Keratometry
- 1. KERATOMETRY Dr Saurabh Kushwaha Resident Ophthalmology
- 2. SCOPE Introduction Principle of Keratometry Methods of Kertaometery Automated Keratometer Clinical Applications Limitations Sources of errors
- 3. INTRODUCTION Keratometry is measurement of curvature of the anterior surface of cornea across a fixed chord length, usually 2-3 mm, which lies within the optical spherical zone of cornea. Kerato : Cornea Metry : Measurement Expressed in Dioptric power
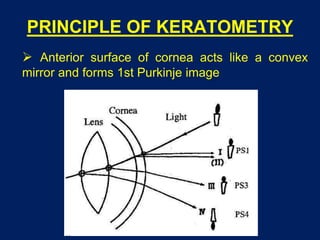
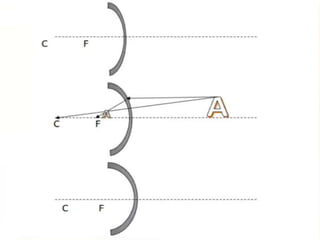
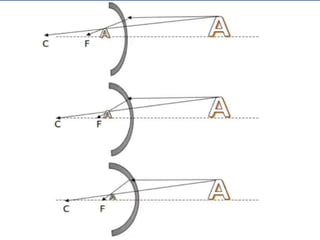
- 4. PRINCIPLE OF KERATOMETRY Anterior surface of cornea acts like a convex mirror and forms 1st Purkinje image
- 8. PRINCIPLE OF KERATOMETRY The curvature of the anterior surface of cornea determines the size of the 1st Purkinje image Greater the curvature of cornea, lesser is the image size If the object size and distance is known and the 1st Purkinje image is determined, then the curvature of anterior corneal surface can be calculated
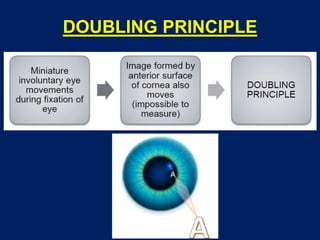
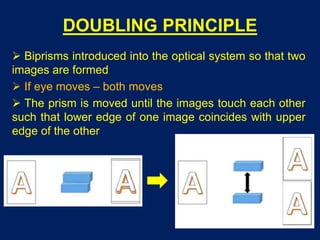
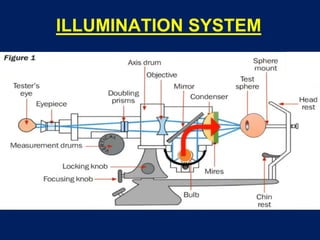
- 10. DOUBLING PRINCIPLE Biprisms introduced into the optical system so that two images are formed If eye moves – both moves The prism is moved until the images touch each other such that lower edge of one image coincides with upper edge of the other
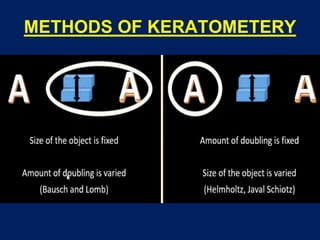
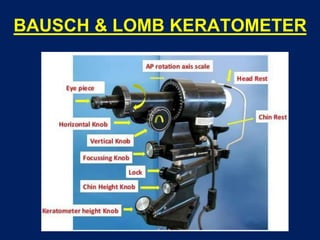
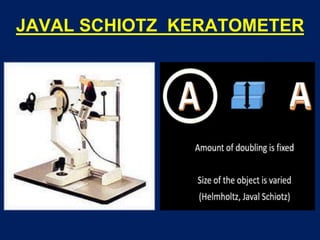
- 12. BAUSCH & LOMB KERATOMETER
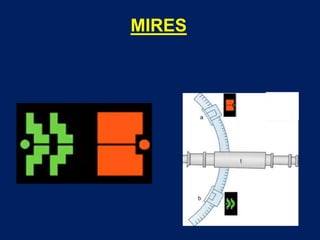
- 15. MIRES Circular Forms an image on the cornea
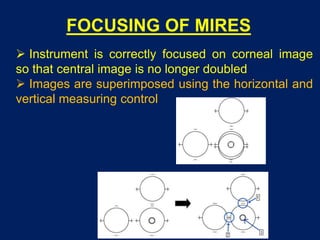
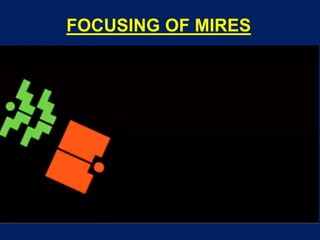
- 16. FOCUSING OF MIRES Instrument is correctly focused on corneal image so that central image is no longer doubled Images are superimposed using the horizontal and vertical measuring control
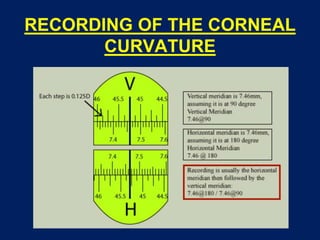
- 17. RECORDING OF THE CORNEAL CURVATURE
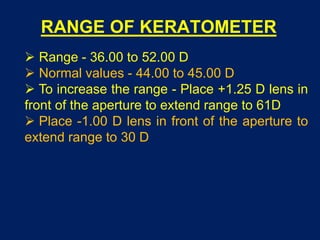
- 18. RANGE OF KERATOMETER Range - 36.00 to 52.00 D Normal values - 44.00 to 45.00 D To increase the range - Place +1.25 D lens in front of the aperture to extend range to 61D Place -1.00 D lens in front of the aperture to extend range to 30 D
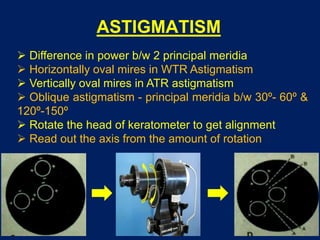
- 19. ASTIGMATISM Difference in power b/w 2 principal meridia Horizontally oval mires in WTR Astigmatism Vertically oval mires in ATR astigmatism Oblique astigmatism - principal meridia b/w 30º- 60º & 120º-150º Rotate the head of keratometer to get alignment Read out the axis from the amount of rotation
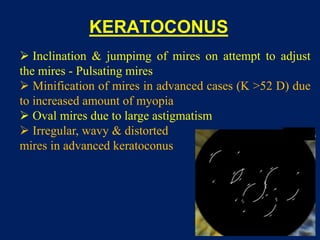
- 20. KERATOCONUS Inclination & jumpimg of mires on attempt to adjust the mires - Pulsating mires Minification of mires in advanced cases (K >52 D) due to increased amount of myopia Oval mires due to large astigmatism Irregular, wavy & distorted mires in advanced keratoconus
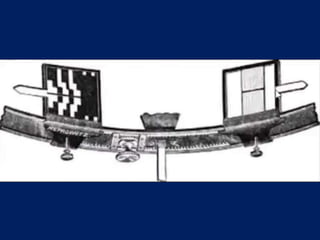
- 22. MIRES
- 24. OPTICAL SYSTEM
- 28. KERATOMETERS Ziess Oberkochen Keratometer Humphrey Keratometer
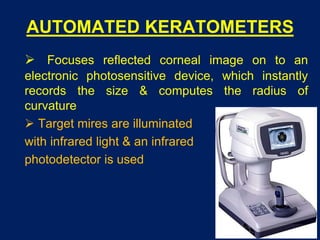
- 29. AUTOMATED KERATOMETERS Focuses reflected corneal image on to an electronic photosensitive device, which instantly records the size & computes the radius of curvature Target mires are illuminated with infrared light & an infrared photodetector is used
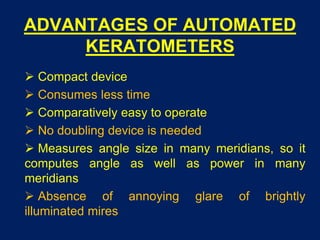
- 30. ADVANTAGES OF AUTOMATED KERATOMETERS Compact device Consumes less time Comparatively easy to operate No doubling device is needed Measures angle size in many meridians, so it computes angle as well as power in many meridians Absence of annoying glare of brightly illuminated mires
- 31. CLINICAL APPLICATIONS OF KERATOMETERS Helps in measurement of corneal astigmatic error Helps to estimate radius of curvature of the anterior surface of cornea - Use in contact lens fitting Monitors shape of the cornea - Keratoconus - Keratoglobus To monitor pre- & post-surgical astigmatism IOL power calculation Used for differential diagnosis of axial versus curvatural anisometropia
- 32. LIMITATIONS OF KERATOMETRY Measurements of keratometer based on false assumption that cornea is a symmetrical spherical or spherocylindrical structure, with 2 principal meridia separated from each other by 90° Measures refractive status of small central cornea (3-4 mm) Loses accuracy when measuring very flat or very steep cornea Small corneal irregularities preclude use of keratometer due to irregular astigmatism It cannot describe corneal asphericity
- 33. SOURCES OF ERRORS IN KERATOMETRY Improper calibration Faulty positioning of patient Improper fixation by patient Localized corneal distortion Abnormal lid positioning Improper focusing of the corneal image
- 34. THANK YOU