Barium meal follow through
- 1. v. Siva prakash Bsc.MIT 3nd year Saveetha medical college Chennai.
- 2. The study called because it is performed following barium meal..... For evaluating patients with suspected small bowel abnormalities Small bowel – ileocaecal junction 2SIVA PRAKASH
- 3. SMALL INTESTINE Is the longest part of alimentary canal Extends from pylorus of stomach ileocecal junction Length = 6 m Diameter = 4 – 2.5 cm. 3SIVA PRAKASH
- 4. Site :it occupies all abdominal regions except epigastic and hypochondriac region normally Fixation :it is stabilized by mesentery Mesentery = peritoneal fold attaching small intestine to posterior body wall 4SIVA PRAKASH
- 5. Anatomical subdivisions : a) Duodenum b) Jejunum c) Ileum 5SIVA PRAKASH
- 6. Duodenum: C-shaped tube 25 cm long & width 3.75-4 cm Joins stomach to jejunum The first & shortest part of small intestine The widest & most fixed part Curves around the head of pancreas Begins at pylorus on right side & ends at duodenojejunal junction on left side Partially retroperitoneal 6SIVA PRAKASH
- 7. Duodenum is divided into four parts : a) First (superior) part b) Second (descending) part c) Third (horizontal) part d) Forth (ascending) part First part of duodenum It is 5 cm long Lies antiero-lateral to body of L1 vertebrae Most movable part 7SIVA PRAKASH
- 8. Duodenum Second part: It is 8 to 10 cm long Descends along right sides of L1 through L3 vertebrae Third part : It is 10 cm long Crosses L3 vertebra Fourth part of duodenum Ascending It is 2.5 cm long Begins at left of L3 & rises superiorly as far as superior border of L2 and continues with jejunum 8SIVA PRAKASH
- 9. JEJUNUM & ILEUM Jejunum begins at duodenojejunal flexure (L2) & ileum ends at ileocecalJunction. Jejunum & ileum = 6 to 7 m long (jejunum 2/5, ileum 3/5) Coils of jejunum & ileum are suspended by mesentery from posterior abdominal wall & freely movable. Most jejunum lies in leftupper quadrant & most ileum lies in right lower quadrant 9SIVA PRAKASH
- 10. Wall of small intestine is made of the following layers : a) Serosa coat b) Muscular coat c) Submucosa coat d) Mucosa coat Serosa: made of peritoneum Muscularis: made of smooth muscle fibers arranged in outer longitudinal & inner circular layers Submucosa : contains loose CT & large venous plexuses (submucosa of duodenum contains duodenal or Brunner’s glands) Mucosa composed of a layer of epithelium, lamina propria & muscularis mucosa (Plicae circulares numerous in jejunum, Peyer’spatches present in ileum) 10SIVA PRAKASH
- 11. 11SIVA PRAKASH
- 12. Barium Techniques Indirect Small bowel follow through.... Dedicated small bowel follow through... Peroral pneumocolon..... Retrograde small bowel .... Direct Enteroclysis... 12SIVA PRAKASH
- 13. Indication Abdominal pain and diarrhoea Small bowel obstruction Crohn’s disease Nasogastric tube/failed intubation Malabsorption Anaemia/gastrointestinal bleeding Abdominal mass 13SIVA PRAKASH
- 14. Contraindications Colonic obstruction Suspected perforation Paralytic ileus 14SIVA PRAKASH
- 15. Contrast media Medium density barium suspension (50-60%w/v) Suspending agent to prevent flocculation and maintain stability High density barium(200-250%) may produce an appearance of fold thickening and clumping of small bowel 15SIVA PRAKASH
- 16. Acid Baso4 suspension may produce spasm, enlarged folds and dilatation of duodenum & jejunum Alkaline Baso4 suspension improves coating of valvulae and improves diagnostic accuracy It is usually mixture of any flavour 16SIVA PRAKASH
- 17. Why barium usedIt is an insoluble material It is high atomic no:56 It is high density, It provides a positive contrast in x-ray It is radiopaque material Is not absorbed or metabolized Is eliminated intact from the body Alkaline BaSO4 suspension improve coating valvulae 17SIVA PRAKASH
- 18. Why iodine is not used Is water soluble Diminish blood volume 18SIVA PRAKASH
- 19. Preparation Purgative- Dulcolax 2tab HS (not in suspected obstruction, acute crohn’s exacerbation, ileostomy) Low roughage high fluid intake diet 48hrs prior No food/fluid should be taken for 12hrs before investigation No antispasmodics, codeine, tranquilizers 24-48hrs prior 19SIVA PRAKASH
- 20. Barium follow-through examination This is performed following a barium meal examination of the esophagus, stomach and duodenum 150ml 250%w/v—200ml 20-25%--250ml40-45% As the barium column progresses through the small intestine large radiographs of the abdomen are taken at intervals First one is taken with the patient supine about 15 minutes after the barium meal and shows the proximal jejunum 20SIVA PRAKASH
- 21. The remaining radiographs are normally taken at half hourly intervals with the patient prone. When the barium column reaches the caecum spot views of the terminal ileum are taken It takes from 2 to 6 hours for the head of the barium column to reach the caecum 21SIVA PRAKASH
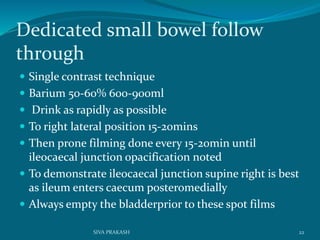
- 22. Dedicated small bowel follow through Single contrast technique Barium 50-60% 600-900ml Drink as rapidly as possible To right lateral position 15-20mins Then prone filming done every 15-20min until ileocaecal junction opacification noted To demonstrate ileocaecal junction supine right is best as ileum enters caecum posteromedially Always empty the bladderprior to these spot films 22SIVA PRAKASH
- 23. Single contrast technique Positioning Purpose First Right side down dependent To aid gastric emptying Second Prone To separate bowel loops Third Right side up To visualize IC junction 23SIVA PRAKASH
- 24. Periodic fluoroscopic examination and compression spot films are recommended 4 spot films for ileocaecal junction should be taken with variable degree of compression Compression over bowel loops to avoid overlap thereby prevents efffacemen of mucosa and small lesions may not be missed The abnormality must be shown in 2 spot films taken at different times to confirm persistence of lesion 24SIVA PRAKASH
- 25. Overlap of contrast filled bowel loops in pelvis Overcome by Table head down 30 degree caudal angled view of pelvis Emptying urinary bladder prior to filming ileal loops Peristalsis can be increased by Metoclopromide, Neostigmine , Cholecystokinin, glucagon 20-40ml sodium/meglumine diatrizoate or gastrograffin to barium increases transit time Cold water- barium more palatable ,speeds gastric emptying 25SIVA PRAKASH
- 26. Interpretation Jejunum Ileum Constitutes proximal 2/5th of small intestine 3/5th Position Upper left and periumblical region Lower right hypogastric and pelvic region Max. diameter 4 cm 3 cm Number of folds 4-7 per cm 3-5 per cm Pattern Feathery mucosa Less feathery or maybe absent Fold thickness 1.5-2mm bowel wall depth 1-1.5mm 26SIVA PRAKASH
- 27. BA Meal follow through: 28SIVA PRAKASH
- 28. 29SIVA PRAKASH
- 29. The pattern of the mucosal lining of the first part of the duodenum is different from the other parts. longitudinal pattern of the mucosa of the first part of the duodenum forming what is known as the duodenal cap This pattern is very similar to that of thepylorus of the stomach This pattern changes to a more flecked appearence in the distal duodenum 30SIVA PRAKASH
- 30. 31SIVA PRAKASH
- 31. Reflux examination Barium and air refluxed through the ileocaecal valve during a barium enema examination give good views the terminal ileum. Replaced by enteroclysis The radiographs should be studied carefully and spot views of the distal ileum is taken if necessary All of the small intestine can be examined by refluxing barium from the colon into the terminal ileum – the complete reflux examination 32SIVA PRAKASH
- 32. doublecontrast barium enema examination (with reflux into terminal ileum) shows carcinoid tumor in terminal ileum Doublecontrast barium enema examination (with reflux into terminal ileum) shows lipoma as smooth, ovoid, submucosal mass in distal ileum 33SIVA PRAKASH
- 33. Peroral Pneumocolon examination Excellent view of the terminal ileum and caecum can be obtained by giving barium orally and when the head of the barium column has reached the ascending colon introducing air per rectum and refluxed in to distal ileum Glucagon can be used to relax ileocaecal valve This procedure shows Crohn’s disease and carcinoma of the caecum particularly well 34SIVA PRAKASH
- 34. Per oral pneumocolon examination Indications contraindicatns Terminal ileum porly visualized on routine compresion spot films . Clinical suspicon of Crohn disease with normal apearance of terminal ileum abnormal apearance of terminal ileum on routine compresion spot films history ileocolic anastomosis. Recent colonic or rectal biopsy 35SIVA PRAKASH
- 35. 36SIVA PRAKASH
- 36. Advantages Disadvantages Easily performed No catheterisation Physiologic transit time can be assessed Overlapping of barium filled bowel loops in pelvis Poor distension Partial or intermittent bowel obstruction Operator dependant Time consuming 38SIVA PRAKASH
- 37. Complicaions Leakage of barium form unsuspected perforation Aspiration Impacted barium converts partial obstruction in to complete obstrction Barium appendicitis impaction at appx 39SIVA PRAKASH
- 38. 40SIVA PRAKASH