Thiamine
- 1. Thiamine- Chemistry, functions and clinical significance Biochemistry for Medics http://www.namrata.co/ 1Biochemistry for medics
- 2. Thiamine- Introduction also known as vitamin B1, anti beriberi factor or anti-neuritic vitamin is an important water-soluble vitamin is involved in carbohydrate, fat, amino acid, glucose, and alcohol metabolism. is required as a coenzyme in enzymatic reactions that involve the transfer of an aldehyde group. is essentially nontoxic. 2Biochemistry for medics
- 3. Thiamine - Structure Thiamine contains a substituted pyrimidine ring (dimethyl 6-amino pyrimidine) connected to a substituted thiazole ring (Methyl hydroxy ethyl thiazole) by means of Methylene bridge. 3Biochemistry for medics
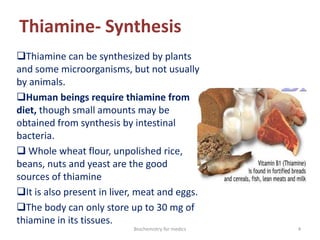
- 4. Thiamine- Synthesis Thiamine can be synthesized by plants and some microorganisms, but not usually by animals. Human beings require thiamine from diet, though small amounts may be obtained from synthesis by intestinal bacteria. Whole wheat flour, unpolished rice, beans, nuts and yeast are the good sources of thiamine It is also present in liver, meat and eggs. The body can only store up to 30 mg of thiamine in its tissues. 4Biochemistry for medics
- 5. Thiamine-Occurrence It is present in large amounts in skeletal muscle, heart, liver, kidney, and brain. It has a widespread distribution in foods, but there can be a substantial loss of thiamine during cooking above 100°C (212°F). The half-life of thiamine is 9-18 days. It is excreted by the kidney. 5Biochemistry for medics
- 6. Activation of Thiamine The active form of the coenzyme, thiamine pyrophosphate (thiamine diphosphate, TPP), is synthesized by an enzymatic transfer of a pyrophosphate group from ATP to thiamine). 6Biochemistry for medics
- 7. Recommended daily Allowance of thiamine Depends on calorie intake (0.5 mg/1000 cals) RDA is 1-1.5 mg/day Requirement increases with- o increased carbohydrate intake o Pregnancy o Lactation o Smoking o Alcoholism o Prolonged antibiotic intake o Serious or prolonged illness 7Biochemistry for medics
- 8. Metabolic role of Thiamine Thiamine has a central role in energy-yielding metabolism, and especially the metabolism of carbohydrates Thiamine pyrophosphate is an essential cofactor for enzymes that catalyze the oxidative decarboxylation of α-keto acids to form an acylated coenzyme A (acyl CoA). These include pyruvate dehydrogenase , α -keto glutarate dehydrogenase and branched-chain α- keto acid dehydrogenase. These three enzymes operate by a similar catalytic mechanism. 8Biochemistry for medics
- 9. Role of TPP in Pyruvate dehydrogenase complex The pyruvate dehydrogenase complex is a large, highly integrated complex of three kinds of enzymes; Pyruvate dehydrogenase, dihydrolipoyl transacetylase and Dihydrolipoyl dehydrogenase. At least two additional enzymes regulate the activity of the complex and five coenzymes: thiamine pyrophosphate (TPP), lipoic acid, CoASH, FAD and NAD+ participate in the overall reaction. 9Biochemistry for medics
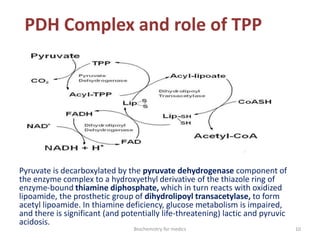
- 10. PDH Complex and role of TPP Pyruvate is decarboxylated by the pyruvate dehydrogenase component of the enzyme complex to a hydroxyethyl derivative of the thiazole ring of enzyme-bound thiamine diphosphate, which in turn reacts with oxidized lipoamide, the prosthetic group of dihydrolipoyl transacetylase, to form acetyl lipoamide. In thiamine deficiency, glucose metabolism is impaired, and there is significant (and potentially life-threatening) lactic and pyruvic acidosis. 10Biochemistry for medics
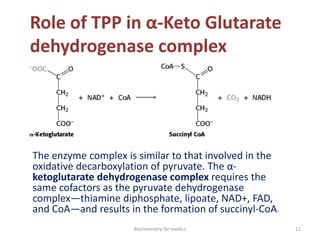
- 11. Role of TPP in α-Keto Glutarate dehydrogenase complex The enzyme complex is similar to that involved in the oxidative decarboxylation of pyruvate. The α- ketoglutarate dehydrogenase complex requires the same cofactors as the pyruvate dehydrogenase complex—thiamine diphosphate, lipoate, NAD+, FAD, and CoA—and results in the formation of succinyl-CoA. 11Biochemistry for medics
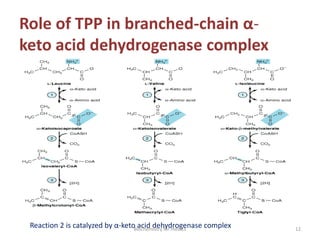
- 12. Role of TPP in branched-chain α- keto acid dehydrogenase complex Reaction 2 is catalyzed by α-keto acid dehydrogenase complex 12Biochemistry for medics
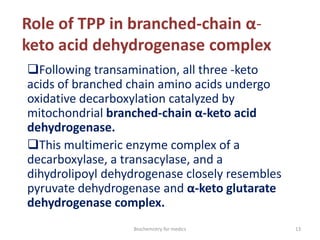
- 13. Role of TPP in branched-chain α- keto acid dehydrogenase complex Following transamination, all three -keto acids of branched chain amino acids undergo oxidative decarboxylation catalyzed by mitochondrial branched-chain α-keto acid dehydrogenase. This multimeric enzyme complex of a decarboxylase, a transacylase, and a dihydrolipoyl dehydrogenase closely resembles pyruvate dehydrogenase and α-keto glutarate dehydrogenase complex. 13Biochemistry for medics
- 14. Role of TPP in Transketolase reaction Thiamine pyrophosphate is also an important cofactor for the Transketolase reactions in the pentose phosphate pathway of carbohydrate metabolism. These reactions are important in the reversible transformation of pentoses into the glycolytic intermediates fructose 6-phosphate and glyceraldehyde 3-phosphate. Transketolase transfers the two-carbon unit comprising carbons 1 and 2 of a ketose onto the aldehyde carbon of an aldose sugar. It therefore effects the conversion of a ketose sugar into an aldose with two carbons less and an aldose sugar into a ketose with two carbons more. The reaction requires Mg2+ and thiamine diphosphate (vitamin B ) as coenzyme. 14Biochemistry for medics
- 15. Role of TPP in Transketolase reaction 15Biochemistry for medics
- 16. Role of TPP in Tryptophan Metabolism Thiamine is also required for the metabolism of Tryptophan( As a coenzyme for Tryptophan pyrrolase) Tryptophan oxygenase (tryptophan pyrrolase) opens the indole ring, incorporates molecular oxygen, and forms N-formyl kynurenine. 16Biochemistry for medics
- 17. Role of TPP in nerve conduction Thiamine pyrophosphate has a role in nerve conduction; It phosphorylates, and so activates, a chloride channel in the nerve membrane. Thiamine appears to have a role in axonal conduction particularly in acetyl cholinergic and serotoninergic neurons. 17Biochemistry for medics
- 18. Thiamine deficiency and impaired reactions A deficiency in thiamine will decrease the efficiency of the enzymes for which TPP is required as a cofactor. Thus, the rate of conversion of pyruvate to acetyl-CoA and the flow of acetyl-CoA through the tricarboxylic acid cycle will be depressed as a result of the inefficiency of the TPP- requiring enzymes pyruvate dehydrogenase and α-keto glutarate dehydrogenase. 18Biochemistry for medics
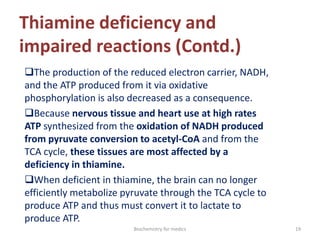
- 19. Thiamine deficiency and impaired reactions (Contd.) The production of the reduced electron carrier, NADH, and the ATP produced from it via oxidative phosphorylation is also decreased as a consequence. Because nervous tissue and heart use at high rates ATP synthesized from the oxidation of NADH produced from pyruvate conversion to acetyl-CoA and from the TCA cycle, these tissues are most affected by a deficiency in thiamine. When deficient in thiamine, the brain can no longer efficiently metabolize pyruvate through the TCA cycle to produce ATP and thus must convert it to lactate to produce ATP. 19Biochemistry for medics
- 20. Thiamine deficiency and impaired reactions (Contd.) A deficiency in thiamine also adversely affects the flux of glucose metabolized by the pentose phosphate pathway. When these reactions cannot proceed, precursor metabolites build up, and the flow through the pathway is decreased. This results in a decreased production of NADPH and decreased conversion of glucose to pentose, including ribose. This can lead to decreased regeneration of reduced glutathione and susceptibility to oxidative stress. 20Biochemistry for medics
- 21. Thiamine deficiency(Beri-Beri) Beriberi is observed in developed nations in- persons with alcoholism, people on fad diets, persons on long-term peritoneal dialysis without thiamine replacement, persons undergoing long-term starvation, or persons receiving intravenous fluids with high glucose concentration. 21Biochemistry for medics
- 22. Pathophysiology of Thiamine deficiency (Beri-Beri) Deficiency causes degeneration of peripheral nerves, thalamus, mammillary bodies, and cerebellum. Cerebral blood flow is markedly reduced, and vascular resistance is increased. The heart may become dilated; muscle fibers become swollen, fragmented, and vacuolized, with interstitial spaces dilated by fluid. Vasodilation occurs and can result in edema in the feet and legs. Arteriovenous shunting of blood increases. Eventually, high-output heart failure may occur. 22Biochemistry for medics
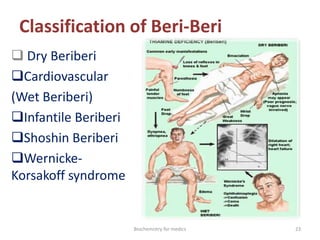
- 23. Classification of Beri-Beri Dry Beriberi Cardiovascular (Wet Beriberi) Infantile Beriberi Shoshin Beriberi Wernicke- Korsakoff syndrome 23Biochemistry for medics
- 24. Dry Beriberi Nervous system involvement is termed dry beriberi. The neurologic findings can be peripheral neuropathy characterized by symmetric impairment of sensory, motor, and reflex functions of the extremities These deficits are bilateral and roughly symmetric, occurring in a stocking-glove distribution. 24Biochemistry for medics
- 25. Dry Beriberi (Contd.) They affect predominantly the lower extremities, beginning with paresthesias in the toes, burning in the feet (particularly severe at night), muscle cramps in the calves, pains in the legs, and plantar dysesthesias. Calf muscle tenderness, difficulty rising from a squatting position, and decreased vibratory sensation in the toes are early signs Continued deficiency worsens polyneuropathy, which can eventually affect the arms. 25Biochemistry for medics
- 26. Dry Beriberi Deficiency causes degeneration of peripheral nerves, thalamus, mammillary bodies, and cerebellum. 26Biochemistry for medics
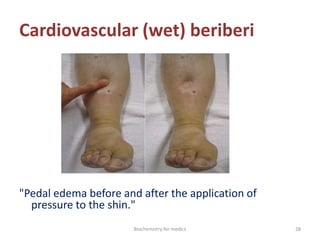
- 27. Cardiovascular (wet) beriberi Wet beriberi is the term used for the cardiovascular involvement of thiamine deficiency. The first effects are vasodilatation, tachycardia, a wide pulse pressure, sweating, warm skin, and lactic acidosis. Later, heart failure develops, causing orthopnea and pulmonary and peripheral edema. Vasodilatation can continue, sometimes resulting in shock. 27Biochemistry for medics
- 28. Cardiovascular (wet) beriberi "Pedal edema before and after the application of pressure to the shin." 28Biochemistry for medics
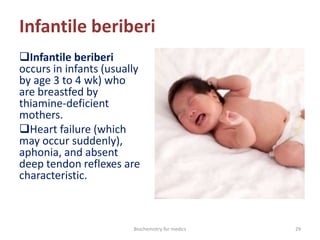
- 29. Infantile beriberi Infantile beriberi occurs in infants (usually by age 3 to 4 wk) who are breastfed by thiamine-deficient mothers. Heart failure (which may occur suddenly), aphonia, and absent deep tendon reflexes are characteristic. 29Biochemistry for medics
- 30. Shoshin beriberi Shoshin beriberi A more rapid form of wet beriberi is termed acute fulminant cardiovascular beriberi, or Shoshin beriberi. The predominant injury is to the heart, and rapid deterioration follows the inability of the heart muscle to satisfy the body's demands because of its own injury. In this case, edema may not be present. Instead, cyanosis of the hands and feet, tachycardia, distended neck veins, restlessness, and anxiety occur. 30Biochemistry for medics
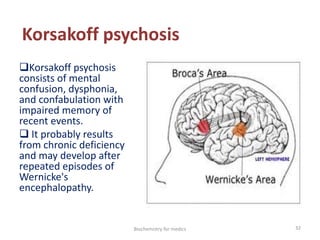
- 31. Wernicke-Korsakoff syndrome Wernicke-Korsakoff syndrome, which combines Wernicke's encephalopathy and Korsakoff's psychosis occurs in some alcoholics who do not consume foods fortified with thiamine. Wernicke's encephalopathy consists of psychomotor slowing or apathy, nystagmus, ataxia, ophthalmoplegia, impaired consciousness, and, if untreated, coma and death. 31Biochemistry for medics
- 32. Korsakoff psychosis Korsakoff psychosis consists of mental confusion, dysphonia, and confabulation with impaired memory of recent events. It probably results from chronic deficiency and may develop after repeated episodes of Wernicke's encephalopathy. 32Biochemistry for medics
- 33. Causes of thiamine deficiency Lack of thiamine intake Food containing a high level of thiaminase, including milled rice, raw freshwater fish, raw shellfish, and ferns Food high in anti-thiamine factor, such as tea, coffee, and betel nuts Processed food with a content high in sulfite, which destroys thiamine Alcoholic state Starvation state 33Biochemistry for medics
- 34. Causes of thiamine deficiency ( contd.) Increased consumption states Diets high in carbohydrate or saturated fat intake Pregnancy Hyperthyroidism Lactation Fever - severe infection Increased physical exercise 34Biochemistry for medics
- 35. Causes of thiamine deficiency (contd.) Increased depletion Diarrhea Diuretic therapies Peritoneal dialysis Hemodialysis Hyperemesis gravidarum 35Biochemistry for medics
- 36. Causes of thiamine deficiency (contd.) Decreased absorption Chronic intestinal disease Alcoholism Malnutrition Gastric bypass surgery Malabsorption syndrome - Celiac and tropical sprue 36Biochemistry for medics
- 37. Laboratory Studies in thiamine deficiency Diagnosis is usually based on a favorable response to treatment with thiamine in a patient with symptoms or signs of deficiency. Electrolytes, including Mg, should be measured to exclude other causes. For confirmation in equivocal cases, erythrocyte Transketolase activity and 24-h urinary thiamine excretion may be measured. Diagnosis of cardiovascular beriberi can be difficult if other disorders that cause heart failure are present. 37Biochemistry for medics
- 38. Treatment of Thiamine deficiency Supplemental thiamine, with dose based on clinical manifestations For mild polyneuropathy, thiamine 10 to 20 mg once/day is given for 2 wk. For moderate or advanced neuropathy, the dose is 20 to 30 mg/day; it should be continued for several weeks after symptoms disappear. For edema and congestion due to cardiovascular beriberi, thiamine 100 mg IV once/day is given for several days. 38Biochemistry for medics
- 39. Prognosis of Beriberi The prognosis for beriberi is usually good, unless patients have established Korsakoff syndrome. When patients have progressed to this stage, the degree of damage is only minimally reversible. 39Biochemistry for medics
- 40. Summary Beriberi Thiamine deficiency (causing beriberi) is most common among people subsisting on white rice or highly refined carbohydrates in developing countries and among alcoholics. Symptoms include diffuse polyneuropathy, high-output heart failure, and Wernicke-Korsakoff syndrome. Diagnosis is usually based on a favorable response to treatment with thiamine in a patient with symptoms or signs of deficiency. For confirmation in equivocal cases, erythrocyte transketolase activity and 24-h urinary thiamin excretion may be measured. Because thiamine deficiency often occurs with other B vitamin deficiencies, multiple water-soluble vitamins are usually given for several weeks 40Biochemistry for medics
- 41. Therapeutic uses of Thiamine Thiamine deficiency Thiamine is also used for digestive problems including poor appetite, ulcerative colitis, and ongoing diarrhea. also used for AIDS and boosting the immune system, diabetic pain, heart disease, alcoholism, aging, vision problems such as cataracts and glaucoma, motion sickness, and improving athletic performance. Other uses include preventing cervical cancer and progression of kidney disease in patients with type 2 diabetes. 41Biochemistry for medics