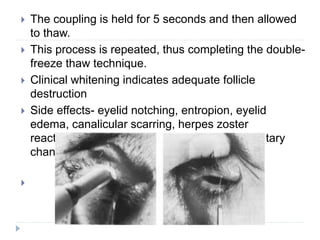
- 31. Cryotherapy After local anesthetic is injected, the probe is applied to the treatment area using a coupling gel . The cold treatment is then initiated, with the thermocouple set to -20 to -30 degrees Celsius. A frost-ball will propagate, and slight traction on the probe will cause eyelid distraction, thus confirming thermocoupling.
- 32. The coupling is held for 5 seconds and then allowed to thaw. This process is repeated, thus completing the double- freeze thaw technique. Clinical whitening indicates adequate follicle destruction Side effects- eyelid notching, entropion, eyelid edema, canalicular scarring, herpes zoster reactivation, symblepharon and eyelid pigmentary changes.
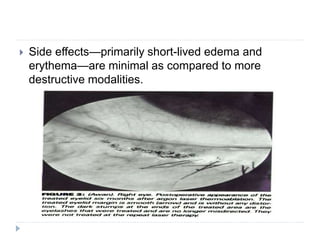
- 33. Argon Laser treatment The argon beam is generally titrated based on the pigmentation of the cilia, with suggested laser settings varying between 300 mW/0.5 s/50 µm and 1,200 mW/0.2 to 0.5 s/50 to 100 µm. The beam is directed 2 to 3 mm below the lash base, coaxial to the lash. Repetitive burns are required for follicle destruction.
- 34. Side effects—primarily short-lived edema and erythema—are minimal as compared to more destructive modalities.
- 35. Surgical techniques Include eyelid wedge resection, horizontal blepharotomy, tarsal fracturing and eyelid splitting.
- 36. How to treat? More than 5 trichiatic lashes/ threatening the cornea/ associated entropion Corrective eyelid margin/ entropion surgery based on degree of entropion
- 37. WHO Recommendation WHO recommends entropion surgery in any trichiasis ‘to avoid loss to follow up in patients with minor trichiasis’
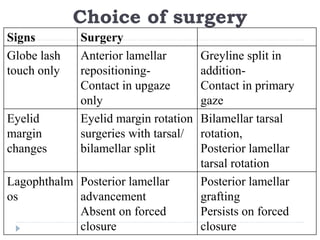
- 38. Degree of entropion? Globe lash contact- in upgaze only / primary gaze Eyelid margin changes- keratinization/ metaplastic lashes Lagophthalmos- inability to close the eyelid on gentle or forced closure Tarsal thickening
- 39. Lid margin keratinisation Metaplastic lashes
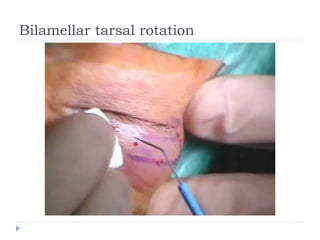
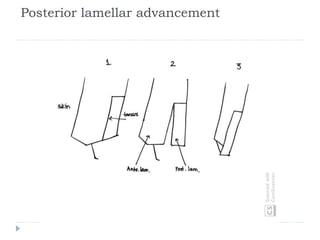
- 40. Choice of surgery Signs Surgery Globe lash touch only Anterior lamellar repositioning- Contact in upgaze only Greyline split in addition- Contact in primary gaze Eyelid margin changes Eyelid margin rotation surgeries with tarsal/ bilamellar split Bilamellar tarsal rotation, Posterior lamellar tarsal rotation Lagophthalm os Posterior lamellar advancement Absent on forced closure Posterior lamellar grafting Persists on forced closure
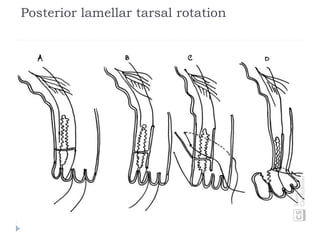
- 45. Posterior lamellar tarsal rotation
- 46. Tarsal fracture with terminal rotation
- 49. Strategies for prevention of trachoma Global Elimination of Trachoma – GET 2020 program WHO Goal - Eliminate trachoma by 2020 India is signatory to GET2020
- 50. History In 1997, WHO launched the WHO Alliance for the Global Elimination of Trachoma by the year 2020 (GET2020). GET strengthens national capacity by Epidemiological Assessment Monitoring surveillance Project Evaluation Resource mobilization
- 52. Target Elimination of trachoma as a public health problem: Persons > 15 years of age suffering from TT “unknown to the health system” (< 0.2% in each district, approximately 1 case per 1000 total population) Children 1-9 years of age suffering from TF/TI < 5% in each district, sustained for at least two years in the absence of ongoing antibiotic mass treatment, in each formerly endemic district Presence of a health system able to identify and manage new trachomatous trichiasis cases Through defined strategies With appropriate financial resources to implement those strategies
- 53. State Prevalence rate of active infection (1959-63 survey) Prevalence rate of active infection (86-89 Survey) Burden of active infection TRA in 2006 Haryana 79.1 (Punjab) 3.8 4.0 Rajasthan 74.1 4.2 7.8 Gujarat 56.0 4.8 0.9 Punjab 79.1 6.9 5.5 Western UP / Uttaranchal 68.1 9.5 9.8 Trachoma burden in India Prevalence studies needed to assess the true burden in the community and to ascertain whether trachoma has ceased to be a public health problem
- 54. Prevalence of TT in India is 3.5 per 1000 in 15+ population (Age & Sex Standardized) Prevalence of Trachomatous Trichiasis in India (2014-17) WHO Criteria For Elimination: Less than 2/1000 in 15+ population
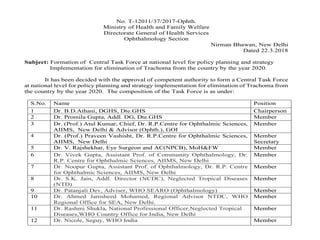
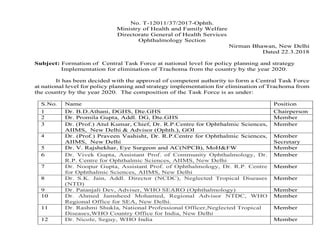
- 55. Trachoma Elimination in India: Recommendations Central Task force & Monitoring committee of trachoma elimination programme: Central Task Force at national level for policy planning, strategy for implementation for elimination of Trachoma from the country by the year 2020 Monitoring Committee for monitoring and reporting of Trachoma cases in states for elimination of Trachoma from the country by the year 2020.
- 56. No. T-12011/37/2017-Ophth. Ministry of Health and Family Welfare Directorate General of Health Services Ophthalmology Section Nirman Bhawan, New Delhi Dated 22.3.2018 Subject: Formation of Central Task Force at national level for policy planning and strategy Implementation for elimination of Trachoma from the country by the year 2020. It has been decided with the approval of competent authority to form a Central Task Force at national level for policy planning and strategy implementation for elimination of Trachoma from the country by the year 2020. The composition of the Task Force is as under: S.No. Name Position 1 Dr. B.D.Athani, DGHS, Dte.GHS Chairperson 2 Dr. Promila Gupta, Addl. DG, Dte.GHS Member 3 Dr. (Prof.) Atul Kumar, Chief, Dr. R.P.Centre for Ophthalmic Sciences, AIIMS, New Delhi & Advisor (Ophth.), GOI Member 4 Dr. (Prof.) Praveen Vashisht, Dr. R.P.Centre for Ophthalmic Sciences, AIIMS, New Delhi Member Secretary 5 Dr. V. Rajshekhar, Eye Surgeon and AC(NPCB), MoH&FW Member 6 Dr. Vivek Gupta, Assistant Prof. of Community Ophthalmology, Dr. R.P. Centre for Ophthalmic Sciences, AIIMS, New Delhi Member 7 Dr. Noopur Gupta, Assistant Prof. of Ophthalmology, Dr. R.P. Centre for Ophthalmic Sciences, AIIMS, New Delhi Member 8 Dr. S.K. Jain, Addl. Director (NCDC), Neglected Tropical Diseases (NTD) Member 9 Dr. Patanjali Dev, Adviser, WHO SEARO (Ophthalmology) Member 10 Dr. Ahmed Jamsheed Mohamed, Regional Advisor NTDC, WHO Regional Office for SEA, New Delhi. Member 11 Dr. Rashmi Shukla, National Professional Officer,Neglected Tropical Diseases,WHO Country Office for India, New Delhi Member 12 Dr. Nicole, Seguy, WHO India Member
- 57. No. T-12011/37/2017-Ophth. Ministry of Health and Family Welfare Directorate General of Health Services Ophthalmology Section Nirman Bhawan, New Delhi Dated 22.3.2018 Subject: Formation of Central Task Force at national level for policy planning and strategy Implementation for elimination of Trachoma from the country by the year 2020. It has been decided with the approval of competent authority to form a Central Task Force at national level for policy planning and strategy implementation for elimination of Trachoma from the country by the year 2020. The composition of the Task Force is as under: S.No. Name Position 1 Dr. B.D.Athani, DGHS, Dte.GHS Chairperson 2 Dr. Promila Gupta, Addl. DG, Dte.GHS Member 3 Dr. (Prof.) Atul Kumar, Chief, Dr. R.P.Centre for Ophthalmic Sciences, AIIMS, New Delhi & Advisor (Ophth.), GOI Member 4 Dr. (Prof.) Praveen Vashisht, Dr. R.P.Centre for Ophthalmic Sciences, AIIMS, New Delhi Member Secretary 5 Dr. V. Rajshekhar, Eye Surgeon and AC(NPCB), MoH&FW Member 6 Dr. Vivek Gupta, Assistant Prof. of Community Ophthalmology, Dr. R.P. Centre for Ophthalmic Sciences, AIIMS, New Delhi Member 7 Dr. Noopur Gupta, Assistant Prof. of Ophthalmology, Dr. R.P. Centre for Ophthalmic Sciences, AIIMS, New Delhi Member 8 Dr. S.K. Jain, Addl. Director (NCDC), Neglected Tropical Diseases (NTD) Member 9 Dr. Patanjali Dev, Adviser, WHO SEARO (Ophthalmology) Member 10 Dr. Ahmed Jamsheed Mohamed, Regional Advisor NTDC, WHO Regional Office for SEA, New Delhi. Member 11 Dr. Rashmi Shukla, National Professional Officer,Neglected Tropical Diseases,WHO Country Office for India, New Delhi Member 12 Dr. Nicole, Seguy, WHO India Member
- 58. Trachoma Elimination in India: Recommendations Implementing SAFE strategy
- 59. Acknowledgements Special thanks to Dr. Rachna Meel, Dr. Noopur Gupta, Dr. Rashmi Singh, Dr. Talvir Sidhu for Anterior lamellar repositioning video and Trabut procedure video. Special thanks to Dr. Hunter Yuen for bilamellar tarsal rotation video. Postgraduate Dr. Sonalika Gogia, Ms. Diksha and Ms. Neha for providing their inputs for making this presentation For any queries, contact us at: [email protected]
Editor's Notes
- Rrna more sensitive than dna based 100% SENSITIVITY AND SPECIFICITY
- INFLAMMATORY INFILTRATE : SEEN AS MULTIPLE BRIGHT WHITE NUCLEI. THE MEAN INFLAMMATORY CELL DENSITY OF 3 RANDOMLY SELECTED VOLUME SCANS IS CALCULATED B. DENDRITIFORM CELLS ( DCs) : present or absent , present when >/= 1 dcs per volume scaned C . Tissue oedema : present or absent D papillae : present or absent .