Ocular side effects of systemic drugs
- 1. OCULAR SIDE EFFECTS OF SYSTEMIC DRUGS PRESENTER- ANJU NAGAR DATE : 15-4-2013
- 2. Introduction • After a drug molecule enters the systemic circulation, it can reach ocular tissues through uveal or retinal circulations. • The choroid, sclera and ciliary body have thin, fenestrated walls for drug molecules to pass. • Small, lipid soluble molecules pass freely into the aqueous humor, and can further diffuse into avascular structures such as the lens, cornea, and trabecular meshwork
- 3. Introduction Drug molecules that enter by means of the uveal circulation exit the eye from the Canal of Schlemm, ciliary body or may diffuse into adjacent anatomical structures. Drugs from the retinal circulation can re-enter the systemic circulation, diffuse into the vitreous and anatomical structures, or get actively transported out.
- 4. Ocular Accumulation Sites Three major accumulation sites- cornea, lens and vitreous. The duration of drug in the eye is prolonged if deposited, increasing chances for toxicity. The cornea has a permeable endothelium, and the stromal glycosaminoglycans (GAGs) can bind drug molecules, leading to edema and decreased transparency. Drug molecules can also bind to lens protein, and photosensitize the lens to ultraviolet (UV) radiation. Lastly, drug molecules tend to accumulate in the vitreous due to the slow rate of fluid exchange.
- 5. MELANIN BINDING • Melanin absorbs light and damage results from the free- radical nature of melanin in structures such as the uveal tract and the RPE. • Chloroquine and chlorpromazine have a high affinity to melanin and tend to affect ocular tissues
- 6. DRUG METABOLISM • The body’s ability to metabolize a drug directly correlates with toxicity. • In patients with hepatic and renal disease, there is a decreased rate of excretion, which allows drug molecules to accumulate to toxic levels. • Also, toxic metabolites formed elsewhere like the liver, can reach the eye through systemic circulation or can be produced locally in ocular tissues.
- 7. PHOTOSENSITIZERS The adult crystalline lens normally filters most ultra-violet ( UV) radiation, so there is minimal risk of UV affecting the retina, where drug molecules can potentially bind. UV radiation does affect anterior tissues like the cornea and lens when photosensitized by bound drug molecules. Exposed lens proteins, when UV photosensitized by bound drug molecules, may denature, opacify and accumulate leading to cataract formation.
- 8. PHOTOSENSITIZERS UV radiation can potentially affect the retina in aphakic and pseudophakic patients, because UV can penetrate without the normal absorptive lens barrier. Well-known photosensitizers that cause anterior subcapsular lens changes – allopurinol, phenothiazine, amiodarone, and chloroquine
- 9. Possible basis of ocular side effects of systemic drugs 1. Specific biochemical basis known: Antimuscarinic drugs Tamsulosin(alpha adrenergic blocker) Sildenafil (Block hyperpolarisation of photoreceptors) 2. Altered metabolism – increased drug concentration Therapeutic window Metabolism by liver/ kidney- ethambutol toxicity in renal impairment; digoxin. Different metabolism in young age Possibility of drug transfer Drug interaction
- 10. Possible basis of ocular side effects of systemic drugs 3. Predisposition to allergy in atopic individuals- Steven Johnson 4. Toxicity due to overdose quinine, Chloroquine 5. Teratogenecity 6. Idiopathic & idiosyncratic- side effects even at correct dose Diplopia- Glitazone, ethambutol, steroid, topiramate Floroquinolone. BIH- vitamin A Red tears- rifampicin in leprosy
- 11. Possible basis of ocular side effects of systemic drugs 7. Recreational drugs Canthaxanthin-gold dust retinopathy LSD Ayahuasca tea(hallucinogen) 8. Adverse new side effects
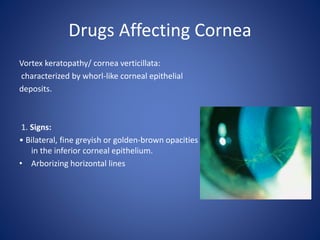
- 12. Drugs Affecting Cornea Vortex keratopathy/ cornea verticillata: characterized by whorl-like corneal epithelial deposits. 1. Signs: • Bilateral, fine greyish or golden-brown opacities in the inferior corneal epithelium. • Arborizing horizontal lines
- 13. Drugs Affecting Cornea Causes: a. Antimalarial Chloroquine (Nivaquine, Avlocor) Hydroxychloroquine (Plaquenil) • INDICATIONS: malaria; certain rheumatological disorders • Unlike retinopathy, keratopathy bears no relationship to dosage or duration of treatment. • reversible on cessation of therapy.
- 14. Drugs Affecting Cornea b. Amiodarone • INDICATIONS: atrial fibrillation; ventricular tachycardia • keratopathy - slowly reversible on discontinuation of medication. • Higher dose/ longer duration of administration more advanced the corneal deposits. • keratopathy does not affect vision- discontinuation not indicated. • Other toxic effects- anterior subcapsular lens deposits optic neuropathy
- 15. Drugs Affecting Cornea CHLORPROMAZINE: INDICATIONS- sedative; psychotic illnesses SIGNS- innocuous, subtle, diffuse yellowish-brown granular deposits in the endothelium, Descemet membrane and deep stroma occurring only in exposed cornea of the interpalpebral fissure anterior lens capsule deposits retinopathy Doses greater than 500 mg/day given for prolonged periods have a higher incidence of irreversible corneal and lenticular deposits.
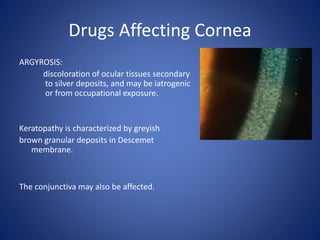
- 16. Drugs Affecting Cornea ARGYROSIS: discoloration of ocular tissues secondary to silver deposits, and may be iatrogenic or from occupational exposure. Keratopathy is characterized by greyish brown granular deposits in Descemet membrane. The conjunctiva may also be affected.
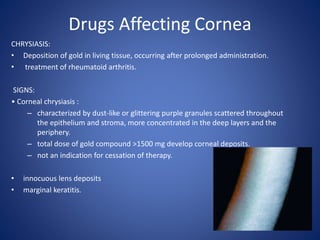
- 17. Drugs Affecting Cornea CHRYSIASIS: • Deposition of gold in living tissue, occurring after prolonged administration. • treatment of rheumatoid arthritis. SIGNS: • Corneal chrysiasis : – characterized by dust-like or glittering purple granules scattered throughout the epithelium and stroma, more concentrated in the deep layers and the periphery. – total dose of gold compound >1500 mg develop corneal deposits. – not an indication for cessation of therapy. • innocuous lens deposits • marginal keratitis.
- 18. Drugs Affecting Cornea AMANTADINE: INDICATIONS: Parkinson disease. SIGNS: • Diffuse white punctate opacities that may be associated with epithelial edema, 1–2 weeks after commencement of therapy (dose 200-400 mg/d). • Resolve with discontinuation of treatment.
- 19. Drugs Affecting Lens STEROIDS: cataractogenic; topical /systemic/nasal. • lens opacities: • PSC • later the anterior subcapsular – relationship between weekly systemic dose, duration of administration, total dose and cataract formation is unclear. – patients on less than 10 mg prednisolone (or equivalent), or treated for less than 4 years may be immune.
- 20. Drugs Affecting Lens – children- more susceptible to the cataractogenic effects of systemic steroids, individual (genetic) susceptibility may also be of relevance. – Early opacities may regress if therapy is discontinued; alternatively progression may occur despite withdrawal and warrant surgical intervention. – The etiology is unknown, the drug may react with amino groups of crystalline lens fibers causing protein complexes to aggregate
- 21. Drugs Affecting Lens CHLORPROMAZINE: • Deposition of innocuous, fine, stellate, yellowish-brown granules on the anterior lens capsule within the pupillary area • 50% of patients who have received a cumulative dose of 1000g. • The deposits persist despite discontinuation of the drug.
- 22. Drugs Affecting Lens BUSULPHAN (MYLERAN): INDICATIONS: Treatment of chronic myeloid leukemia. SIGNS: Occasionally cause lens opacities. GOLD: INDICATIONS: used in the treatment of rheumatoid arthritis SIGNS: Causes innocuous anterior capsular deposits in about 50% of patients on treatment for longer than 3 years.
- 23. Drugs Affecting Lens ALLOPURINOL: INDICATIONS: hyperuricaemia and chronic gout SIGNS: Increases the risk of cataract formation in elderly patients, if the cumulative dose exceeds 400 g or duration of administration exceeds 3 years. DESFERRIOXAMINE: can cause cataract
- 24. Drugs causing uveitis RIFABUTIN: INDICATIONS: Tuberculosis in combination with other drugs in immunocompetent patients. • Drugs that inhibit metabolism of rifabutin through the cytochrome p-450 pathway (clarithromycin and fluconazole), increase the risk of uveitis. SIGNS: ACUTE ANTERIOR UVEITIS (AAU) U/L; assoc with hypopyon; Treatment involves withdrawal of the drug or reduction of dose.
- 25. Drugs causing uveitis • BISPHOSPHONATES: osteoporosis. – FOSAMAX – AREDIA – ACTONEL Bisphosphonate molecules preferentially "stick" to calcium and bind to it. They accumulate to a high concentration in bones, resulting in maintained or increased bone density and strength Ocular Side Effects • Scleritis/Episcleritis • Blurred vision • Hyperemia • Anterior uveitis
- 26. Drugs causing uveitis Cidofovir INDICATION: CMV retinitis in AIDS patients. SIGNS: AAU- Vitritis is common and hypopyon may occur with long- term administration. Treatment- topical steroids and mydriatics.
- 27. Drugs affecting retina ANTIMALARIALS: Drugs Antimalarials- melanotropic drugs. Chloroquine retinotoxicity- related to the total cumulative dose(>300g), Rx duration > 3y Hydroxychloroquine - much safer than chloroquine The risk of toxicity is increased if a daily dose over 6.5 mg/kg is administered for longer than 5 years, although even then the risk is still very small.
- 28. CHLOROQUINE RETINOPATHY Chloroquine retinopathy can be divided into the following stages: 1. Premaculopathy – normal visual acuity and a scotoma to a red target located between 4° and 9° from fixation. – Amsler grid testing may also show a defect. – colour vision assessed- mild blue-yellow and protan red-green defects. (Adams Desaturation-15 test and the Hardy-Rand- Rittler test). – If the drug is discontinued, visual function usually returns to normal.
- 29. CHLOROQUINE RETINOPATHY 2. Early maculopathy modest reduction of visual acuity (6/9– 6/12). Fundus examination- subtle ‘bull’s eye’ macular lesion (central foveolar island of pigment surrounded by a depigmented zone of RPE atrophy, which is itself encircled by a hyperpigmented ring). may progress even if the drug is stopped.
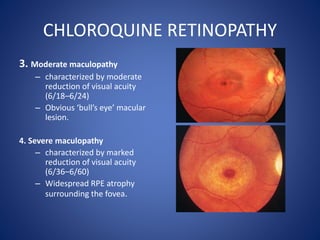
- 30. CHLOROQUINE RETINOPATHY 3. Moderate maculopathy – characterized by moderate reduction of visual acuity (6/18–6/24) – Obvious ‘bull’s eye’ macular lesion. 4. Severe maculopathy – characterized by marked reduction of visual acuity (6/36–6/60) – Widespread RPE atrophy surrounding the fovea.
- 31. CHLOROQUINE RETINOPATHY 5. End-stage maculopathy – Characterized by severe reduction of visual acuity – Marked atrophy of the RPE with unmasking of the larger choroidal blood vessels. – retinal arterioles may also become attenuated and pigment clumps develop in the peripheral retina.
- 32. DRUGS AFFECTING RETINA PHENOTHIAZINES: 1. Thioridazine: schizophrenia and related psychoses. – normal daily dose is 150– 600 mg. – Doses> 800 mg/day: cause reduced visual acuity and impairment of dark adaptation. The clinical signs of progressive retinotoxicity are : •‘Salt and pepper’ pigmentary disturbance involving the mid-periphery and posterior pole. Pigmented plaques and focal loss of the RPE and choriocapillaris
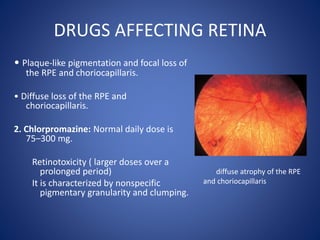
- 33. DRUGS AFFECTING RETINA • Plaque-like pigmentation and focal loss of the RPE and choriocapillaris. • Diffuse loss of the RPE and choriocapillaris. 2. Chlorpromazine: Normal daily dose is 75–300 mg. Retinotoxicity ( larger doses over a prolonged period) It is characterized by nonspecific pigmentary granularity and clumping. diffuse atrophy of the RPE and choriocapillaris
- 34. DRUG-INDUCED CRYSTALLINE MACULOPATHIES: 1. TAMOXIFEN : specific anti-oestrogen -breast carcinoma. Normal daily dose is 20–40 mg. SIGNS: Retinopathy- bilateral, superficial, fine, yellow, crystalline deposits in the inner layers of the retina and punctate grey lesions in the outer retina and RPE Visual impairment- caused by maculopathy associated with foveolar cyst formation. Optic neuritis- reversible on cessation of therapy.
- 35. DRUG-INDUCED CRYSTALLINE MACULOPATHIES 2. CANTHAXANTHIN: – carotenoid used to enhance sun tanning. – deposition of innocuous glistening yellow inner retinal deposits arranged symmetrically in a doughnut shape at the posterior poles- GOLD DUST RETINOPTHY – deposits are slowly reversible.
- 36. DRUG-INDUCED CRYSTALLINE MACULOPATHIES: 3. METHOXYFLURANE: – Inhalant general anaesthetic. – metabolized to oxalic acid which combines with calcium to form an insoluble salt which is deposited in tissues including the RPE. – Prolonged administration may lead to renal failure and secondary hyperoxalosis. Ocular involvement is characterized by- mild visual impairment associated with calcium oxalate crystals scattered throughout the retina that may later be associated with RPE hyperplasia at the posterior pole.
- 37. DRUG-INDUCED CRYSTALLINE MACULOPATHIES Interferon-alpha: chemotherapeutic Delayed type hypersensitivity reaction OCULAR SIGNS: • Retinopathy – – characterized by cotton wool spots and intraretinal haemorrhages (particularly high-dose therapy). – usually resolves spontaneously with cessation of therapy and in the majority of patients the visual prognosis is good. • Less common ocular side-effects – oculomotor nerve palsy, – optic disc edema – retinal vein occlusion.
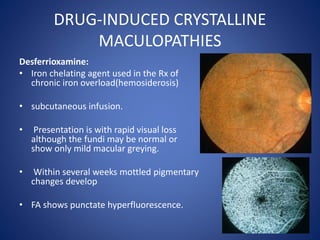
- 38. DRUG-INDUCED CRYSTALLINE MACULOPATHIES Desferrioxamine: • Iron chelating agent used in the Rx of chronic iron overload(hemosiderosis) • subcutaneous infusion. • Presentation is with rapid visual loss although the fundi may be normal or show only mild macular greying. • Within several weeks mottled pigmentary changes develop • FA shows punctate hyperfluorescence.
- 39. DRUG-INDUCED CRYSTALLINE MACULOPATHIES Nicotinic acid: Cholesterol-lowering agent. OCULAR SIGNS: – cystoid maculopathy suggestive of cystoid macular edema . – occur when doses greater than 1.5 g daily are used – resolve with discontinuation of the drug.
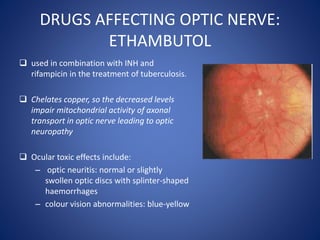
- 40. DRUGS AFFECTING OPTIC NERVE: ETHAMBUTOL used in combination with INH and rifampicin in the treatment of tuberculosis. Chelates copper, so the decreased levels impair mitochondrial activity of axonal transport in optic nerve leading to optic neuropathy Ocular toxic effects include: – optic neuritis: normal or slightly swollen optic discs with splinter-shaped haemorrhages – colour vision abnormalities: blue-yellow
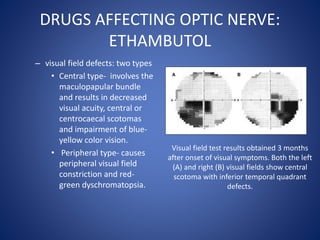
- 41. DRUGS AFFECTING OPTIC NERVE: ETHAMBUTOL – visual field defects: two types • Central type- involves the maculopapular bundle and results in decreased visual acuity, central or centrocaecal scotomas and impairment of blue- yellow color vision. • Peripheral type- causes peripheral visual field constriction and red- green dyschromatopsia. Visual field test results obtained 3 months after onset of visual symptoms. Both the left (A) and right (B) visual fields show central scotoma with inferior temporal quadrant defects.
- 42. DRUGS AFFECTING OPTIC NERVE: ETHAMBUTOL • Toxicity is dose- and duration- dependent; • the incidence is up to 6% at a daily dose of 25 mg/kg and rare with a daily dose not exceeding 15 mg/kg. • Toxicity typically occurs within 3–6 months of starting treatment. • Isoniazid may also rarely cause toxic optic neuropathy, particularly when given in combination with ethambutol.
- 43. DRUGS AFFECTING OPTIC NERVE: AMIODARONE Antiarrythmic Optic neuropathy: rare and not dose-related. Presentation is with insidious unilateral or bilateral visual impairment. Signs are bilateral optic disc swelling that may persist for a few months after medication is stopped. Visual field defects may be mild and reversible or severe and permanent. Cessation of the drug may not inevitably bring about improvement.
- 44. DRUGS AFFECTING OPTIC NERVE: VIGABATRIN • Second-line antiepileptic drug for the treatment of uncontrolled complex partial seizures • first line monotherapy for infantile spasms (West syndrome). • Presentation- – months or years after starting treatment – bilateral concentric or binasal visual field defects. – The defects persist if treatment is stopped but do not progress if medication is continued. This suggests that the defects are idiosyncratic rather than a dose-related effect.
- 45. DRUGS AFFECTING OPTIC NERVE: TOPIRAMATE • anticonvulsant • Also used in the treatment of migraine. • It can cause acute angle-closure glaucoma with associated myopia due to ciliochoroidal effusion. • Presentation is usually within a month of starting treatment with blurred vision, and sometimes haloes, ocular pain and redness.
- 46. DRUGS AFFECTING OPTIC NERVE: TOPIRAMATE • Signs include shallowing of the anterior chamber and raised intraocular pressure. • Treatment consists of reducing the intraocular pressure and stopping the drug. • Prognosis is usually good provided the complication is recognized.
- 47. DRUGS CAUSING DRY EYE 1. Beta blockers 2. Diuretics(change the tear film) 3. Niacin 4. Oral contraceptives 5. Antipsychotics (phenothiazines: thioridazine, chlorpromazine,), tricyclic antidepressant, anticholinergics(atropine, scoploamine) -anticholinergic properties. 6. Isotretinoin(decreased meibomian gland function- deficiency of normal lipid layer in tear film)
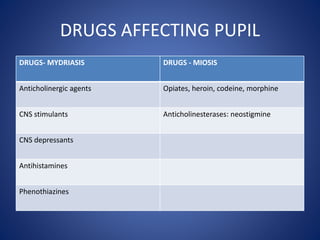
- 48. DRUGS AFFECTING PUPIL DRUGS- MYDRIASIS DRUGS - MIOSIS Anticholinergic agents Opiates, heroin, codeine, morphine CNS stimulants Anticholinesterases: neostigmine CNS depressants Antihistamines Phenothiazines
- 49. DRUGS CAUSING MYOPIA AND CYCLOPLEGIA MYOPIA CYCLOPLEGIA Sulfonamides Chloroquine Diuretics (chlorthalidone) Phenothiazine Carbonic anhydrase inhibitor anticholinergis Isotretinoin antihistamines Topiramate Anti-anxiety agents Tricyclic antidepressants
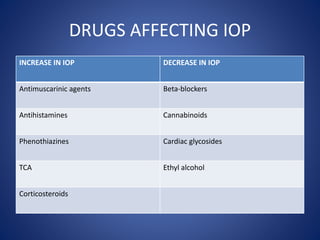
- 50. DRUGS AFFECTING IOP INCREASE IN IOP DECREASE IN IOP Antimuscarinic agents Beta-blockers Antihistamines Cannabinoids Phenothiazines Cardiac glycosides TCA Ethyl alcohol Corticosteroids
- 51. ANTICOAGULANTS • Aspirin (salicylate) • Coumadin (warfarin) • Heparin (unfractionated heparin) • Lovenox (enoxaparin sodium) • Plavix (clopidogrel) • Pradaxa (dabigatran etexilate mesylate) Ocular Side Effects • Subconjunctival and retinal hemorrhage • Recommend to be discontinued for a week prior to eye surgery • INR > 5 prone to bleed • Chronic use of ASA may cause yelllowing of vision
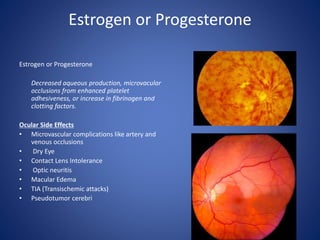
- 52. Estrogen or Progesterone Estrogen or Progesterone Decreased aqueous production, microvacular occlusions from enhanced platelet adhesiveness, or increase in fibrinogen and clotting factors. Ocular Side Effects • Microvascular complications like artery and venous occlusions • Dry Eye • Contact Lens Intolerance • Optic neuritis • Macular Edema • TIA (Transischemic attacks) • Pseudotumor cerebri
- 53. RARE OCULAR SIDE EFFECTS Conjunctivitis: 1. Antianxiety (diazepam; alprazolam) 2. Phenytoin; carbamazepine Extraocular muscle paresis: 1. Sufonylureas- glipizide, glyburide. 2. Barbiturate 3. Oculomotor nerve palsy- interferon alpha Visual sensation: • Digitalis
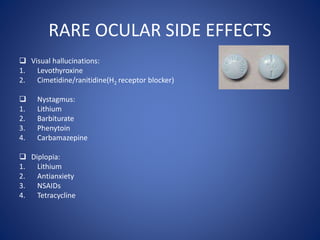
- 54. RARE OCULAR SIDE EFFECTS Visual hallucinations: 1. Levothyroxine 2. Cimetidine/ranitidine(H2 receptor blocker) Nystagmus: 1. Lithium 2. Barbiturate 3. Phenytoin 4. Carbamazepine Diplopia: 1. Lithium 2. Antianxiety 3. NSAIDs 4. Tetracycline
- 55. RARE OCULAR SIDE EFFECTS Eyelid hyperemia: 1. Levothyroxine. Ptosis: 1. Barbiturate 2. Chloroquine Visual field changes: 1. Vigabatrin 2. Paracentral scotoma: Chloroquine Pseudotumor cerebri: 1. Amiodarone 2. Levothyroxine 3. OCPs 4. NSAIDs 5. Isotretinoin 6. Tetracycline.
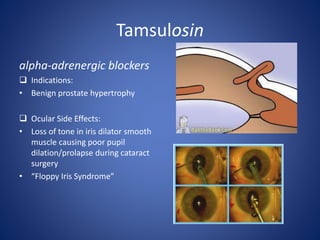
- 56. Tamsulosin alpha-adrenergic blockers Indications: • Benign prostate hypertrophy Ocular Side Effects: • Loss of tone in iris dilator smooth muscle causing poor pupil dilation/prolapse during cataract surgery • “Floppy Iris Syndrome”
- 57. SILDENAFIL inhibits phosophodiesterase-5 (PDE-5) which results in vasodilation of smooth muscle. Ocular Side Effects • Objects have color tinges—usually blue or blue- green, may be pink or yellow • 11% of patients on 100mg perceive a blue haze up to four hours • Dark colors appear darker • Visual disturbances
- 58. SILDENAFIL • The above ocular side effects are dose-dependent . – For sildenafil side effects occur at the following incidences: – 50mg 3% – 100mg 10% – 200mg 40-50% • The side effects based on dosage with sildenafil start 15-30 minutes after ingestion of the drug, and usually peak 60 minutes after ingestion.
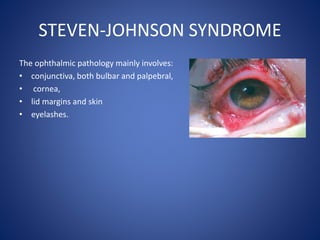
- 59. STEVEN-JOHNSON SYNDROME • Immune complex mediated hypersensitivity reaction • Involves skin and mucosa Pathophysiology: • SJS involves massive apoptosis of keratinocytes within epidermis. • Intermediate drug metabolites initiate an immune response in susceptible individuals- increase in release of Fas-ligand- binds to and activates Fas, which is a keratinocyte cell surface receptor that initiates apoptosis. • In large retrospective studies, Power et al and Chang et al reported ocular involvement in 69% and 81%, respectively, of patients with SJS.
- 60. STEVEN-JOHNSON SYNDROME The ophthalmic pathology mainly involves: • conjunctiva, both bulbar and palpebral, • cornea, • lid margins and skin • eyelashes.
- 61. STEVEN-JOHNSON SYNDROME Conjunctiva: • Mild cases- conjunctivitis- minimal ocular discomfort and photophobia. • Severe cases- pseudomembranous and membranous conjunctivitis. Discomfort and photophobia more pronounced. • The raw surfaces can lead to adhesion formation between the palpebral and bulbar conjunctiva, known as symblepharon.
- 62. STEVEN-JOHNSON SYNDROME Eyelids: • Contracture of the palpebral conjunctiva can yield cicatricial entropion. • Lid margin inflammation can cause widespread destruction of meibomian gland orifices and the glands themselves. • Eyelash architecture can also be affected, resulting in trichiasis and distichiasis. • Keratinization of the lid margins and palpebral conjunctiva further contributes to discomfort and corneal damage via blink-related microtrauma to the corneal epithelium.
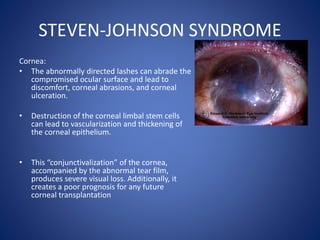
- 63. STEVEN-JOHNSON SYNDROME Cornea: • The abnormally directed lashes can abrade the compromised ocular surface and lead to discomfort, corneal abrasions, and corneal ulceration. • Destruction of the corneal limbal stem cells can lead to vascularization and thickening of the corneal epithelium. • This “conjunctivalization” of the cornea, accompanied by the abnormal tear film, produces severe visual loss. Additionally, it creates a poor prognosis for any future corneal transplantation
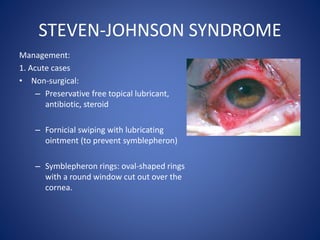
- 64. STEVEN-JOHNSON SYNDROME Management: 1. Acute cases • Non-surgical: – Preservative free topical lubricant, antibiotic, steroid – Fornicial swiping with lubricating ointment (to prevent symblepheron) – Symblepheron rings: oval-shaped rings with a round window cut out over the cornea.
- 65. STEVEN JOHNSON SYNDROME • Surgical: Amniotic membrane: minimize the destructive inflammation during the acute phase of SJS Indication- – membranous conjunctivitis, early symblepharon formation, and intense lid margin inflammation with lash loss
- 66. SUMMARY A careful and detailed case history is important to reveal a patient’s medication history The ocular and visual side effects from a patient’s systemic medication can range from mild to severe. These side effects may or may not be serious enough to warrant discontinuing treatment. Recognition of ocular and visual side effects is important for prompt management to prevent and minimize serious complications Familiarity with medications improves by routinely paying attention to concomitant medications.