Basic principle of ct and ct generations
- 1. Supervising Faculty: Dr. B. P. Baruah Mentor: Dr. Sushma Rani Presenter: Dr. Tarun Goyal
- 2. A conventional X-ray image is basically a shadow. Shadows give you an incomplete picture of an object's shape. This is the basic idea of computer aided tomography. In a CT scan machine, the X- ray beam moves all around the patient, scanning from hundreds of different angles.
- 3. Designed by Godfrey N. Hounsfield to overcome the visual representation challenges in radiography and conventional tomography by collimating the X-ray beam and transmitting it only through small cross-sections of the body. In 1979, G.N. Hounsfield shared the Nobel Prize in Physiology & Medicine with Allan MacLeod Cormack, Physics Professor who developed solutions to mathematical problems involved in CT. Godfrey N. Hounsfield Allan MacLeod Cormack
- 4. Year Event 1917 Austrian mathematician Johann Radon proved that a 2D/3D object could be reproduced from an infinite set of all its projections 1956 Bracewell, working in radioastronomy, constructed a solar map from ray projections. 1961 and 1963 Oldendorf and Cormack understood the concept of computed tomography and built laboratory models. 1968 Kuhl and Edwards built a successful mechanical scanner for nuclear imaging, but did not extend their work into diagnostic radiology 1969 G.N. Hounsfield developed first clinically useful CT head scanner 1971 First clinically useful CT head scanner was installed at Atkinson- Morley Hospital (England) 1972 First paper on CT presented to British Institute of Radiology by Hounsfield and Dr. Ambrose
- 5. Computed Tomography, CT for short (also referred to as CAT, for Computed Axial Tomography), utilizes X-ray technology and sophisticated computers to create images of cross-section “slices” through the body. Tomography is a term that refers to the ability to view an anatomic section or slice through the body. Anatomic cross sections are most commonly refers to transverse axial tomography.
- 6. Basics Principle The basic principle behind CT is that the internal structure of an object can be reconstructed from multiple projections of the object. The ray projections are formed by scanning a thin cross section of the body with a narrow x-ray beam and measuring the transmitted radiation with a sensitive radiation detector. CT scanning is a systematic collection and representation of projection data
- 7. Parts of CT Scan Machine The basic technology employed in the CT scanner is designed to provide a source of x-rays to be transmitted through the patient and then get detected by the detectors. The CT system consists of: 1. a computer work station for operation of the scanner, 2. image processing computers, 3. electronic cabinets, 4. the gantry 5. and the patient imaging table.
- 8. Composition Of Gantry 1. The gantry houses the key components of the scanner. 2. Production of the x-ray beam and detection and acquisition of the beam must be located within the rotating portion of the gantry. 3. The fan-beam x-ray tube sits opposite the detector array within the rotating gantry. 4. The three phase power generator is also within the gantry module. 5. The x-ray tube in a CT scanner is designed to produce a fan beam of x-rays that is approximately as wide as the body. 6. Tissue attenuation is measured over a large region from one position of the x-ray tube. 7. On the opposite side of the patient is the detector array that measures the strength of the x-ray beam at various points laterally across the body.
- 9. A look inside of the Gantry T: X-ray tube D: X-ray detectors X: X-ray beam R: Gantry rotation
- 10. X Ray Tubes The radiation source for CT would supply a monochromatic x-ray beam (i.e., one made up of photons all having the same wavelength) with advantage that image reconstruction is simpler and more accurate. Earlier models used oil-cooled, fixed-anode, relatively large (2 X 16 mm) focal spot tubes at energies of about 120 kV (constant potential) and 30 mA. The beam was heavily filtered to remove low energy photons and to increase the mean energy of the radiation. New fan beam units have a diagnostic type x-ray tube with a rotating anode and a much smaller focal spot around (0.6 mm). These tubes have large heat loading and heat dissipation capabilities to withstand the very high heat loads generated when multiple slices are acquired in rapid sequence
- 11. X-ray beam collimated at two points, one close to the x- ray tube and the other at the detector(s) with perfect alignment. Each detector has its own collimator. Collimator at the detector controls scatter radiation. The collimators also regulate the thickness of the tomographic slice (i.e., the voxel length). Pixel size is determined by the computer program and not by the collimator. COLLIMATORS
- 12. DETECTORS Two types of detectors are used 1. Scintillation Detectors 2. Gas Filled Detectors Scintillation Detectors These are the materials that will produce light (scintillate) when ionizing radiation reacts with them. The combination of a scintillation crystal and the light detector is called a scintillation detector. Material Used: 1. Sodium Iodide (Nal) 2. Cesium Iodide(Csl), 3. Bismuth Germinate (BGO) and 4. Cadmium Tungstate (CdW04
- 13. Xenon Gas Ionization Chambers Those rotate-rotate CT units that do not use scintillating crystals use xenon gas ionization chambers. Regardless of the shape or size, all gas-filled detectors use ionization of the gas by the incoming radiation to produce a signal. Photon interacts with gas atom by ionizing the atom into an electron-ion pair. Voltage between the anode and cathode will cause the electron to move toward the anode, and the positive ion to move toward the cathode. When the electrons reach the anode, they produce a small current in the anode. This small current is the output signal from the detector.
- 14. Data Accumulation Data-gathering techniques have developed by stages. These stages have been called "generations.“ The number of ray projections increases from 28,800 in the original scanner to more than one million in newer scanners. Image quality is related to the number of ray projections used to reconstruct each CT scan image Eliminates the superimposition of structures Sensitive to subtle differences in x-ray attenuation
- 15. The average linear attenuation coefficient (µ), between tube and detectors Attenuation coefficient reflects the degree to which the X-ray intensity is reduced by a material What are we measuring?
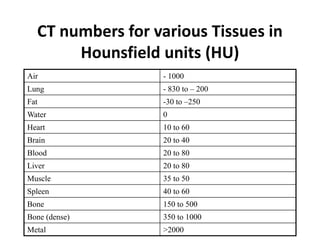
- 16. The computer calculates a relationship between the linear attenuation coefficients of the pixel and water which is given as CT number. To image materials with higher than dense bone CT number larger than 1000 should be available CT numbers based on a magnification constant of 1000 are Hounsfield units CT NUMBER & HOUNSFIELD UNIT
- 17. Values of CT Image Reconstruction • CT numbers (Hounsfield units) are the pixel values assigned in the image • They are computed by calculating the relative difference between the linear attenuation coefficient of tissue and that of water
- 18. Hounsfield Units (HU) or CT numbers Calculation • For tissue and that of water the equation is: CTTissue = (µtissue - µwater)/µwater x 1000 • The CT number for water has a value of 0 because: (µtissue - µwater)/µwater = 0
- 19. CT numbers for various Tissues in Hounsfield units (HU) Air - 1000 Lung - 830 to – 200 Fat -30 to –250 Water 0 Heart 10 to 60 Brain 20 to 40 Blood 20 to 80 Liver 20 to 80 Muscle 35 to 50 Spleen 40 to 60 Bone 150 to 500 Bone (dense) 350 to 1000 Metal >2000
- 20. • CT image is displayed on TV monitor for immediate viewing and recorded on film for storage • Display matrix has on average 512x512 some may have 1024x1024 • But one display has only 256 shades of gray • Thus, we are going to image CT no from -1000 to 1000 with 256 shades of gray • Pixel size on average 0.1 mm with scan field view of 40cm • With pixel size of 0.1 mm ,40 cm scan field contain 4000 pixels • These 4000 pixels displayed on 512x 512 TV monitor will result in 8 pixel per matrix element IMAGE DISPLAY
- 21. Now the challenge is how to display CT no from -1000 to 1000 with only 256 shades of gray 1. Thus, assign 8 CT no.s to the same shade of gray and display entire range of information in compressed scale. 2. And select a CT no that will be average of body examined Computer instructed to assign one shade of gray to each of 128 CT no below and 128 CT no above baseline. Centre CT no is ‘window level’ Range of CT no's above and below are called ‘window width’ This leads to the concept of Windowing, also known as grey- level mapping, contrast stretching, histogram modification or contrast enhancement
- 22. The values below are written as width and level (W:x L:y) in Hounsfield units (HU). head and neck brain W:80 L:40 subdural W:130-300 L:50-100 stroke W:8 L:32 or W:40 L:40 3 temporal bones W:2800 L:600 soft tissues: W:350–400 L:20–60 4 chest lungs W:1500 L:-600 mediastinum W:350 L:50 abdomen soft tissues W:400 L:50 liver W:150 L:30 spine soft tissues W:250 L:50 bone W:1800 L:400
- 24. Image Quality Image quality is the visibility of diagnostically important structures in the CT image. The factors that affect CT image quality are 1. Quantum mottle (noise) 2. Resolution (Spatial and contrast) 3. Patient exposure.
- 25. • Quantum mottle is the statistical fluctuations of X- photons absorbed by the detector • The only way to decrease noise is to increase the number of photons absorbed by the detector • The way to increase the number of photons absorbed is to increase x-ray dose to the patient. • Mottle becomes more visible as the accuracy of the reconstruction improves Quantum Mottle (NOISE)
- 26. RESOLUTION Spatial Resolution Contrast Resolution Spatial resolution is the ability of the CT scanner to display separate images of two objects placed close together Contrast resolution is the ability of the CT scanner to display an image of a relatively large (2 or 3mm) object that is only slightly different in density from its surroundings.
- 27. RADIATION DOSE • Even distribution of radiation dose to the tissues as exposures are from almost all angles. • No overlapping of scan fields takes place. • Exposure factors used are higher to improve spatial and contrast resolutions and to reduce noise.
- 28. Scanning Motions CT scanners have gone through a number of design changes since the technology was first introduced in 1971. Scan time reduction is the predominant reason for introducing new configurations. We will discuss geometry of design in five categories: 1. First generation (translate-rotate, one detector) 2. Second generation (translate-rotate, multiple detectors) 3. Rotate-rotate (third generation) 4. Rotate-fixed (fourth generation) 5. Other geometries
- 29. Original EMI Scanner / 1st Generation CT Original EMI unit was a first-generation scanner Employed a pencil-like x-ray beam and a single detector; that is, one detector per tomographic section Five-view study of the head took about 25 to 30 minutes Was designed specifically for evaluation of the brain Gantry moved through two different types of motion, one linear and the other rotary
- 30. linear motion was repeated over and over 180 times. Between each of these 180 linear movements, the gantry rotated 1°. Thus, the total rotary motion encompassed a 180° semicircle. The axis of rotation passed through the center of the patient's head The x-ray beam was "on“ throughout the linear movement and "off “ during the rotary movements The total number of transmission measurements was the product of the number of linear measurements (160) and rotary steps (180), which was 28,800 in the original EMI scanner. The transmission readings represented a composite of the absorption characteristics of all the elements in the path of the beam
- 31. In the original EMI scanner, the CT image was reconstructed and then displayed on an 80 X 80 matrix in two different formats: a paper printout of CT numbers and a visual image on a cathode ray tube. CT numbers were proportional to the linear attenuation coefficient. Each square in the image matrix was called a pixel, and it represented a tiny elongated block of tissue called a voxel. An oil-cooled stationary anode tube was used in the original EMI scanner. Its nominal focal spot size was 2.25 X 12 mm. The tube was operated at 120 kVp and 33 mA. The x-ray beam was heavily filtered with a half-value layer of 6 mm of aluminum. Beam size was restricted by a pair of slit like collimators, one near the tube and the other near the detectors.
- 32. This is the first CT image taken by first generation CT.
- 33. • Cross sectional layer of the body is represented as an image matrix. • Each square of the image matrix is called pixel(picture element) and it represents tiny block of tissue called voxel (volume element)
- 34. 2nd Generation CT The main objective for its development was to shorten the scanning time for each tomographic section This was achieved by abandoning the single detector and pencil beam of the original EMI scanner and adopting a fan-shaped beam and multiple detectors. The movements of the x-ray tube- detector array are both linear and rotary, just like a first generation scanner, but the rotary steps are larger. Instead of moving 1°at the end of each linear scan, the gantry rotates through a greater arc, up to 30°.
- 35. With 30 detectors, the linear movements only have to be repeated six times rather than the 180 linear movements of the original EMI unit. Second-generation scanners produced a tomographic section in between 10 and 90 sec, depending on the manufacturer. The other advantage of 2nd Gen CT other than reducing imaging time is that thorax can also be imagined. By adding detectors angularly displaced, several projections could be obtained in a single translation.
- 36. 3rd Generation (Rotate/Rotate type) Introduced by General Electric Company in 1975 in which complete translation motion was eliminated. Only rotation motion was required, with both the x-ray tube and detectors rotating around the patient
- 37. This scanning geometry came to be known as "fan beam" geometry, or "third-generation" geometry, and the original unit could produce a scan in 4.9 sec. Multiple detectors are aligned along the arc of a circle whose center is the x-ray tube focal spot Both the x-ray tube and detectors rotate about the patient (rotate-rotate geometry) in concentric circles whose centers approximately coincide with the center of the patient. Detectors vary in no. from 288 from the original to 700 in modern equipments. The fan beam must completely cover the object to be imaged. In the original rotate-rotate scanners the x-ray tube was pulsed. Each pulse of the tube produced one projection, and the number of scan lines in each projection was equal to the number of detectors.
- 38. In some rotate- rotate scanners the x-ray tube is continuously on, and individual projections are obtained by reading the output of the detectors at rapid intervals. Let us not confuse ourselveswiththe terms“CT Image, Projections and Line”. The CT image is the image of one CT slice that is viewed on the TV monitor or on film. The image is computed from many projections A projection is produced each time the detectors are read. Therefore, the data contained in a projection is a set of readings composed of one signal from each detector that has been exposed to the x-ray beam. We describe the data (signal) collected from one exposed detector as a line, or scan line.
- 39. 4th Generation CT scanners (Rotate-Fixed type) Detectors form a ring that completely surrounds the patient and they do not move. (Stationary detector ring and rotating X-ray tube) The x-ray tube rotates in a circle inside the detector ring, and the x-ray beam is collimated to form a fan beam. When the x-ray tube is at prescribed angles, the exposed detectors are read. One CT scan will be made up of many projections, each projection taken at a slightly different angle and that is why continuous-on x-ray tubes are generally used today.
- 40. The detectors in a fan beam array have their own individual collimators. Most scattered photons are absorbed by these collimators. The advantage of a fan-beam/multiple detector array is speed (reduced to few seconds). One principal disadvantage of the fan beam is an increased amount of scattered radiation.
- 41. Other Scan Configurations This include but is not limited to: 5th generation / CINE CT / CVCT 6th generation / Spiral CT/ HELICAL CT 7th generation / cone beam CT MultiSlice CT
- 42. CineCT /Ultrafast CT ● Nomechanicalscanning motion ● X-raydetector andtube anodeare stationary. It incorporates a semicircular tungsten x-ray target into the gantry. ● Anode,isaverylargesemicircularringthat formsanarc aroundthe patient scancircle. ● Source of X-raysismoved around the samepath asafourth generation CTscannerbysteeringanelectron beamaroundthe X-ray anode ● Fifty millisecond multilevel scanning at rates of 17 scans per second allows quantization of left ventricular (LV) function at each tomographic level during a cardiac cycle.
- 43. Capable of scanning entire airway from nasopharynx to larynx i.e distance of ~8cm in 0.24 seconds. It allow analysis of entire airway during inspiration, expiration and apenic episodes. Cine CT systems although have higher noise level and lower spatial resolution but are ideal for cardiac imaging , lung imaging and pediatric studies. A very fast scanner collecting data for 1 slice in 50 to 100ms. Sweeps an intense electron beam across large stationary anode target which surrounds the patient.
- 44. 5th Gen CT / IMATRON / CVCT / CINE CT / Ultrafast CT
- 45. SPIRAL CT / HELICAL CT ● Design:x-raytuberotates aspatientismoved smoothlyintox-rayscan field ● Simultaneoussourcerotation, tabletranslation anddata acquisition ● Producesonecontinuousvolumesetofdatafor entire region ● Dataformultipleslicesfrompatientacquiredat 1sec/slice Threetechnological developments: 1. Slip-ringgantry designs 2. Veryhighpowerx-ray tubes 3. Interpolationalgorithmsto handleprojection data
- 46. Continuous rotation of the x-ray tube and detectors and simultaneous translation of the patient through the gantry opening. q Slip rings are circular electrical conductive rings and brushes which transmits electrical energy across moving interface. It allows scan frame to rotate continuously with no need to stop between rotations to rewind system cables. Interpolation methods developed by Kalender are used to generate projections in a single plane. The overlapping sections generated by math, not beam improves Z axis with no increase in dose which helps in improving image quality.
- 47. In helical CT, pitch is the ratio of the patient’s movement through the gantry during one 360 degree rotation relative to the beam collimation. For single slice CT, Pitch is equal to the table movement per rotation divided by slice collimation. On most CT and PET/CT systems the pitch is entered as a parameter that is set in defining the procedure for the acquisition of patient data. When the pitch is greater than 1.0 mm, there are interspaces created and some portion of the body is being missed. PITCH
- 48. The increment is the distance between the slices. In CT data are acquired as projection information along the helical path. Slices may be reconstructed at various positions along the helix. One important factor in defining the slices and their positional relationship to one another is the distance between the reconstructed axial slices in the ‘z’ direction. INCREMENT
- 49. Advantages of Spiral CT • Faster image acquisition • Quicker response to contrast media • Fewer motion artifacts • Improved two-axis resolution • Physiological imaging • Improved coronal, sagittal, and 3D imaging • Less partial volume artefact
- 50. 7th Generation CT It is a new technology to overcome the limitations of single row detectors; hence it has multiple detector array. The collimator spacing is wider and more of the x rays produced by x ray tube are used in producing image data.
- 51. There is formation of cone beam and multiple parallel rows of detectors. Widened ( Z-direction) X ray beam and detector array to acquire multiple slices This gives advantage of reducing scan time with increased Z- Resolution but it is very expensive.
- 52. MultiSlice CT ● Relatesto the techniqueofdoubleor triple rotationofthe tube and detectors aroundthe sameaxial plane ● Providesdoubleoftriple the volume per slice,uponwhich the finalimage canbe derived ● Inpracticeeachrotationproducesits ownbankof rawdata, ● Multiscanningtherefore reducesmotionartifactsand consequentlyimprovesimage quality ● Development insoftwareand computer capacityleadto processingand reconstruction inashorttime
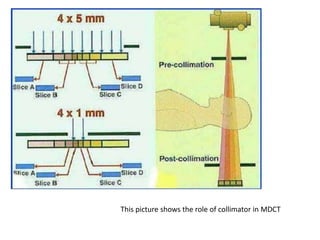
- 53. This picture shows the role of collimator in MDCT
- 54. Multiple detector array illustration Image showing comparison of the different geometrical generations
- 55. Generation Source Source Collimation Detector 1st Single X-ray Tube Pencil Beam Single 2nd Single X-ray Tube Fan Beam (not enough to cover FOV) Multiple 3rd Single X-ray Tube Fan Beam (enough to cover FOV) Many 4th Single X-ray Tube Fan Beam covers FOV Stationary Ring of Detectors 5th Many tungsten anodes in single large tube Fan Beam Stationary Ring of Detectors 6th 3G/4G 3G/4G 3G/4G 7th Single X-ray Tube Cone Beam Multiple array of detectors
- 56. Let us know our department CT machine Setup.. Name: GE Optima 660 – 128 slice Computed Tomographic Scanner with slice thickness of 0.35mm with Advantage Workstation (AW) Volume Share workstation. It has got the Performix 40 tube, backed by a powerful 72-kW generator, delivers peak mA capability of up to 600 mA. The 40-mm wide V-Res detector (HiLight scintillator) acquires data at 0.35-mm microVoxel spatial resolution through GE innovations. The Optima CT660 image chain is powered by the Volara XT Data Acquisition System (DAS).
- 57. Performix 40 X ray Tube Cone-beam filtered back projection utilizes two sets of counter-opposed projections to provide 128 distinct projection measurements per rotation for axial and a helical acquisition mode. For cardiac acquisitions, fast rotation speed provides excellent temporal resolution (44 msec). The table allows patients as heavy as 500 lbs (226.796 kgs) to be imaged through a long scannable range.
- 58. In computed tomography (CT), the term artifact is applied to any systematic discrepancy between the CT numbers in the reconstructed image and the true attenuation coefficients of the object. CT images are inherently more prone to artifacts than conventional radiographs because the image is reconstructed from something on the order of a million independent detector measurements. CT Scanner Artifacts
- 59. Types of artifact 1. Streaking, which is generally due to an inconsistency in a single measurement 2. Shading, which is due to a group of channels or views deviating gradually from the true measurement 3. Rings, which are due to errors in an individual detector calibration 4. Distortion which is due to helical reconstruction.
- 60. ON BASIS OF ORIGIN 1. Physics-based artifacts, which result from the physical processes involved in the acquisition of CT data 2. Patient-based artifacts (motion artifacts) which are caused by such factors as patient movement or the presence of metallic materials in or on the patient 3. Scanner-based artifacts, which result from imperfections in scanner function 4. Helical and multi-section artifacts, which are produced by the image reconstruction process.
- 61. BEAM HARDENING ARTIFACT • can give a "cupped appearance" when grayscale is visualized as height • As heterogeneous/polychromatic X ray beam passes through patient, low energy photons are absorbed • the mean energy of the spectrum increases when passing the object, often described as getting "harder" • Linear attenuation coefficient is directly related to energy • Linear attenuation coefficient of tissue near beam entry is higher than that on exit side • leads to an effect increasingly underestimating material thickness
- 62. • Cause: presence of tissues with highly varying absorbtion properties in a voxel. • Rectification : Usage of Thinner CT slices Partial Volume Averaging Artifact Thick slice Thin slice
- 63. Motion Artifact Streak Artifact Ring Artifact