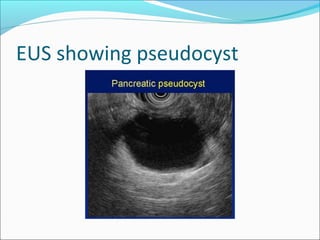
Pancreatic pseudocyst
- 1. Dr. Abrar Ahmad Post graduate resident Surgical unit 1 BVH Bahawalpur
- 2. Pancreatic Pseudocyst A fluid collection contained within a well-defined capsule of fibrous or granulation tissue or a combination of both Does not possess an epithelial lining Persists > 4 weeks May develop in the setting of acute or chronic pancreatitis Bradley III et al. A clinically based classification system for acute pancreatitis: summary of the International Symposium on Acute Pancreatitis, Arch Surg. 1993;128:586-590
- 3. Pancreatic Pseudocyst Most common cystic lesions of the pancreas, accounting for 75-80% of such masses Location Lesser peritoneal sac in proximity to the pancreas Large pseudocysts can extend into the paracolic gutters, pelvis, mediastinum, neck or scrotum May be loculated
- 4. Composition Thick fibrous capsule – not a true epithelial lining Pseudocyst fluid Similar electrolyte concentrations to plasma High concentration of amylase, lipase, and enterokinases such as trypsin
- 5. Pathophysiology Pancreatic ductal disruption 2° to 1. Acute pancreatitis – Necrosis 2. Chronic pancreatitis – Elevated pancreatic duct pressures from strictures or ductal calculi 3. Trauma 4. Ductal obstruction and pancreatic neoplasms
- 6. Pathophysiology Acute Pancreatitis Pancreatic necrosis causes ductular disruption, resulting in leakage of pancreatic juice from inflamed area of gland, accumulates in space adjacent to pancreas Inflammatory response induces formation of distinct cyst wall composed of granulation tissue, organizes with connective tissue and fibrosis
- 7. Pathophysiology Chronic Pancreatitis Pancreatic duct chronically obstructed ongoing proximal pancreatic secretion leads to secular dilation of duct – true retention cyst Formed micro cysts can eventually coalesce and lose epithelial lining as enlarge
- 8. Presentation Symptoms Abdominal pain > 3 weeks (80 – 90%) Nausea / vomiting Early satiety Bloating, indigestion Signs Tenderness Abdominal fullness Cohen et al: Pancreatic pseudocyst. In: Cameron JL, ed. Current Surgical Therapy. 7th ed.; 2001: 543-7
- 9. Diagnosis Clinically suspect a pseudocyst Episode of pancreatitis fails to resolve Amylase levels persistantly high Persistant abdominal pain Epigastric mass palpated after pancreatitis
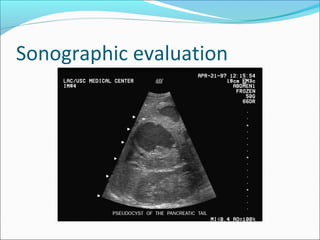
- 10. Diagnosis Labs Persistently elevated serum amylase Plain X-ray Not very useful Ultrasound 75 -90% sensitive CT Most accurate (sensitivity 90-100%)
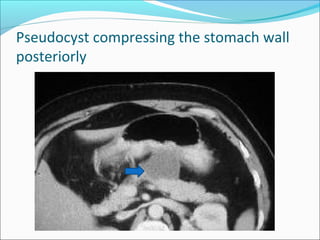
- 11. Pseudocyst compressing the stomach wall posteriorly
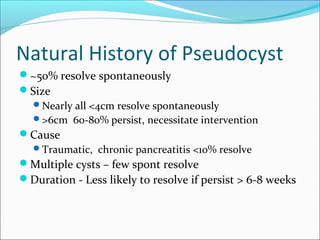
- 14. Natural History of Pseudocyst ~50% resolve spontaneously Size Nearly all <4cm resolve spontaneously >6cm 60-80% persist, necessitate intervention Cause Traumatic, chronic pancreatitis <10% resolve Multiple cysts – few spont resolve Duration - Less likely to resolve if persist > 6-8 weeks
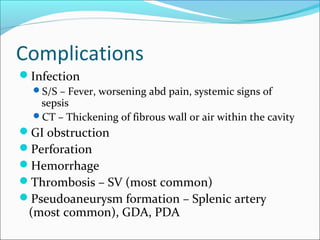
- 15. Complications Infection S/S – Fever, worsening abd pain, systemic signs of sepsis CT – Thickening of fibrous wall or air within the cavity GI obstruction Perforation Hemorrhage Thrombosis – SV (most common) Pseudoaneurysm formation – Splenic artery (most common), GDA, PDA
- 16. Treatment Initial NPO TPN Octreotide Antibiotics if infected 1/3 – 1/2 resolve spontaneously
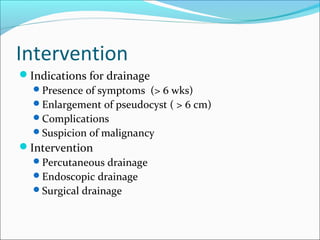
- 17. Intervention Indications for drainage Presence of symptoms (> 6 wks) Enlargement of pseudocyst ( > 6 cm) Complications Suspicion of malignancy Intervention Percutaneous drainage Endoscopic drainage Surgical drainage
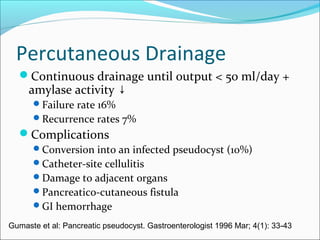
- 18. Percutaneous Drainage Continuous drainage until output < 50 ml/day + amylase activity ↓ Failure rate 16% Recurrence rates 7% Complications Conversion into an infected pseudocyst (10%) Catheter-site cellulitis Damage to adjacent organs Pancreatico-cutaneous fistula GI hemorrhage Gumaste et al: Pancreatic pseudocyst. Gastroenterologist 1996 Mar; 4(1): 33-43
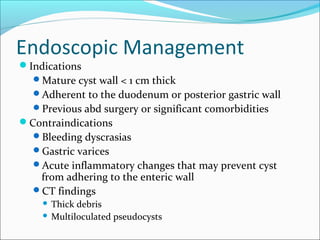
- 19. Endoscopic Management Indications Mature cyst wall < 1 cm thick Adherent to the duodenum or posterior gastric wall Previous abd surgery or significant comorbidities Contraindications Bleeding dyscrasias Gastric varices Acute inflammatory changes that may prevent cyst from adhering to the enteric wall CT findings Thick debris Multiloculated pseudocysts
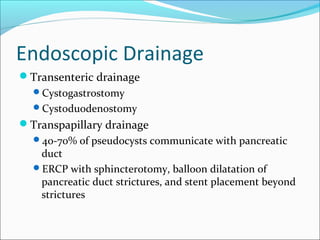
- 20. Endoscopic Drainage Transenteric drainage Cystogastrostomy Cystoduodenostomy Transpapillary drainage 40-70% of pseudocysts communicate with pancreatic duct ERCP with sphincterotomy, balloon dilatation of pancreatic duct strictures, and stent placement beyond strictures
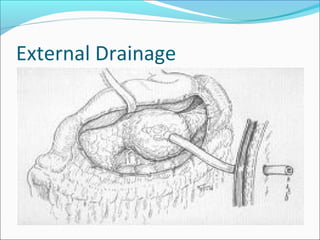
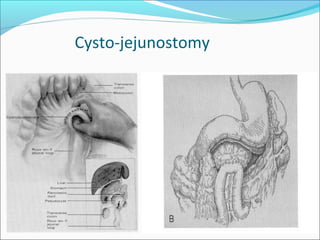
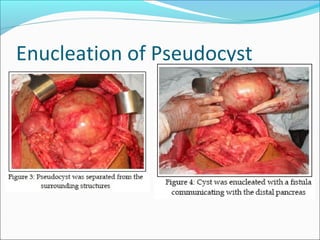
- 21. Surgical Options Excision Tail of gland & along with proximal strictures – distal pancreatectomy & splenectomy Head of gland with strictures of pancreatic or bile ducts – pancreaticoduodenectomy External drainage Internal drainage Cystogastrostomy Cystojejunostomy Permanent resolution confirmed in b/w 91%–97% of patients* Cystoduodenostomy Can be complicated by duodenal fistula and bleeding at anastomotic site
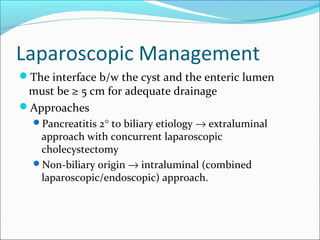
- 25. Laparoscopic Management The interface b/w the cyst and the enteric lumen must be ≥ 5 cm for adequate drainage Approaches Pancreatitis 2° to biliary etiology → extraluminal approach with concurrent laparoscopic cholecystectomy Non-biliary origin → intraluminal (combined laparoscopic/endoscopic) approach.
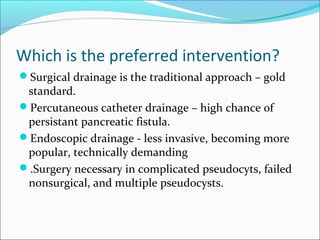
- 26. Which is the preferred intervention? Surgical drainage is the traditional approach – gold standard. Percutaneous catheter drainage – high chance of persistant pancreatic fistula. Endoscopic drainage - less invasive, becoming more popular, technically demanding .Surgery necessary in complicated pseudocyts, failed nonsurgical, and multiple pseudocysts.
- 27. THANKS