Peptic ulcer drugs and pharmcotherapy - drdhriti
- 1. Pharmacotherapy of Peptic Ulcer Dr. D. K. Brahma Department of Pharmacology NEIGRIHMS, SHILLONG MEGHALAYA
- 2. Contents • Physiology of Gastric acid secretion • An introduction to Peptic Ulcer Disease • An outline on the Drugs used in such disorders • Pharmacokinetics and Pharmacodynamics of important groups of Drugs • Clinical pharmacology of Peptic Ulcer Disease
- 3. Phases of gastric secretion Phase Stimuli Pathway Cephalic (stimulate) Sight, smell, taste or thought of food 1) Vagus (M3 receptors) 2) Histamine (H2 receptor) 3) Gastrin Gastric (stimulate) Food in the stomach 1) Stretch: local reflex (M3 receptors) 2) Chemical substances in food (gastrin) 3) Increase pH: Inhibition of somatostatin (GHIH) release Intestinal (inhibit) Chyme in the duodenum
- 4. Physiology of Gastric Secretion Vagus Food GC CNS •H2 – cAMP •M3 & CCK2 – IP3-DAG
- 5. What is Peptic Ulcer ? • A peptic ulcer disease or PUD is an ulcer (defined as mucosal erosions equal to or greater than 0.5 cm) of an area of the gastrointestinal tract exposed to the acid and pepsin secretion • Gastritis is the precursor to PUD and it is clinically difficult to differentiate the two – Stomach (called gastric ulcer) – Duodenum (called duodenal ulcer) – Esophagus (called Esophageal ulcer) – Meckel's Diverticulum (called Meckel's Diverticulum ulcer)
- 6. Duodenal Vs Gastric Ulcers Duodenal • Age: 25-75 years • Gnawing or burning upper abdomen pain relieved by food but reappears 1-3 hrs after meals • Worsening pain when stomach empty • Bleeding occurs with deep erosion – Haematemesis – Maelena Gastric • Age: 55-65 years • Relieved by food but pain may persist even after eating • Anorexia, wt loss, vomiting • Infrequent or absent remissions • Small % become cancerous • Severe ulcers may erode through stomach wall
- 7. Gastroesophageal Reflux Disease (GERD) • Common and is a GIT motility disorder • Acidity of Gastric contents – most common factor • Acid contents reflux back into esophagus • Intense burning, sometimes belching • Can lead to esophagitis, esophageal ulcers, and strictures – Barrett’s esophagus • Commonly associated with obesity • Improves with lifestyle management
- 8. Why Ulceration Occurs? • High pH (2 to 3) in the gastric lumen – Pepsin is active • Require defense mechanisms to protect oesophagus and stomach Oesophagus – protected by LES – Stomach: a number of mechanisms • Mucus secretion • Prostaglandins: I2 and E2 (alcohol, aspirin, and other drugs) • Bicabonate ions • High Blood Flow (nitric oxide mediated)
- 10. Because of Imbalance • Imbalance primarily between Aggressive factors and Defensive factors: Aggressive factors, e,g, acid, pepsin, bile etc. Defensive factors, e.g. mucus, HCO3, PG
- 11. What may contribute imbalance ? • Helicobacter pylori • NSAIDs • Ethanol • Tobacco • Severe physiologic stress (Burns, CNS trauma, Surgery, Severe medical illness) • Steroids
- 12. H. pylori • Gram (-) rod with flagella • H pylori is most common cause of PUD • Transmission route fecal-oral • Secretes urease → convert urea to ammonia • Produces alkaline environment enabling survival in stomach • Almost all duodenal and 2/3 gastric ulcer pt’s infected with HP • Considered class 1 carcinogen → gastric cancer • Higher prevalence in Low SES
- 13. Who are they ? Barry J Marshall J. Robin Warren Nobel Laureates of Medicine – 2005 Discovery of H. pylori & its role in peptic ulcer
- 14. NSAIDS Damage to the cytoprotective role of PGs – PGE2 and PGI2
- 15. Differentiating between H. pylori and NSAID-induced ulcer Ulcers associated with H. pylori • More often in duodenum • Often superficial • Less severe GI bleeding Ulcers associated with NSAIDs • More often in stomach • Often deep • More severe GI bleeding • Sometimes asymptomatic
- 16. Therapy Purpose Therapy is directed at enhancing host defense or eliminating aggressive factors; i.e., H. pylori Peptic Ulcers
- 17. Classification 1. Acid Neutralizing agents: (ANTACIDS) • Systemic: Sodium Bicarbonate and Sod. Citrate • Nonsystemic: Magnesium hydroxide, Mag. Treisilicate, Aluminium hydroxide gel, Magaldrate and calcium carbonate 1. Reduction in Gastric acid secretion: • H2 antihistamines: Cimetidine, Ranitidine, Famotidine, Nizatidine and Roxatidine • Proton pump inhibitors: Omeprazole, Lansoprazole Pantoprazole, Rabeprazole and Esomeprazole • Anticholinergics: Pirenzepine, Propantheline and Oxyphenonium • Prostaglandin analogue: Misoprostol
- 18. Classification – contd. 3. Ulcer protectives: Sucralfate, Colloidal Bismuth sudcitrate 4. Anti-H. pylori Drugs: Amoxicillin, Clarithromycin, metronidazole, tinidazole and tetracycline
- 19. Antacids • Weak bases that neutralize acid • Also inhibit formation of pepsin (As pepsinogen converted to pepsin at acidic pH) • Acid Neutralizing Capacity: – Potency of Antacids – Expressed in terms of Number of mEq of 1N HCl that are brought down to pH 3.5 in 15 minutes by unit dose of a preparation (1 gm)
- 20. Antacids - The Oldest Remedy • Sodium Bicarbonate: – Potent neutralizing capacity and acts instantly – ANC: 1 gm = 12 mEq • NOT USED ANYMORE FOR ITS DEMERITS: – Systemic alkalosis – Distension, discomfort and belching – CO2 – Rebound acidity – Sodium overload
- 21. Antacids • Present day antacids : – Aluminium Hydroxide (ANC 1-2.5mEq/g) – Magnesium Hydroxide (ANC 30 mEq) – milk of magnesia – Magnesium trisilicate (ANC 1mEq/g) • Duration of action : 30 min when taken in empty stomach and 2 hrs when taken after a meal • Side effects : – Aluminium antacids – constipation (As they relax gastric smooth muscle & delay gastric emptying) – also hypophosphatemia and osteomalcia – Mg2+ antacids – Osmotic diarrhoea • In renal failure Al3+ antacid – Aluminium toxicity & Encephalopathy (Magaldrate – hydrated hydroxy magnesium aluminate)
- 22. Antacids – contd. • Simethicone: Decrease surface tension thereby reduce bubble formation - added to prevent reflux • Alginates: Form a layer of foam on top of gastric contents & reduce reflux • Oxethazaine: Surface anaesthetic
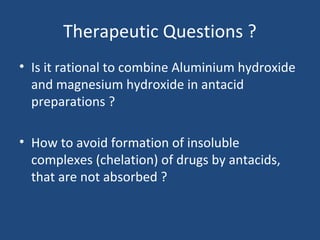
- 23. Therapeutic Questions ? • Is it rational to combine Aluminium hydroxide and magnesium hydroxide in antacid preparations ? • How to avoid formation of insoluble complexes (chelation) of drugs by antacids, that are not absorbed ?
- 24. Answers (!) • Interactions can be avoided by taking antacids 2 hrs before or after ingestion of other drugs • Combination provides a relatively fast and sustained neutralizing capacity – (Magnesium Hydroxide – Rapidly acting – Aluminium Hydroxide - Slowly acting ) • Combination preserves normal bowel function – (Aluminium Hydroxide – constipation – Magnesium hydroxide – diarrhoea )
- 25. The Reality • Not part of Physician prescribed regimen – frequency of dosing and rebound acidity (Gastrin secretion) • Over the counter (OTC) drug for symptomatic relief of dyspepsia • May only be prescribed for very short term: – Non-ulcer dyspepsia and minor episodes of heart burn – As adjuvant in GERD – quick relieve
- 26. Sucralfate – ulcer protective • Salt of sucrose complexed to sulfated aluminium hydroxide (basic aluminium salt) • MOA: – In acidic pH polymerises to viscous gel that adheres to ulcer crater - more on duodenal ulcer – Precipitates protein on surface proteins and acts as physical barrier – Dietary proteins get deposited on this layer forming another coat – Delays gastric emptying and causes gastric PG synthesis – protective action
- 27. Sucralfate – contd. • Taken on empty stomach 1 hr. before meals • Concurrent antacids, H2 antagonist avoided (as it needs acid for activation) • Uses: – NSAID induced ulcers – Patients with continued smoking – ICU – Topically – burn, bedsore ulcers, excoriated skins • Dose: 1 gm 1 Hr before meals • ADRs: Constipation, hypophosphatemia
- 28. Chemical reactions of antacids with HCl in the stomach
- 29. Antacids Capsules & Tablets: • Powders • Chewable tablets • Suspensions • Effervescent granules and tablets
- 30. H2 Antagonists • Cimetidine, Ranitidine, Famotidine, Roxatidine, Nizatidine and • MOA: – Reversible competitive inhibitors of H2 receptor – Highly selective, no action on H1 or H3 receptors – All phases of gastric acid secretion – Very effective in inhibiting nocturnal acid secretion (as it depends largely on Histamine ) – Modest impact on meal stimulated acid secretion (as it depends on gastrin, acetylcholine and histamine) – Volume of pepsin content and IF are also reduced – Volume reduced by 60 – 70% - anti ulcerogenic effect – No effect on motility
- 31. H2 antagonists • Kinetics: – All drugs are absorbed orally adequately – Bioavailability upto 80 % – Absorption is not interfered by presence of food – Can cross placental barrier and reaches milk – Poor CNS penetration – 2/3rd of the drugs are excreted unchanged in bile and urine • Preparations: available as tablets, injections
- 32. H2 antagonists - ADRs • Extremely safe drugs and well tolerated • Main ADRs are related to Cimetidine: – Antiandrogenic effects – Increases prolactin secretion and inhibits degradation of estradiol by liver – Cytochrome P450 inhibition – theophylline, metronidazole, phenytoin, imipramine etc. – Antacids • Others: – Headache, dizziness, bowel upset, dry mouth – Bolus IV – release histamine – bradycardia, arrhythmia, cardiac arrest – Elderly - precaution
- 33. Bioavailability 80 50 40 >90 Relative Potency 1 5 -10 32 5 -10 Half life (hrs) 1.5 - 2.3 1.6 - 2.4 2.5 - 4 1.1 -1.6 Duration of 6 8 12 8 action (hrs) Inhibition of 1 0.1 0 0 CYP 450 Dose mg (bd) 400 150 20 150 Cimetidine Ranitidine Famotidine Nizatidine Comparison of H2 antagonists Antiandrogenic effect, prolactin secretion and gynocomastia
- 34. H2 antagonists - Uses Promote the healing of gastric and duodenal ulcers • Duodenal ulcer – 70 to 90% • Gastric Ulcer – 50 to 75% (NSAID ulcers)) • Stress ulcer and gastritis • GERD • Zollinger-Ellison syndrome • Prophylaxis of aspiration pneumonia • Urticaria Doses: • 300 mg/40 mg/150 mg at bed time of R, F, Rox respectively for healing • Maintenance: 150/20/150 mg BD of R, F, Rox
- 35. H2 blockers Tablets in Peptic ulcer Cimetidine 800mg bedtime /400mgBd 400mg bedtime Ranitidine 300 mg bedtime/150mg BD 150 mg bedtime Famotidine 40 mg bedtime 20 mg bedtime Roxatidine 150 mg bedtime 75 mg bedtime
- 36. Question Your friend wants to take a H2 antagonist before he takes alcohol to avoid gastric irritation .He consults you .Which H2 antagonist will you ask him to take ? Ranitidine/Famotidine/Roxatidine/Tiznidine ?
- 37. H2 antagonists – contd. • Answer : Famotidine • Explanation : All H2 antagonist except famotidine inhibit gastric first pass metabolism of ethanol and increase its bioavailability
- 38. Proton Pump Inhibitors • Most effective drugs in antiulcer therapy • Prodrugs requiring activation in acid environment • Block enzymes responsible for secreting HCl - binds irreversibly to H+K+ATPase • Prototype: Omeprazole (Prilosec) • Examples: – Lansoprazole – Pantoprazole – Rabeprazole – Esomeprazole Omeprazole
- 39. Omeprazole - MOA • Substituted Benzimidazole derivative • Its a Prodrug • Diffuses into G. canaliculi = accumulation pH < 5 (proton catalyzed )= tetracyclic sulfenamide + sulphenic acid • Covalent binding with sulfhydryl cysteines of H⁺K⁺ ATPase • Irreversible inactivation of the pump molecule (The charged forms cannot diffuse back across the canaliculi) • Acid suppressants regardless of stimulating factors • Also inhibits gastric mucosal carbonic anhydrase
- 40. Pharmacokinetics - PPI Oral forms are prepared as acid resistant formulations that release the drug in the intestine (because they are degraded in acid media) After absorption, they are distributed by blood to parietal cell canaliculi They irreversibly inactivate the proton pump molecule – but half life is very short and only 1-2 Hrs Still action persists for 24 Hrs to 48 hrs after a single dose – irreversible inhibition of PPI and new PP synthesis takes time (24 to 48 hour suppression of acid secretion, despite the much shorter plasma half-lives of the parent compounds) Platue state is attained after 4-5 days of dosing Action lasts for 4-5 days even after stoppage of the drug
- 41. Question • Half life of proton pump inhibitors is 1.5 hours only and these drugs are generally given once daily. How this can be justified ? • Answer : – P.P.I - Irreversible inhibitors of H+K+ATPase (Hit and run drugs)
- 42. Pharmacokinetics - PPI Given on an empty stomach because food affects absorption They should be given 30 minutes to 1 hour before food intake because an acidic pH in the parietal cell acid canaliculi is required for drug activation, and food stimulates acid production Concomitant use of other antisecretory drugs - H2 receptor antagonists – reduces action Highly protein bound and rapidly Metabolized by the liver by CYP2C19 and CYP3A4 – dose reduction necessary in severe hepatic failure Excreted in Kidneys minimally (no dose reduction needed in renal failure and elderly)
- 43. Adverse Effects The most common are GIT troubles in the form of nausea, abdominal pain, constipation, flatulence, and diarrhea Subacute myopathy, arthralgias, headaches, and skin rashes Prolonged use: Gynaecomastia, erectile dysfunction Leucopenia and hepatic dysfunction Vitamin B12 deficiency Hypergastrinemia which may predispose to rebound hypersecretion of gastric acid upon discontinuation of therapy and may promote the growth of gastrointestinal tumors (carcinoid tumors )
- 44. PPI – contd. • Drug Interaction: – Inhibits metabolism of Warfarin, Diazepam • Therapeutic uses: 1. Gastroesophageal reflux disease (GERD) 2. Peptic Ulcer - Gastric and duodenal ulcers 3. Bleeding peptic Ulcer 4. Zollinger ellison Syndrome 5. Prevention of recurrence of nonsteroidal antiinflammatory drug (NSAID) - associated gastric ulcers in patients who continue NSAID use. 6. Reducing the risk of duodenal ulcer recurrence associated with H. pylori infections 7. Aspiration Pneumonia
- 45. PPI – Dosage schedule • Omeprazole 20 mg o.d. • Lansoprazole 30 mg o.d. • Pantoprazole 40 mg o.d. • Rabeprazole 20 mg o.d. • Esomeprazole 20 - 40 mg o.d.
- 46. Muscarinic antagonists Atropine: – Block the M1 class receptors – Reduce acid production – Abolish gastrointestinal spasm Pirenzepine and Telenzepine Mechanism of action: • Reduce meal stimulated HCl secretion by reversible blockade of muscarinic (M1) receptors on the cell bodies of the intramural cholinergic ganglia (receptors on parietal cells are M3). • Unpopular as a first choice because of high incidence of anticholinergic side effects (dry mouth and blurred vision)
- 47. Prostaglandin analogues • Inhibit gastric acid secretion • Exhibit ‘cytoprotective’ activity • Enhance local production of mucus or bicarbonate • Promote local cell regeneration • Help to maintain mucosal blood
- 48. Prostaglandin analogues - Misoprostol Actions: Inhibit histamine-stimulated gastric acid secretion Stimulation of mucin and bicarbonate secretion Increase mucosal blood flow (Reinforcing of mucous layer buffered by HCO3 secretion from epithelial cells) Therapeutic uses: Prevent ion of NSAID-induced mucosal injury (rarely used because it needs frequent administration – 4 times daily)
- 49. Misoprostol • Doses: 200 mcg 4 times a day (Misoprost) • ADRs: – Diarrhoea and abdominal cramps – Uterine bleeding – Abortion – Exacerbations of inflammatory bowel disease and should be avoided in patients with this disorder Contraindications: 1. Inflammatory bowel disease 2. Pregnancy (may cause abortion)
- 50. Question A patient comes to your clinic at midnight complaining of heart burn. You want to relieve his pain immediately. What drug will you choose?
- 51. Answer is Antacids • Explanation : Antacids neutralize the already secreted acid in the stomach. All other drugs act by stopping acid secretion and so may not relieve symptoms atleast for 45 min
- 52. Eradication of H.pylori ! Omeprazole Amoxicillin Clarithromycin Metronidazole
- 53. Triple Therapy The BEST among all the Triple therapy regimen is: Omeprazole / Lansoprazole - 20 / 30 mg bd Clarithromycin - 500 mg bd Amoxycillin / Metronidazole - 1gm / 500 mg bd Given for 14 days followed by P.P.I for 4 – 6 weeks Short regimens for 7 – 10 days not very effective
- 54. Triple Therapy – cont … Bismuth subsalicylate – 2 tab qid Metronidazole - 250 mg qid Tetracycline - 500 mg qid Some other Triple Therapy Regimens are Ranitidine Bismuth citrate - 400 mg bd Tetracycline - 500 mg bd Clarithromycin / Metronidazole - 500 mg bd
- 55. Bismuth subsalicylate Pharmacological actions: • Undergoes rapid dissolution in the stomach into bismuth and salicylates • Salicylates are absorbed • Bismuth coats ulcers and erosions protecting them from acid and pepsin and increases prostaglandin and bicarbonate production • Uses: • Treatment of dyspepsia and acute diarrhoea
- 56. Question A pregnant lady (first trimester) comes to you with peptic ulcer disease. Which drug will you prescribe for her ?
- 57. Answer: Antacids or Sucralfate Explanation ; H2 antagonists cross placenta and are also secreted in breast milk. Safety of Proton pump inhibitors not established in pregnancy. Misoprostol causes abortion
- 58. Additional Drugs causing peptic ulcer: • Non Steroidal Anti Inflammatory Drugs (NSAIDs) • Glucocorticoids • Cytotoxic agents Stress induced ulceration after head trauma -Cushing’s ulcer Stress induced ulceration after severe burns - Curling’s ulcer
- 59. H2 Receptor Antagonists - in stomach at all stages decreases formation of HCl by selective blocking of H2 receptors - therapeutic effect after 4 weeks - 60 -80% efficiency, after 8 weeks even 90%, 10-15% resistance Ranitidine, Famotidine /more effective/, Nizatidine: /1- 2x daily/ - good pharmacokinetic /p.o. absorbtion, metabolism in liver/ and safety profile, good tollerance - long-term maintenance therapy after uncomplicated peptic ulcer healing and treatment of some forms of gastric dyspepsiasKhublei Shibun /Mitela/ Thank you
Editor's Notes
- #13: Infection with Helicobacter pylori, a short, spiral-shaped, microaerophilic gram-negative bacillus, is the leading cause of PUD and is associated with virtually all ulcers not induced by NSAIDs. H pylori colonize the deep layers of the mucosal gel that coats the gastric mucosa and presumably disrupts its protective properties. H pylori is thought to infect virtually all patients with chronic active gastritis.
- #40: 2 charged cationic forms