Respiratory System - Physiology
- 2. Respiratory System Functions 1. Supplies the body with oxygen and disposes of carbon dioxide 2. Filters inspired air 3. Produces sound 4. Clears the body from excess water and heat 5. Control blood pH
- 3. • Primary function is to obtain oxygen for use by body's cells & eliminate carbon dioxide that cells produce
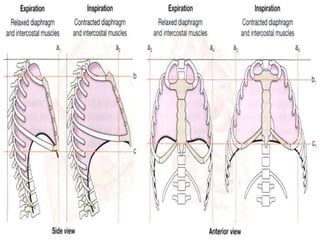
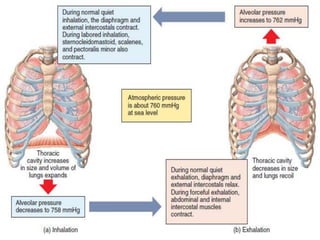
- 4. Breathing • Breathing (pulmonary ventilation). consists of two cyclic phases: • Inhalation, also called inspiration - draws gases into the lungs. • Exhalation, also called expiration - forces gases out of the lungs.
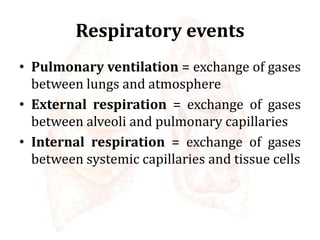
- 5. Respiratory events • Pulmonary ventilation = exchange of gases between lungs and atmosphere • External respiration = exchange of gases between alveoli and pulmonary capillaries • Internal respiration = exchange of gases between systemic capillaries and tissue cells
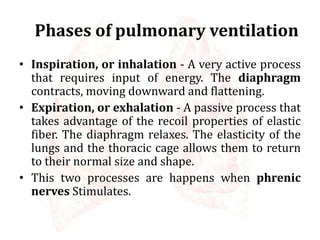
- 7. Phases of pulmonary ventilation • Inspiration, or inhalation - A very active process that requires input of energy. The diaphragm contracts, moving downward and flattening. • Expiration, or exhalation - A passive process that takes advantage of the recoil properties of elastic fiber. The diaphragm relaxes. The elasticity of the lungs and the thoracic cage allows them to return to their normal size and shape. • This two processes are happens when phrenic nerves Stimulates.
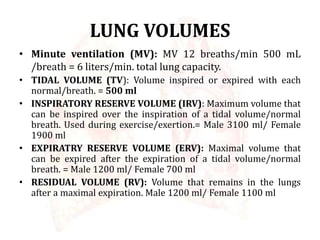
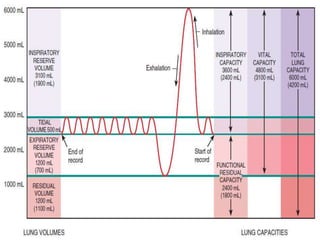
- 8. LUNG VOLUMES • Minute ventilation (MV): MV 12 breaths/min 500 mL /breath = 6 liters/min. total lung capacity. • TIDAL VOLUME (TV): Volume inspired or expired with each normal/breath. = 500 ml • INSPIRATORY RESERVE VOLUME (IRV): Maximum volume that can be inspired over the inspiration of a tidal volume/normal breath. Used during exercise/exertion.= Male 3100 ml/ Female 1900 ml • EXPIRATRY RESERVE VOLUME (ERV): Maximal volume that can be expired after the expiration of a tidal volume/normal breath. = Male 1200 ml/ Female 700 ml • RESIDUAL VOLUME (RV): Volume that remains in the lungs after a maximal expiration. Male 1200 ml/ Female 1100 ml
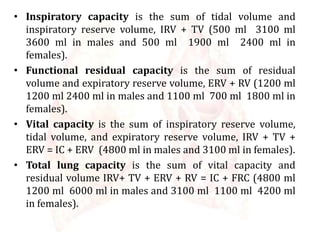
- 9. • Inspiratory capacity is the sum of tidal volume and inspiratory reserve volume, IRV + TV (500 ml 3100 ml 3600 ml in males and 500 ml 1900 ml 2400 ml in females). • Functional residual capacity is the sum of residual volume and expiratory reserve volume, ERV + RV (1200 ml 1200 ml 2400 ml in males and 1100 ml 700 ml 1800 ml in females). • Vital capacity is the sum of inspiratory reserve volume, tidal volume, and expiratory reserve volume, IRV + TV + ERV = IC + ERV (4800 ml in males and 3100 ml in females). • Total lung capacity is the sum of vital capacity and residual volume IRV+ TV + ERV + RV = IC + FRC (4800 ml 1200 ml 6000 ml in males and 3100 ml 1100 ml 4200 ml in females).
- 11. Physiology of respiration The process of gas exchange in the body, called respiration, it has three basic steps: 1. Pulmonary ventilation or breathing – It is the inhalation (inflow) and exhalation (outflow) of air and involves the exchange of air between the atmosphere and the alveoli of the lungs. 2. External (pulmonary) respiration – It is the exchange of gases between the alveoli of the lungs and the blood in pulmonary capillaries across the respiratory membrane. – In this process, pulmonary capillary blood gains O2 and loses CO2. 3. Internal (tissue) respiration – It is the exchange of gases between blood in systemic capillaries and tissue cells. In this step the blood loses O2 and gains CO2. Within cells, the metabolic reactions that consume O2 and give off CO2 during the production of ATP are termed cellular respiration
- 12. Inhalation • Breathing in is called inhalation (inspiration) • Each inhalation, the air pressure inside the lungs is equal to the air pressure of the atmosphere, which is about 760 mmHg. • Air to flow into the lungs, the pressure inside the alveoli must become lower than the atmospheric pressure. • This condition is achieved by increasing the size of the lungs.
- 13. Exhalation Breathing out or exhalation starts when the inspiratory muscles relax. As the diaphragm relaxes, its dome moves superiorly owing to its elasticity. As the external intercostals relax, the ribs are depressed. • The pressure in the lungs is greater than the pressure of the atmosphere. Normal exhalation during quiet breathing • It is a passive process because no muscular contractions are involved. Instead, exhalation results from elastic recoil of the chest wall and lungs, both of which have a natural tendency to spring back after they have been stretched. • Two inwardly directed forces contribute to elastic recoil: a. The recoil of elastic fibers that were stretched during inhalation b. The inward pull of surface tension due to the film of alveolar fluid.
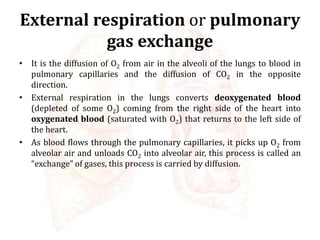
- 15. External respiration or pulmonary gas exchange • It is the diffusion of O2 from air in the alveoli of the lungs to blood in pulmonary capillaries and the diffusion of CO2 in the opposite direction. • External respiration in the lungs converts deoxygenated blood (depleted of some O2) coming from the right side of the heart into oxygenated blood (saturated with O2) that returns to the left side of the heart. • As blood flows through the pulmonary capillaries, it picks up O2 from alveolar air and unloads CO2 into alveolar air, this process is called an “exchange” of gases, this process is carried by diffusion.
- 16. Internal respiration The left ventricle pumps oxygenated blood into the aorta and through the systemic arteries to systemic capillaries. The exchange of O2 and CO2 between systemic capillaries and tissue cells is called internal respiration or systemic gas exchange
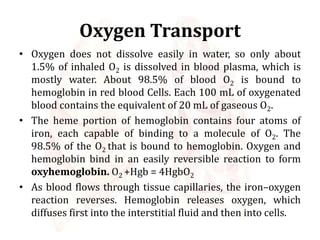
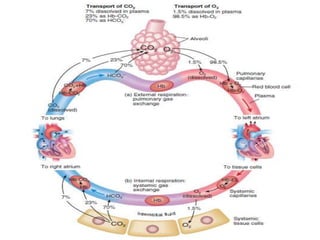
- 17. Oxygen Transport • Oxygen does not dissolve easily in water, so only about 1.5% of inhaled O2 is dissolved in blood plasma, which is mostly water. About 98.5% of blood O2 is bound to hemoglobin in red blood Cells. Each 100 mL of oxygenated blood contains the equivalent of 20 mL of gaseous O2. • The heme portion of hemoglobin contains four atoms of iron, each capable of binding to a molecule of O2. The 98.5% of the O2 that is bound to hemoglobin. Oxygen and hemoglobin bind in an easily reversible reaction to form oxyhemoglobin. O2 +Hgb = 4HgbO2 • As blood flows through tissue capillaries, the iron–oxygen reaction reverses. Hemoglobin releases oxygen, which diffuses first into the interstitial fluid and then into cells.
- 18. Factors Affecting the Affinity of Hemoglobin for Oxygen • Although PO2 is the most important factor that determines the percent O2 saturation of hemoglobin. The following four factors affect the affinity of hemoglobin for O2 : 1. Acidity (pH). 2. Partial pressure of carbon dioxide 3. Temperature. 4. 2,3-bisphosphoglycerate (BPG)
- 19. Acidity • As acidity increases (pH decreases), the affinity of hemoglobin for O2 decreases, and O2 dissociates more readily from hemoglobin. • When H+ ions bind to amino acids in hemoglobin, they alter its structure slightly, decreasing its oxygen-carrying capacity. Thus, lowered pH drives O2 off hemoglobin, making more O2 available for tissue cells.
- 20. Oxygen–hemoglobin dissociation curves showing the relationship of pH
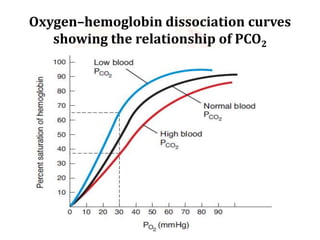
- 21. Partial pressure of carbon dioxide • CO2 enters the blood it is temporarily converted to carbonic acid (H2CO3). • It dissociates and form hydrogen ions and bicarbonate ions. So in red blood cells the H+ concentration increases, pH decreases. Thus, an increased PCO2 produces a more acidic environment, which helps release O2 from hemoglobin.
- 22. Oxygen–hemoglobin dissociation curves showing the relationship of PCO2
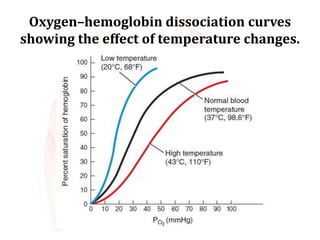
- 23. Temperature • Heat is a by-product of the metabolic reactions of all cells, and the heat released by contracting muscle fibers tends to raise body temperature. Metabolically active cells require more O2 and liberate more acids and heat.
- 24. Oxygen–hemoglobin dissociation curves showing the effect of temperature changes.
- 25. 2,3-bisphosphoglycerate (BPG) (Diphosphoglycerate) • BPG is formed in red blood cells when they break down glucose to produce ATP in a process called glycolysis. When BPG combines with hemoglobin, it unloads or decreases the bonding with oxygen.
- 26. CO2 Transportation • Normal resting conditions, each 100 mL of deoxygenated blood contains the equivalent of 53 mL of gaseous CO2, which is transported in the blood in three main forms 1. Dissolved CO2. The smallest percentage— about 7%—is dissolved in blood plasma. On reaching the lungs, it diffuses into alveolar air and is exhaled.
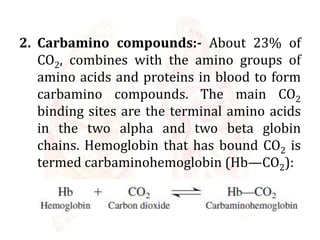
- 27. 2. Carbamino compounds:- About 23% of CO2, combines with the amino groups of amino acids and proteins in blood to form carbamino compounds. The main CO2 binding sites are the terminal amino acids in the two alpha and two beta globin chains. Hemoglobin that has bound CO2 is termed carbaminohemoglobin (Hb—CO2):
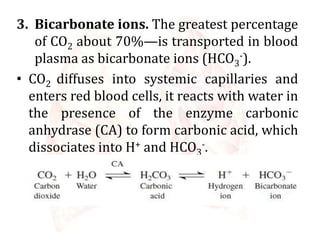
- 28. 3. Bicarbonate ions. The greatest percentage of CO2 about 70%—is transported in blood plasma as bicarbonate ions (HCO3 -). • CO2 diffuses into systemic capillaries and enters red blood cells, it reacts with water in the presence of the enzyme carbonic anhydrase (CA) to form carbonic acid, which dissociates into H+ and HCO3 -.
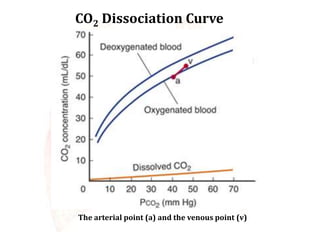
- 29. CO2 Dissociation Curve The arterial point (a) and the venous point (v)
- 31. Regulation of respiration • Regulation of respiration control is the rate and depth of respiration as per the physiologic demand. Control of respiration primarily involves neurons in the reticular formation of the medulla and pons. Because the medulla sets the respiratory rhythm. The purpose of Regulation of respiration are 1. To maintain a constant O2 and CO2 level in blood 2. It adjust the O2 supply as per the metabolic demand of the body. 3. It helps to regulate acid base balance or pH.
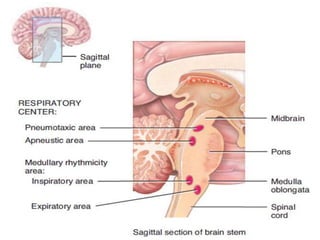
- 32. • The size of the thorax is altered by the action of the respiratory muscles, which contract as a result of nerve impulses transmitted to them from centers in the brain and relax in the absence of nerve impulses. This impulses travels along the phrenic and intercostal nerves to excite the diaphragm and external intercostal muscles • These nerve impulses are sent from clusters of neurons located bilaterally in the medulla oblongata and pons of the brainstem. • This widely dispersed group of neurons, collectively called the respiratory center.
- 33. Mechanism of Regulation of respiration • There are two major mechanisms 1. Nervous regulation of respiration 2. Chemical regulation of respiration
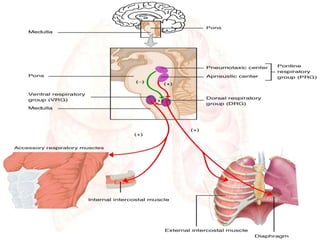
- 34. 1. Nervous regulation of respiration Respiratory Center The respiratory centers are divided into four major groups, two groups in the medulla and two in the pons. The two groups in the medulla are a. The dorsal respiratory group b. The ventral respiratory group. The two groups in the pons are the pneumotaxic center and the apneustic center also known as the pontine respiratory group.
- 36. • Respiratory centers can be divided into three areas on the basis of their functions: 1. The medullary rhythmicity area in the medulla oblongata 2. The pneumotaxic area in the pons 3. The apneustic area, also in the pons
- 38. Medullary Rhythmicity Area • The function of the medullary rhythmicity area is to control the basic rhythm of respiration. It includes two areas a. Inspiratory medullary rhythmicity area or inspiratory centre b. Expiratory medullary rhythmicity area or expiratory centre
- 39. a. Inspiratory centre: It establish the basic rhythm of breathing. When its inspiratory neurons fire, a burst of impulses travels along the phrenic and intercostal nerves to excite the diaphragm and external intercostal muscles. b. Expiratory centre: Impulses from the expiratory area cause contraction of the internal intercostal and abdominal muscles, which decreases the size of the thoracic cavity and causes forceful exhalation.
- 40. Pneumotaxic Area • It transmits inhibitory impulses to the inspiratory area. The major effect of these nerve impulses is to help turn off the inspiratory area before the lungs become too full of air.
- 41. Apneustic area • This area sends stimulatory impulses to the inspiratory area that activate it and prolong inhalation. The result is a long, deep inhalation.
- 42. 2. Chemical regulation of respiration • There are three important chemical factors controlling respiration 1. Concentration of CO2 in blood 2. Concentration of H+ ions or pH 3. Concentration of oxygen In blood
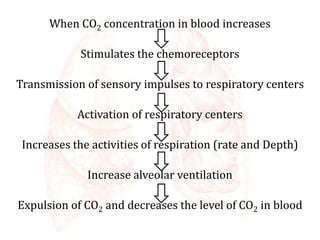
- 43. Concentration of CO2 in blood • When CO2 concentration in blood increases, it stimulates the chemoreceptors. There are two group of chemoreceptors 1. Peripheral chemoreceptors – situated at the carotid body and aortic body 2. Central chemoreceptors – situated at the medulla oblongata
- 44. When CO2 concentration in blood increases Stimulates the chemoreceptors Transmission of sensory impulses to respiratory centers Activation of respiratory centers Increases the activities of respiration (rate and Depth) Increase alveolar ventilation Expulsion of CO2 and decreases the level of CO2 in blood
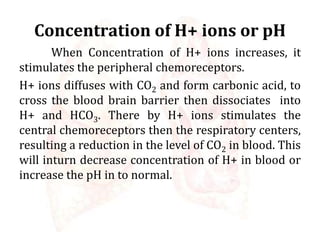
- 45. Concentration of H+ ions or pH When Concentration of H+ ions increases, it stimulates the peripheral chemoreceptors. H+ ions diffuses with CO2 and form carbonic acid, to cross the blood brain barrier then dissociates into H+ and HCO3. There by H+ ions stimulates the central chemoreceptors then the respiratory centers, resulting a reduction in the level of CO2 in blood. This will inturn decrease concentration of H+ in blood or increase the pH in to normal.
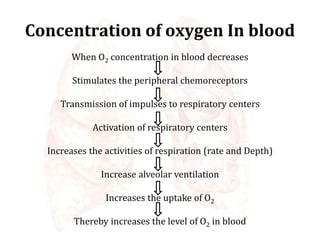
- 46. Concentration of oxygen In blood When O2 concentration in blood decreases Stimulates the peripheral chemoreceptors Transmission of impulses to respiratory centers Activation of respiratory centers Increases the activities of respiration (rate and Depth) Increase alveolar ventilation Increases the uptake of O2 Thereby increases the level of O2 in blood
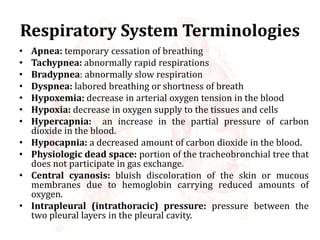
- 47. Respiratory System Terminologies • Apnea: temporary cessation of breathing • Tachypnea: abnormally rapid respirations • Bradypnea: abnormally slow respiration • Dyspnea: labored breathing or shortness of breath • Hypoxemia: decrease in arterial oxygen tension in the blood • Hypoxia: decrease in oxygen supply to the tissues and cells • Hypercapnia: an increase in the partial pressure of carbon dioxide in the blood. • Hypocapnia: a decreased amount of carbon dioxide in the blood. • Physiologic dead space: portion of the tracheobronchial tree that does not participate in gas exchange. • Central cyanosis: bluish discoloration of the skin or mucous membranes due to hemoglobin carrying reduced amounts of oxygen. • Intrapleural (intrathoracic) pressure: pressure between the two pleural layers in the pleural cavity.
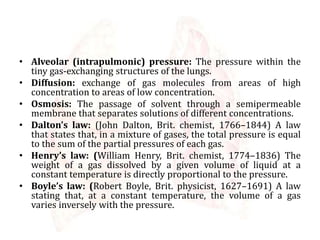
- 48. • Alveolar (intrapulmonic) pressure: The pressure within the tiny gas-exchanging structures of the lungs. • Diffusion: exchange of gas molecules from areas of high concentration to areas of low concentration. • Osmosis: The passage of solvent through a semipermeable membrane that separates solutions of different concentrations. • Dalton’s law: (John Dalton, Brit. chemist, 1766–1844) A law that states that, in a mixture of gases, the total pressure is equal to the sum of the partial pressures of each gas. • Henry’s law: (William Henry, Brit. chemist, 1774–1836) The weight of a gas dissolved by a given volume of liquid at a constant temperature is directly proportional to the pressure. • Boyle’s law: (Robert Boyle, Brit. physicist, 1627–1691) A law stating that, at a constant temperature, the volume of a gas varies inversely with the pressure.
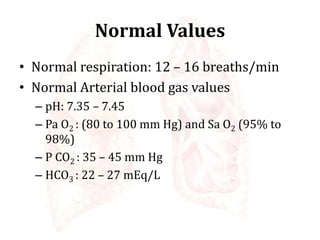
- 49. Normal Values • Normal respiration: 12 – 16 breaths/min • Normal Arterial blood gas values – pH: 7.35 – 7.45 – Pa O2 : (80 to 100 mm Hg) and Sa O2 (95% to 98%) – P CO2 : 35 – 45 mm Hg – HCO3 : 22 – 27 mEq/L