Tumor pathogenesis
- 2. Growth factors Epidermal growth factor Endothelial growth factor Fibroblast growth factor Platelet-derived growth factor Nerve growth factor Insulin-like growth factors Hepatocyte growth factor Transforming growth factor Interleukins 1-7
- 3. Genes controlling growth The genes which are controlling growth factors synthesis are named proto-oncogenes. If gene controlling growth factor is mutant or hyper activated it is named oncogen. Tumor suppressor gene or anti- oncogenes - their protein product inhibits mitosis
- 4. Mutagenic factors chemical - pro-carcinogens (substances that can convert to carcinogens) and carcinogens. Aflatoxin (from fungus Aspergillus flavus) growing on stored grains, nuts and peanut butter Cooking protein-rich food at high temperatures can lead to the formation of many potent carcinogens. Industrial and tobacco smoke contain benzopyrene, tobacco-specific nitrosamines such as nitrosonornicotine Formaldehyde —embalming and making plastics.
- 5. Mutagenic factors physical (ionizing radiation, ultraviolet rays); biological - viruses. The viral particles can carry a gene that encodes for an overactive oncogene called viral-oncogene and the infected cell is transformed into tumor cell. When tumor development occurs due to above mentioned cause carcinogenesis is named mutational.
- 6. Epigenetic carcinogenesis Transformation of the normal cel to tumor one without mutations by stimulating mitosis may be caused by: certain hormones chronic tissue injury agents that cause inflammation certain viruses.
- 7. The main causes of cancer Smoking, Dietary imbalances (excess fat and calories; inadequate intake of fruits, vegetables, fiber, and calcium) Chronic infections leading to chronic inflammation. Chronic inflammation is a major cause of cancer in the world because it releases powerful oxidants which both stimulate cell division and are mutagens.
- 8. Role of host factors and environment Microsomal enzymes in the liver degrade a large part of a pro-carcinogens to non-carcinogenic products. Naturally occurring compounds, such as indole, flavones, and related compounds that occur in vegetables have a protective action in animals exposed to carcinogenic polycyclic hydrocarbons. Endogenous (and exogenous) sex hormones are important factors apparently in the promotion stage of human carcinomas of breast, endometrium, and prostate.
- 9. Definitions Neoplasia A pathologic process in which a permanent alteration in a cell’s growth controlling mechanism permits its continuous proliferation. Neoplasm A mass of tissue that is actively and progressively growing because of permanent defects its cells’ growth-controlling mechanisms. Benign “Good”; a group of neoplasms that do not threaten life. Malignant “Bad,” a group of neoplasms that invariably kill if not treated. Cancer Any malignant neoplasm. Tumor Any neoplasm.
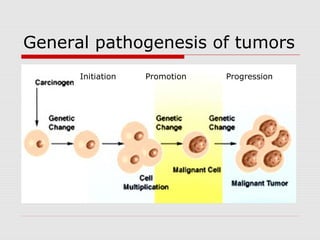
- 10. General pathogenesis of tumor mutation CLONE mutation
- 11. General Pathogenesis of tumors Stage 1. INITIATION. Normal cell under the effect of etiological factors obtains capability to boundless growth and becomes tumor cell. Stage 2. PROMOTION. Transformed cell under the effect of promotors (etiological factors that activate cell division) begins to multiply, giving the beginning to the clone (family) of daughter cells. The primary tumor tissue appears, which consists of similar cells.
- 12. General Pathogenesis of tumors Stage 3. TUMOR PROGRESSION. Regulatory systems of the organism affect the multiplying tumor cells. Tumor cells, in their turn, begin to adapt to the influence of regulatory systems. Thus, tumor cells getting from under the control of immune, endocrine and other regulatory systems of the organism, create new clones of cells. Tumor tissue obtains polymorphism (consists of different cellular clones that differ from each other), increases the speed of its growth, and obtains malignant character.
- 13. General pathogenesis of tumors Initiation Promotion Progression
- 14. Types of neoplasms Benign – less autonomy, usually not invasive, does not metastasize, and generally produces no great harm if treated adequately. Malignant – manifests a greater degree of autonomy, is capable of invasion and metastatic spread, may be resistant to treatment, and may cause death.
- 15. Common characteristics of neoplasms Neoplasia is an irreversible new growth Growth controlling mechanisms are impaired in neoplastic cells. The difference between hyperplasia and neoplasia: Hyperplasia is characterized by cellular proliferation, once its cause is removed, growth stops. Therefore, in hyperplasia growth is “active” but not “progressive.” Neoplastic cells continue to divide even when their causes are removed.
- 16. Common characteristics of neoplasms Absence of cell division limit. Normal cells have division limit Tumor cells are free to divide unlimited amount of times, they are theoretically immortal. The doubling rate of benign cells is relatively slow. The growth rate is much faster in malignant neoplasms.
- 17. Common characteristics of neoplasms Inadequate Differentiation Neoplastic cells do not become as specialized as do normal cells. Malignant neoplasms are composed of less- differentiated cells than benign ones. Benign neoplasms are composed of cells that more closely resemble normal, mature, adult, differentiated cells. Malignant neoplasms are composed of cells that more closely resemble primitive, immature, juvenile, undifferentiated, stem cells.
- 18. Characteristics Unique to Malignant Neoplasms Loss of differentiation is known as “anaplasia.” Anaplasia is seen only in malignant neoplasms Anaplasia may be severe or mild. The more anaplasia that is observed, the more malignant a neoplasm is. There are several types of anaplasia: morphological, biochemical, physical, chemical, functional.
- 19. Characteristics Unique to Malignant Neoplasms Morphological anaplasia. Pleomorphism (pleo- = many; -morphism = shape). Abnormally large nuclei (increased nuclear- cytoplasmic ratio). Abnormally dark nuclei—hyperchromatism. (hyper- = increased; -chromatism = color). Abnormally large and multiplied nucleoli. The quantity and quality of other cell organelles may be changed too. (mitochondrions and ribosomes).
- 20. Characteristics Unique to Malignant Neoplasms Biochemical anaplasia. Carbohydrate atypia –shift to anaerobic glycolysis. negative Paster’s effect - great amount of sub-oxidized products occurs after decomposition of carbohydrates, particularly, lactic acid. Protein atypia - appearance of unusual proteins during certain kinds of tumors. The presence of these proteins, also called embryony proteins or Abbel’s proteins, is a diagnostic test for hepatoma identification.
- 21. Characteristics Unique to Malignant Neoplasms Functional anaplasia Normal cells stop their division when they contact surrounding cells, and that is called contact inhibition. Tumor cells do not stop their division even when they contact surrounding cells. Thus they destroy healthy cells and grow into the surrounding tissue. Autonomy (independence from the organism) Tumor cells get out of control of regulating systems of the organism (nervous, endocrine, immune).
- 22. Characteristics Unique to Malignant Neoplasms Loss of polaruty and specialized functions Normal differentiated cells are polar and possess specialized functions. Anaplastic cells lose their polarity and specialized functions. The more severe is the anaplasia, the more polarity and specialized functions are impaired. The less severe the anaplasia, the more cells show polarity and specialized functions.
- 23. Characteristics Unique to Malignant Neoplasms Invasion Malignant cells lose their attachment to their neighbors, move about on their own, and secrete substances that dissolve surrounding ground substance and collagen fibers.
- 24. Characteristics Unique to Malignant Neoplasms Invasive malignancies are difficult to eradicate. There is no line of demarcation around malignant neoplasms As malignant cells invade they infiltrate important structures—nerves, ducts, bone marrow. Malignant cells can invade lymphatic and blood vessels providing ready access to body regions far from their point of origin.
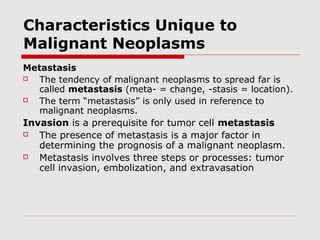
- 25. Characteristics Unique to Malignant Neoplasms Metastasis The tendency of malignant neoplasms to spread far is called metastasis (meta- = change, -stasis = location). The term “metastasis” is only used in reference to malignant neoplasms. Invasion is a prerequisite for tumor cell metastasis The presence of metastasis is a major factor in determining the prognosis of a malignant neoplasm. Metastasis involves three steps or processes: tumor cell invasion, embolization, and extravasation
- 26. Invasion and metastasis of malignant tumor cells Tumor cell invasion. The sequence of events: detachment of tumor cells from the primary tumor; attachment to basement membrane matrix; degradation of basement membrane matrix; locomotion and infiltration of tumor cells; degradation of extracellular matrix; degradation of vascular basement membrane matrix.
- 27. Invasion and metastasis of malignant tumor cells Tumor Cell Embolization. Malignant tumor cells may invade lymphatic or blood vessels and enter the circulation. Only an extremely small number of embolized cells are able to establish metastatic lesions. The survival and growth of metastatic cells depends on the selection of cancer cells possessing specific properties needed for metastatic growth
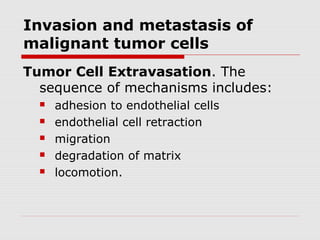
- 28. Invasion and metastasis of malignant tumor cells Tumor Cell Extravasation. The sequence of mechanisms includes: adhesion to endothelial cells endothelial cell retraction migration degradation of matrix locomotion.
- 29. Metastasis of tumor cells Malignant tumor cells may spread by three major routes: lymphatics, blood vessels, implantation (seeding) by physical contact between tumor and normal serosal or mucosal surfaces.
- 30. Other Differences between Benign and Malignant Neoplasms Benign Neoplasms growth pattern is known as expansive growth. Sometimes a fibrous connective tissue band surrounding the neoplasm—a capsule. When they arise from some surface, benign neoplasms almost always grow outward from the surface—a pattern known an exophytic growth. Benign neoplasms never invade surrounding tissues; they never metastasize; are composed of well- differentiated cells that resemble the tissue from which they originated. Cells of benign neoplasms stay attached to each other. Because of their cohesiveness, they do not enter blood or lymphatic vessels to spread elsewhere.
- 31. Other Differences between Benign and Malignant Neoplasms Malignant neoplasms grow rapidly and have the capacity to invade surrounding tissues. They are not well demarcated from the surrounding tissues—there is no capsule. If they arise from some surface, malignant neoplasms grow inward invading the underlying tissues, a pattern called endophytic growth. Metastatic malignant neoplasms cause severe body wasting—cachexia. Cachexia is loss of weight, muscle atrophy, fatigue, weakness and anorexia. Cachexia is often seen in end-stage cancer, and in that context is called "cancer cachexia".
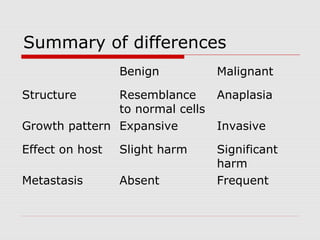
- 32. Summary of differences Benign Malignant Structure Resemblance to normal cells Anaplasia Growth pattern Expansive Invasive Effect on host Slight harm Significant harm Metastasis Absent Frequent
- 33. Summary of differences Benign Malignant Relapses As a rule - no Gives relapses Cachexia Only in case of GIT of tumor location (in esophagus) As usual Encapsulation Present Absent
- 34. How tumor cell escape immune surveilance low immunogenicity of tumor antigens constant modification of tumor antigens clonal selection of immune resistant tumor cells expression of embryonic antigens absence of MHC molecules (low differentiation of tumor cells) resistance to apoptosis depression of immune system by producing specific inhibitory cytokines (IL-8).
- 35. Organism defense against tumor anticarcinogenic mechanisms antimutational mechanisms anticellular mechanisms
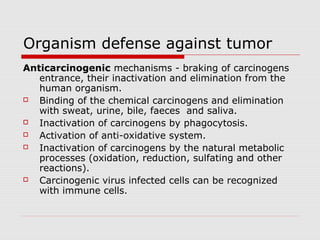
- 36. Organism defense against tumor Anticarcinogenic mechanisms - braking of carcinogens entrance, their inactivation and elimination from the human organism. Binding of the chemical carcinogens and elimination with sweat, urine, bile, faeces and saliva. Inactivation of carcinogens by phagocytosis. Activation of anti-oxidative system. Inactivation of carcinogens by the natural metabolic processes (oxidation, reduction, sulfating and other reactions). Carcinogenic virus infected cells can be recognized with immune cells.
- 37. Organism defense against tumor Antimutational mechanisms provide revealing, elimination or inhibition of oncogenes activity with the help of tumor suppressor gene (anti-oncogenes) or DNA reparative systems. Anticellular mechanisms provide recognition and destruction of tumor cells or inhibition of their division process. Non-immune cellular mechanisms - phagocytes and NK cells. Non-immune humoral mechanisms - tumor necrosis factor alpha (TNF). Immune mechanisms are represented by cellular immunity (cytotoxic T-cells – T-killers) and humoral immunity (specific antibodies formation).
- 38. Organism defense against tumor TNF is released primarily by WBC and endothelium. Stimulating of the corticotropin releasing hormone (CRH) release in the hypothalamus Suppressing appetite (hence its name "cachexin"). Fever. Activates liver function (C-reactive protein). Oncolytic effect of TNF is provided due to its ability: To attract neutrophils To stimulate phagocytosis and activate “respiratory burst” in phagocytes To activate thrombogenesis in the vessels of tumor
- 39. Interrelations between the host organism and the tumor Peculiarities of tumor Location is of critical importance with both benign and malignant tumors (e.g. adenoma compress hypophysis; carcinoma within the common bile duct may induce fatal biliary tract obstruction). The production of hormones. (pancreatic adenoma often produces hyperinsulinism). Ulceration through a surface with consequent bleeding or secondary infection Intussusception— leading to ulceration of the mucosa or intestinal obstruction or infarction.
- 40. Interrelations between the host organism and the tumor Cancer Cachexia is a progressive loss of body weight accompanied by profound weakness, anorexia, and anemia. Small, localized cancers therefore are generally silent and produce no cachexia, but there are exceptions. The origins of cancer cachexia: Anorexia - due to abnormalities in taste and in the central control of appetite. High basal metabolic rate. TNF suppresses appetite and inhibits the action of lipoprotein lipase, thereby inhibiting the release of free fatty acids from lipoproteins.
- 41. Interrelations between the host organism and the tumor The paraneoplastic syndromes: hypercalcemia, Cushing's syndrome, and nonbacterial thrombotic endocarditis. Cushing’s syndrome as a paraneoplastic phenomenon is usually related to ectopic production by the cancer of ACTH or ACTH-like polypeptides. The mediation of hypercalcemia may be caused by the cancer secretion of a parathyroid hormone-like peptide. Paraneoplastic syndromes may take many other forms, such as hypercoagulability leading to venous thrombosis and nonbacterial thrombotic endocarditis.
- 42. Cancer grading and staging The cancer may be classified as grade: I, II, III, or IV, in order of increasing anaplasia. normal
- 43. Cancer grading and staging Staging of a malignant neoplasm assesses its amount of invasion and metastasis. TNM system: T for primary tumor (T1-4) N for regional lymph node involvement (N1-4) M for metastases (M0,M1)
- 44. Treatment of Neoplasms Surgery.” Situations in which little surrounding tissue needs to be sacrificed is called “simple surgical excision”. Surgery performed for lesions that have invaded is often described as “radical” because much surrounding tissue is sacrificed. Radiation kills cells which are dividin. Radiation therapy and surgery are often used together. Chemotherapy. Certain chemicals affect cell which are in mitosis process.
- 45. Treatment of neoplasms Immunotherapy. Stimulation of immune system to attack cancer cells (BCG). Hormone Therapy. Some neoplasms are hormone- dependent. Cryotherapy is used for surface lesions where the freezing agent can be controlled accurately. Electosurgery resembles scalpel surgery with two exceptions. First, an electric current makes a wire loop hot enough to cut tissue. Second, the tissue around the edge of the surgical specimen is incinerated.