Goniometry.ppt uche
- 2. OUTLINE What is goniometry ? Importance of goniometry Types of goniometer Universal Goniometer Range of Motion Planes and Axes of joint motion Important Notes Procedures for Goniometric measurement ROM measurement Current Trends References 9/15/2015 2
- 3. WHAT IS GONIOMETRY Goniometry is the measuring of angles created by the bones of the body at the joints.1, 2, 3 The term goniometry is derived from two Greek words, gonia meaning angle and metron, meaning measure. 1, 2, 3, 4, 5, System to measure the joint ranges in each plane of the joint is termed goniometry. 4 These measurements are done with instrument such as goniometer, a tape measure, inclinometers or by visual estimate. 1, 2, 3, 4, 5 9/15/2015 3
- 4. IMPORTANCE OF GONIOMETRY Goniometry is useful in determining the presence of dysfunction establishing a diagnosis developing goals evaluating progress, fabricating orthoses a measurement for research purposes 4, 5, 6 9/15/2015 4
- 5. TYPES OF GONIOMETERS Universal goniometer Gravity goniometer/ inclinometer Electro goniometer sensor with angle meter Single and twin axis goniometer 9/15/2015 5
- 6. Bubble goniometer Smartphone soft wares Digital goniometer Arthroidal protractor 9/15/2015 6
- 7. UNIVERSAL GONIOMETER A universal goniometer may be constructed of metal or plastic and it has three parts A body Fulcrum Stationary arms Moving arms The body of the goniometer is designed like a protractor and may form a full or half circle; and on it is a scale from 0 to 180 or 360 1, 2, 3 The fulcrum is a rivet or screw-like device at the center of the body that allows the moving arm to move freely on the body of the device.1, 2, 3, 4, 5 6, 9/15/2015 7
- 8. UNIVERSAL GONIOMETER The fulcrum and body is placed over the joint being measured 3, 4, 5, 6, 7, 8 The stationary arm will be aligned with the inactive part of the joint measured while the moving arm is placed on the part of the limb which is moved in the joint’s motion1, 2, 3, 4, 5, 6, 7. 9/15/2015 8
- 9. 9/15/2015 9
- 10. RANGE OF MOTION Range of motion can be defined as the amount of motion available at a joint. 5 Each specific joint has a normal range of motion that is expressed in degrees. 1 Joint ranges are divided into Active range of motion AROM Passive range of motion PROM The structure involved with movement of the bones as well as the bony arrangements are factors in limiting motion. 1, 2, 3,4. 9/15/2015 10
- 11. RANGE OF MOTION Determinants of joint ROM Normal Age Gender Others such as ADL, right vs left, body physique, active vs passive ROM Abnormal Tight soft tissues around the joint Muscle insufficiency Adhesion Foreign body 9/15/2015 11
- 12. RANGE OF MOTION The end-feel is the feeling which is experienced by the examiner as a barrier to further motion at the end of a PROM. These normal end-feels have been described as soft, firm, and hard. The same terms are used to describe abnormal end-feels with the addition of "empty". 1, 2, 3 9/15/2015 12
- 13. RANGE OF MOTION Contraindications to ROM testing: Dislocation or unhealed fracture in the region, immediately following surgery, On medication for pain or muscle relaxants (careful) Regions of osteoporosis or bone fragility, Patients with hemophilia, Immediately after an injury where disruption of tissue is present. 9/15/2015 13
- 14. PLANES AND AXES OF JOINT MOTION Motion at a joint occurs as a result of movement of one joint surface in relation to another. 1 Arthrokinematics is the term used to refer to the movement of joint surfaces. The movements at the joint surfaces are described as slides (glides), spins, and rolls. These three usually occur in combination with each other and result in movement of the shafts of the bones. 1, 2, 3, 4, 5, 9, Osteokinematics refers to the movement of the shafts of the bones. These are usually described in terms of rotary movement about an axis of motion. 1, 2, 3 9/15/2015 14
- 15. PLANES AND AXES OF JOINT MOTION Goniometry measures the angles created by the rotary motion of the shafts of the bones.1, 2, 3, 4 Osteokinematic motions are classically described as taking place in one of the three cardinal planes of the body (sagittal, frontal, and transverse) around three corresponding axes (medial-lateral, anterior-posterior, and vertical). The three planes lie at right angles to one another whereas the three axes are both at right angles to the corresponding plane and to each other.1, 2, 3, 4 9/15/2015 15
- 16. PLANES AND AXES OF MOVEMENT ANATOMICAL POSITION 9/15/2015 16
- 17. VALIDITY AND RELIABILITY OF GONIOMETER According to the American Academy of Orthopeadic Surgeons, Kendall and McCreary, Hoppenfeld, and the American Medical Association. 1, 2, 3, 4, 5, 6, 7 Content validity – it is assumed that the angle created by aligning the arms of the goniometer with bony landmarks truly represents the angle. “The accurate application of knowledge and skills, combined with interpreting the results as measurement of range of motion only, provide sufficient evidence to ensure content validity.” Reliability – overall good to excellent reliability. Higher reliability has been found for measurements of joint position compared to range of motion. 9/15/2015 17
- 18. VALIDITY AND RELIABILITY OF GONIOMETER Reliability varies depending on the joint being measured. Intratester reliability is found to be higher than intertester reliability Advantages • Good reliability and validity. • Ease of use. • Inexpensive. •Can be used to establish presence or absence of dysfunction and also monitor progress Limitations • Reliability dependent on examiner experience. • Reliability varies depending on what joint is measured. • Requires consistency in positioning, stabilization, and alignment. • Some disagreement between sources for normal values of range of motion. 9/15/2015 18
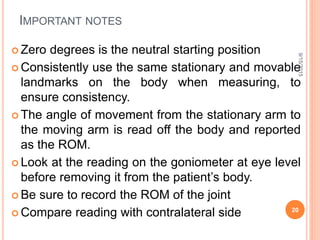
- 19. IMPORTANT NOTES The starting position for measuring all ROM is the anatomical position except for rotation in transverse plane. Be aware of the position the body is supposed to be in for movement and any stabilization issues. Stabilize the part of the body that is proximal (stationary portion) to the joint you are testing. The patient do not move his body while the moving the joint; this step isolates the joint movement for a more accurate measurement. There are three notation of goniometric measurement which are 0-180º, 180-0º and 0- 360º. 9/15/2015 19
- 20. IMPORTANT NOTES Zero degrees is the neutral starting position Consistently use the same stationary and movable landmarks on the body when measuring, to ensure consistency. The angle of movement from the stationary arm to the moving arm is read off the body and reported as the ROM. Look at the reading on the goniometer at eye level before removing it from the patient’s body. Be sure to record the ROM of the joint Compare reading with contralateral side 9/15/2015 20
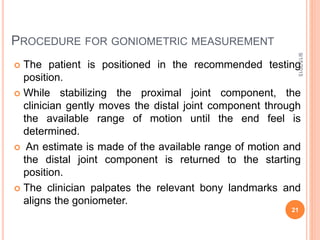
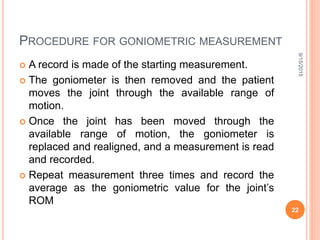
- 21. PROCEDURE FOR GONIOMETRIC MEASUREMENT The patient is positioned in the recommended testing position. While stabilizing the proximal joint component, the clinician gently moves the distal joint component through the available range of motion until the end feel is determined. An estimate is made of the available range of motion and the distal joint component is returned to the starting position. The clinician palpates the relevant bony landmarks and aligns the goniometer. 9/15/2015 21
- 22. PROCEDURE FOR GONIOMETRIC MEASUREMENT A record is made of the starting measurement. The goniometer is then removed and the patient moves the joint through the available range of motion. Once the joint has been moved through the available range of motion, the goniometer is replaced and realigned, and a measurement is read and recorded. Repeat measurement three times and record the average as the goniometric value for the joint’s ROM 9/15/2015 22
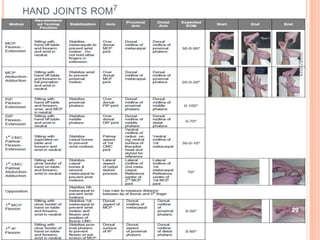
- 23. ROM MEASUREMENT Shoulder ROM Flexion: Motion: 0-180º Position: Subject supine with knees flexed or sitting. elbow extended with the palm facing the body Goniometer: Axis at the acromion process, laterally through the head of the humerus. Stationary arm is placed along the mid-axillary line of the trunk Moving arm place along the lateral mid-line of the humerus in line with the lateral epicondyle. Extension: Motion: 0-45º~60º from neutral position Position: Subject prone or sitting , elbow in slight flexion with the palm facing the body. Goniometer: Axis at the acromion process, laterally through the head of the humerus Stationary Arm aligned with mid- axillary line of the trunk Moving arm along the lateral mid-line of humerus in line with lateral epicondyle. 9/15/2015 23
- 24. Abduction: Motion:0-180º Position: Supine, prone or sitting with the limb in anatomic position Goniometer: Axis at anterior portion of acromion process. Stationary arm at lateral aspect of anterior surface of chest parallel to midline of sternum. Moving arm on anterior aspect of arm parallel to midline of humerus and in line with medial epicondyle. OR Goniometer: Axis at the posterior portion of the acromion process; Stationary arm aligned parallel to spinous process of the vertebral colomn Moving arm aligned with the midline of the humerus in line with lateral epicondyle Adduction: Motion: 0-30º Aligment of goniometer is same for abduction. 9/15/2015 24
- 25. External rotation: Motion: 0-90º Position: Supine. Shoulder is abducted to 90º. Elbow flexed with forearm in neutral and perpendicular to table top such that the palm is facing the feet. Elbow not supported. Humerus is fully supported on the table. Stabilize the distal humerus, thorax, and scapula. Goniometer: Axis at olecranon process of the ulna. Stationary arm placed parallel to the table top or perpendicular to the floor. Moving arm along the ulnar shaft aligned with the styloid process of the ulna. Internal rotation: Motion: 0-65~90º Positioning and goniometer alignment is same as in external rotation 9/15/2015 25
- 26. Radio-ulnar ROM Supination: Motion: 0- 80º~ 90º Position: Subject sitting or supine, with the elbow flexed to 90º. Shoulder in zero degrees of its’ ROM. Position starts midway between Supination and Pronation. Goniometer: Axis is medial to the ulnar styloid process. Stationary arm is aligned parallel to the anterior midline of the humerus. Moving arm across the ventral aspect of the wrist on a line between and proximal to the styloid process of the radius and the ulna. Pronation: Motion: 0- 80º~ 90º Position: same for supination Goniometer: Axis is lateral to the ulnar styloid process. Stationary arm is aligned parallel to the anterior midline of the humerus. Moving arm across the dorsum of the wrist on a line between and proximal to the styloid process of the radius and the ulna. 9/15/2015 27
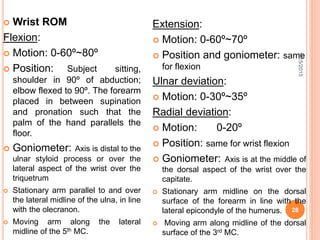
- 27. Wrist ROM Flexion: Motion: 0-60º~80º Position: Subject sitting, shoulder in 90º of abduction; elbow flexed to 90º. The forearm placed in between supination and pronation such that the palm of the hand parallels the floor. Goniometer: Axis is distal to the ulnar styloid process or over the lateral aspect of the wrist over the triquetrum Stationary arm parallel to and over the lateral midline of the ulna, in line with the olecranon. Moving arm along the lateral midline of the 5th MC. Extension: Motion: 0-60º~70º Position and goniometer: same for flexion Ulnar deviation: Motion: 0-30º~35º Radial deviation: Motion: 0-20º Position: same for wrist flexion Goniometer: Axis is at the middle of the dorsal aspect of the wrist over the capitate. Stationary arm midline on the dorsal surface of the forearm in line with the lateral epicondyle of the humerus. Moving arm along midline of the dorsal surface of the 3rd MC. 9/15/2015 28
- 29. Hip ROM Flexion: Motion: 0-100º~125º Position: Supine or side lying on the opposite limb to be measured; limb in anatomical position with knee flexed at the end of the motion. Goniometer: Place the axis at the lateral aspect of the hip joint over the greater trochanter. stationary arm is parallel to the long axis of the trunk in line with the greater trochanter or the lateral midline of the pelvis moving arm is placed along the lateral midline of the femur in line with lateral epicondyle of the femur Extension: Motion: 0-10º~30º Position: Prone or Side lying on the opposite limb to measured; the limb in anatomical position Goniometer alignment is the same for hip flexion. *Stabilise the pelvis when measuring hip flexion and extension. 9/15/2015 30
- 30. Abduction: Motion: 0 - 40º~50º Position: Supine with the limb in anatomical position (0º of all limb joints ROM) Goniometer: axis at the anterior superior iliac spine(ASIS) of the measured limb. Stationary arm is at an imaginary horizontal line extending from one ASIS to the other. Moving arm is with the anterior midline of the femur, in line with the midline of the patella. Adduction: Motion: 0-20º~30º Position: Supine, with opposite limb abducted Goniometer alignment is same as for hip abduction *Stabilise the pelvis 9/15/2015 31
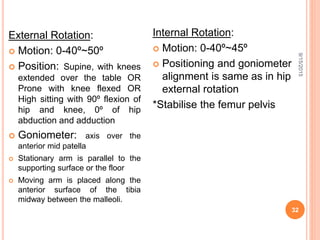
- 31. External Rotation: Motion: 0-40º~50º Position: Supine, with knees extended over the table OR Prone with knee flexed OR High sitting with 90º flexion of hip and knee, 0º of hip abduction and adduction Goniometer: axis over the anterior mid patella Stationary arm is parallel to the supporting surface or the floor Moving arm is placed along the anterior surface of the tibia midway between the malleoli. Internal Rotation: Motion: 0-40º~45º Positioning and goniometer alignment is same as in hip external rotation *Stabilise the femur pelvis 9/15/2015 32
- 32. Knee ROM Flexion: Motion: 0-135º~150º Position: Supine, knees in extension with hip flexed to 90o at end of the motion OR prone lying with knee extended foot over the edge of the supporting surface. Goniometer: Axis is placed over the lateral epicondyle of the femur Stationary arm is parallel to the lateral midline of the femur in line with the greater trochanter Moving arm is placed lateral at the midline of the fibula in line with the lateral malleolus. Extension: Motion: note any hyperextension Positioning and goniometer alignment is same with knee flexion. Extension is an opposite motion to flexion *The thigh should be stabilized in flexion motion measurement 9/15/2015 33
- 33. Ankle ROM Dorsiflexion: Motion:0-20º Position: Subject was sitting with legs off the table or on high sitting with lower leg at right angle to the thigh and the foot at right angle to the lower leg as the zero starting position. Goniometer: fulcrum was aligned slightly inferior to the lateral malleolus. Stationary arm is with the midline of the lateral aspect of the lower leg, in line with the head of fibula. Moving arm was parallel to the 5th metatarsal. Plantarflexion: Motion:0-40º~50º Positioning and goniometer alignment is same with dorsiflexion Inversion: Motion:0-15º~20º Position: same with dorsiflexion Goniometer: axis is midway between the two malleoli at the anterior aspect of the ankle Stationary arm is with the anterior midline of tibia in line with the tibial tuberosity Moving arm is with the anterior midline of the 2nd metatarsal. 9/15/2015 34
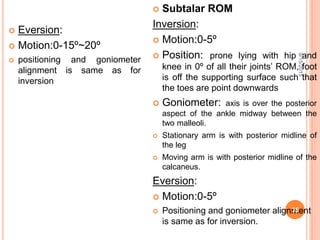
- 34. Eversion: Motion:0-15º~20º positioning and goniometer alignment is same as for inversion Subtalar ROM Inversion: Motion:0-5º Position: prone lying with hip and knee in 0º of all their joints’ ROM, foot is off the supporting surface such that the toes are point downwards Goniometer: axis is over the posterior aspect of the ankle midway between the two malleoli. Stationary arm is with posterior midline of the leg Moving arm is with posterior midline of the calcaneus. Eversion: Motion:0-5º Positioning and goniometer alignment is same as for inversion. 9/15/2015 35
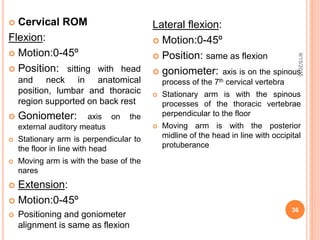
- 35. Cervical ROM Flexion: Motion:0-45º Position: sitting with head and neck in anatomical position, lumbar and thoracic region supported on back rest Goniometer: axis on the external auditory meatus Stationary arm is perpendicular to the floor in line with head Moving arm is with the base of the nares Extension: Motion:0-45º Positioning and goniometer alignment is same as flexion Lateral flexion: Motion:0-45º Position: same as flexion goniometer: axis is on the spinous process of the 7th cervical vertebra Stationary arm is with the spinous processes of the thoracic vertebrae perpendicular to the floor Moving arm is with the posterior midline of the head in line with occipital protuberance 9/15/2015 36
- 36. Rotation: Motion: 0-60º~80º Position: same as for flexion Goniometer: axis over the centre of the cranial aspect of the head Stationary arm in line with an imaginary line between the two acromial processes Moving arm is with the tip of the nose Lumbar ROM Flexion: Motion: 4inches Position: standing and in anatomical position Tape Measure: Placed proximately at the C7 spinous process and distally at S1; calculate the difference between standing and flexion ending position. Extension: Motion:2inches Position: same with flexion Tape Measure: Placed proximately at the C7 spinous process and distally at S1; calculate the difference between standing and extension ending position. 9/15/2015 37
- 37. Lateral flexion: Motion: 0-25º~35º Position: same as flexion Goniometer: axis over the spinous process of 1st sacral vertebra Stationary arm is perpendicular to the floor Moving arm is in line with the spinous process of the of the 7th cervical vertebra Tape Measure: Placed proximally at the finger tips and distally at the lateral malleolus; calculate the difference between sides when standing and with side bending. Rotation: Motion:0-30º~45º Position: same as flexion Goniometer: axis at the centre of the cranial aspect of the head Stationary arm is parallel with the imaginary line between the two prominent tubercles on the iliac crest. Moving arm is with an imaginary line between the two acromial processes 9/15/2015 38
- 38. CURRENT TRENDS The use of inclinometer software to measure ROM in a joint. In a study by Brian et al, (2013), it was inferred that Smart phones have good correlation with the “gold standard” goniometer for measuring shoulder range of motion. Additionally, there is good correlation amongst different levels of providers with measurements obtained using the smart phone Drgoniometer 12 The use of sensor and goniometer probe setup to measure joint ROM. It usually convenient for large joints It is designed as a sensor pad connected to a potentiometer or a probe connected to a sensor angle meter 7, 8 9/15/2015 39
- 39. 9/15/2015 40
- 40. Example of goniometric measurement using DrGoniometer as it appears on the smartphone screen 9/15/2015 41
- 41. CONCLUSION Goniometric measurement is an important skill all physiotherapist must have as it employed in almost all area of physiotherapy practice. There are different instrument for measurement of joint’s range of motion but the universal goniometre remains the gold standard due to it’s excellent validity and reliability in most articles. It also has advantages such as ease of use, inexpensive, easily available and accuracy. Though some other instrument are as reliable and valid as the universal goniometer but the cost of purchase, availability and ease of use may not be met. 9/15/2015 42
- 42. REFERNCES 1. Norkin, C.C. & White, D.C. (1988) Techniques and procedures, in Measurement of joint motion: A guide to goniometry. In Norkin & White, Eds. FA Davis: Philadelphia. p. 9-24. 2. Norkin, & White.(1995) Measurement of Joint Motion: A Guide to Goniometry. 2nd ed. Philadelphia, PA: F.A. Davis Company. 3. Norkin, & White.(2003) Measurement of Joint Motion: A Guide to Goniometry. 3rd ed. Philadelphia, PA: F.A. Davis Company;. 4. The British Orthopaedic Association (1983) Joint motion: method of measuring and recording. In Heck, C.V., Hendryson, I.E., Rowe, C.R. (eds). Edinburg: Churchill Livingstone. 5. Gadjosik, & Bohannon(1987) Clinical measurement of range of motion: review of goniometry emphasizing reliability and validity. Physical Therapy; 67: 1867-1872. 6. Gogia, Braatz, Rose, & Norton.(1987) Reliability and validity of goniometric measurements at the knee. Physical Therapy; 67: 192-195. 7. Nadeau, Kovacs, Gravel, Piotte, Moffet, Gagnon, & Hebert.(2007) Active movement measurements of the shoulder girdle in healthy subjects with goniometer and tape measure techniques: A study on reliability and validity. Physiotherapy Theory and Practice.; 23: 179-187. 8. Brian, C.W., Chris, M.K., Justin, W.G., Matthew, L.L., Joseph, M.H., & Stephen F.B.(2013) Shoulder Range of Motion: Validation of an Innovative Measurement Method Using a Smartphone The Orthopaedic Journal of Sports Medicine, 1(4)(suppl 1) 9. MacDermid, et al.(1999) Range of motion measurement. Journal of Hand Therapy; 12:187-192. 9/15/2015 43
- 43. REFERNCES 10. Rasmussen, O.(1985) Stability of the ankle joint. Acta Orthop. Scandinavica; Suppl. 211: p. 56-78. 11. Seto, J.L. & Brewster,C.E.(1985) Treatment approaches following foot and ankle injury. Clinical Sports Medicine; 13: p. 295 12. Ferriero,G., Sartorio, F., Foti,C., Primavera,D., Brigatti, E.& Vercelli, S. (2012) Reliability of a New Application for Smartphones (DrGoniometer) for Elbow Angle Measurement. The American Academy of Physical Medicine and Rehabilitation; Vol. 3:1153-1154 9/15/2015 44
- 44. 9/15/2015 45