Surgical infections
- 1. SURGICAL INFECTION Neil Mendoza, MD, FPSGS, FPCS
- 2. Factors that Increase the Number of Serious Surgical Infection Performance of more complicated and longer operations Increase in the number of geriatric patients Use of implants Use of immunosuppressive agents
- 3. Factors that Increase the Number of Serious Surgical Infection Utilization of diagnostic and treatment modalities Laxity of aseptic technique Disregard for established surgical principles Unwarranted reliance upon prophylactic antibiotic therapy
- 4. Classification Of Surgical Infections I. Relative to Final Outcome Self limiting infections Serious infection Fulminant infection (fatal or permanently disabling)
- 5. Classification Of Surgical Infections II. Relative to Time of Onset Pre-operative surgical infection Operative surgical infection a. Preventable operative surgical infection b. Non-preventable operative surgical infection Post-operative surgical infection (UTI, Respiratory, Wound)
- 6. Determinants Of Infection A. Microbial Pathogenicity: Virulence (tissue invading powers) Infecting dose (10 5 ) Ability to produce toxins (exotoxins / endotoxins) Ability to resist phagocytosis and intracellular destruction
- 7. B. Host Defenses: 1. Local Host defenses: Layers of epithelium Local environment features Skin lack moisture Flushing action of tears & urine Cilia, peristalsis, mucus, pH Local immunity IgA
- 8. B. Host Defenses: 2. Systemic Host defenses: Decrease delivery of phagocytes Diminution in blood flow Presence of devitalized tissue, foreign bodies, hematomas and seroma Decrease vascular reactivity (uremic, old age, high dose of steroid) Decrease production of phagocytes (chemotherapy)
- 9. 2. Systemic Host defenses: Abnormal serum factors (opsonins) Specific antibody and complement act as a strong opsonizing agents for phagocytosis of containing bacteria. Abnormal ingestion & intracellular killing of Phagocytes Seen in uremia, ketosis, hyperglycemia, malignancies, severe thermal or traumatic injury, malnutrition, immunosuppres sed
- 10. c. Surgical technique: Handle tissues gently Remove devitalized tissues, blood Using drains Avoid excessive cautery (-) tension in intestinal anastomosis Good blood supply
- 11. Prevention Of Infection A. Avoidance of Predisposing Conditions 1. Bacterial Contamination: Minimize contamination ----> strict aseptic technique 2 great sources of microbial contamination Exogenous contact from breaks in technique by the team Endogenous contamination from patient’s skin and various bacteria-containing tracts.
- 12. Classification Of Surgical Wounds According to Risk of Infection a. CLEAN WOUND (I): 1.5 – 5.4% infection rates Elective cases, primarily closed and undrained Nontraumatic, uninfected, no inflammation No break in asepsis Respiratory, alimentary, genitourinary or oropharyngeal tracts not entered Hernia repair, breast biopsy
- 13. B. CLEAN – CONTAMINATED WOUND: 2.1 – 9.5% infection rate Alimentary, respiratory, genito-urinary tract entered under controlled conditions and w/o unusual contamination Minor break in technique Mechanical drainage Appendectomy, biliary tract
- 14. C. CONTAMINATED WOUND 3.4 – 13.2% infection rates Open, fresh traumatic wound Gross spillage from gastrointestinal tract Entrance of genitourinary or biliary tracts in presence of infected urine and bile Major break in technique Penetrating abdominal trauma, large tissue injury, enterotomy during bowel obstruction
- 15. D. DIRTY AND INFECTED WOUND 28 – 40% infection rates Traumatic wound with retained devitalized tissue, foreign bodies, fecal contamination or delayed treatment Perforated viscus encountered Acute bacterial inflammation with pus encountered during operation
- 16. Prophylaxis: Prevent Wound Infections 1. Avoidance of Bacterial Contamination: a) Environmental factors Avoid exogenous and endogenous contamination Use of ultraviolet light and laminar flow ventilation Limitation of traffic in and out of the operating room Limitation of activity and talking within the operating room
- 17. b) Pre-operative preparations of the patient Pre-operative shower w/ antimicrobial soap (chlorhexidine) Cutaneous infection should be controlled or cleared before elective operation
- 18. Hair removal promotes bacterial growth to 100% if the blade cuts the skin Seropian & Reynolds study 406 clean wounds showed that shaving increases infection rate to 5.6% from 0.6% where no shaving was done
- 19. c.) Skin preparation Scrub the operative area for 5 to 7 mins. germicidal solution and paint w/ povidine-iodine or chlorhexidine Use an antimicrobial incision drape Operating Room Team and Discipline Wear clean scrab suits, cap and mask Scrub hands and forearms w/ antimicrobial soap Careful wearing of gowns and gloves Change puncture or tear gloves
- 20. Operating Room Team and Discipline Wear clean scrab suits, cap and mask Scrub hands and forearms w/ antimicrobial soap Careful wearing of gowns and gloves Change puncture or tear gloves
- 21. 3. Endogenous Contamination Avoid bacterial contamination of the surgical wound at the time of transection of the GIT, GUT and respiratory tract
- 22. 4. Importance of Surgical Technique Gentle care of the tissues to minimized local damaged All devitalized tissue and foreign bodies should be removed Use monofilament sutures for potentially infected wound Avoid the presence of hematomas, seromas and dead spaces Role of delayed primary closure (tertiary wound healing)
- 23. 5. Systemic Factors: Host resistance (control systemic diseases) Correct malnutrition Avoid disturbance of circulation Avoid unnecessary used of drugs
- 24. 6. Systemic Prophylactic Chemotherapeutic and Antibiotic: Avoid indiscriminate used of antibiotics because: Secondary infection or superimposed infection Hypersensitivity reaction May mask signs and symptoms of infection Development of antibiotic resistant strains
- 25. 7. Reduction of Colonic Bacteria (Intestinal Antisepsis) reduce the high rate of infectious complication after colorectal surgery Combined w/ mechanical cleansing of the colon Ideal drugs: Bactericidal Minimillay absorbed No side effect
- 26. Types: a. 3 day bowel preparation b. Nichols-Condon Method 2 days fluid diet, mechanical Oral methronidazole and erythromycin 1gm each 1 gm give 1, 2 qnd 11 PM c. Whole GUT irrigation w/ polyethylene-glycol-electrolyte lavage (GOLYTELY) 1 L ---> 5hrs w/o = wound infection 48% w/ = wound infection 20%
- 27. 8. Prophylactic Antibiotics: Given IV 30 – 60 mins before operation so that adequate blood and tissue levels are present at the time that the skin incision is made Another dose given if operating time is > 4hrs and other dose given w/in 24 hrs.
- 28. Prophylactic Antibiotics: Principles: Choose antibiotic effective against pathogens most likely to be encountered Low toxicity Administer a single full therapeutic dose. 2 nd dose given postoperatively Utilization of host defenses to augment antimicrobial effect of the antibiotics
- 29. Prevention Of Infection Avoidance of Predisposing Conditions Immunotherapy: Specific immunotherapy in the practice of surgery is limited to the administration of antitoxins against: TETANUS RABIES SNAKE BITE
- 30. Surgical Site Infections SSIs are infections of the tissues, organs, or spaces exposed by surgeons during performance of an invasive procedure. SSIs are classified into Incisional: superficial (limited to skin and subcutaneous tissue) deep incisional categories Organ/space infections
- 31. Factors: 1. The degree of microbial contamination of the wound during surgery 2. The duration of the procedure 3. Host factors such as diabetes, malnutrition, obesity, immune suppression, and a number of other underlying disease states.
- 32. Risk Factors for Development of Surgical Site Infections A. Patient factors Older age Immunosuppression Obesity Diabetes mellitus Chronic inflammatory process Malnutrition 7. Peripheral vascular disease 8. Anemia 9. Radiation 10. Chronic skin disease 11. Carrier state (e.g., chronic Staphylococcus carriage) 12.Recent operation
- 33. Risk Factors for Development of Surgical Site Infections Local factors Poor skin preparation Contamination of instruments Inadequate antibiotic prophylaxis Prolonged procedure Local tissue necrosis Hypoxia, hypothermia
- 34. Risk Factors for Development of Surgical Site Infections C. Microbial factors Prolonged hospitalization (leading to nosocomial organisms) Toxin secretion Resistance to clearance (e.g., capsule formation)
- 35. Surgical management of the wound In healthy individuals, class I and II wounds may be closed primarily , while skin closure of class III and IV wounds is associated with high rates of incisional SSIs (25 to 50%). Class III and IV wounds should be packed open and allowed to heal by secondary intention , although selective use of delayed primary closure has been associated with a reduction in incisional SSI rates.
- 36. Surgical management of the wound Increased SSI rates being associated with hyperglycemia It is recommended that clinicians maintain appropriate blood sugar control in diabetic patients in the peri-operative period to minimize the occurrence of SSIs.
- 37. ANTIBIOTICS A chemical cpd. derived from or produced by living organisms capable at low concentration of inhibiting the life process of the microorganisms
- 38. ANTIBIOTICS Classification: Bacteriostatic: prevent the growth of bacteria but do not destroy them. Affects early stages of protein synthesis in the ribosome Bactericidal: Agents that actively kill the bacteria It causes the ribosome to miscode and consequently induced the manufacture of defective proteins and enzymes that poison the cell
- 39. Antibiotic Mode of Action Cellular site of inhibition Bactericidal Bacteriostatic 1. Cell wall synthesis Penicillin Cephalosphorin Vancomysin Bacitracin 2. Barrier function of cell membrane Polymyxin B Colistin Amphotericin B Nystatin
- 40. Antibiotic Mode of Action Cellular site of inhibition Bactericidal Bacteriostatic 3. Protein synthesis in the ribosome Streptomycin aminoglycoside Tetracyclin Chloramphenicol Erythromycin Clindamycin 4. DNA replication in chromosome griseogulvin
- 41. Antibiotic Agents 1. Penicillin blocks the synthesis of the bacterial wall ---> osmotic instability & lysis Active against most gram (+) bacteria 2. Cephalosphorin Bactericidal by inhibiting bacterial cell wall synthesis Arranged into generation For gram (+) and (-) bacteria
- 42. Antibiotic Agents 3.Erythromycin Bacteriostatic ; bactericidal in higher dose Inhibit bacterial protein synthesis Treatment of choice in treating mycoplasm and Legionnaire’s disease, also for actinomycosis
- 43. Antibiotic Agents 4. Tetracyclines For gram (+) and (-) not sensitive to penicillin Good for TB Bacteriostatic Interfere w/ protein synthesis For actinomycosis and nocardiosis Should be avoided in early childhood causing yellow discoloration of the teeth
- 44. Antibiotic Agents 5. Chloramphenicol Broad spectrum and bacteriostatic Inhibits protein synthesis Well absorbed orally and parenterally Drug of choice in typhoid fever and other salmonella infection Good for meningitis and H. influenzae
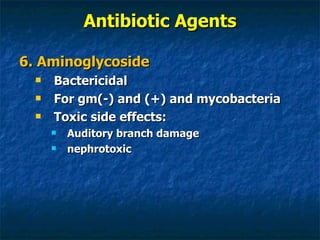
- 45. Antibiotic Agents 6. Aminoglycoside Bactericidal For gm(-) and (+) and mycobacteria Toxic side effects: Auditory branch damage nephrotoxic
- 46. Antibiotic Agents 7. Metronidazole Bactericidal Important for obligate anaerobic bacteria 8. Amphotericin B Good for antifungal agents IV, intrathecally or instilled directly to the site of infection
- 47. Antibiotic Agents 9. Sulfonamides - Trimethoprim Effective against community acquired gm (-) Orally administered Has limited usefulnes in nosocomial infection 10. 4-Fluoroquinolones Good for nosocomial infections Good activity against nearly all gram (-) organism
- 48. Antibiotic Agents 11. Carbapenems Has the widest spectrum Highly effective against most aerobic (S. aureus & P. aeruginosa) as well as anaerobic bacteria
- 49. Diagnosis and Treatment of Surgical Infection The most important part of the evaluation of pt. suspected of having a surgical infection is careful history and PE Laboratory and radiological technique: Urinalysis, CBC, blood culture and sensitivity Ultrasonography / CT scan / MRI
- 50. Diagnosis and Treatment of Surgical Infection If w/ Pus (color, Odor and Consistency) Foul odor - Anaerobic Greenish - P. aeruginosa Creamy - S. aureus Thin watery - Strep / clostridium
- 51. Surgical Intervention Primary principle of surgical treatment of surgical infection are: Incision and drain of localized abscess Adequate debridement of necrotic tisue Removal of all hematomas, seroma and foreign bodies If with dead space ---> put sterile close suction tube
- 52. Types of Surgical Infections Soft Tissue Infections: Cellulitis, Erysipelas, Lymhangitis Erythema, local pain & tenderness, edema Fever, chills, malaise and toxic reaction Pathogens: S. pyogenes S. aureus S. pneumoniae H. influenzae Aerobic and anaerobic gram (-) Tx: - antibiotic, immobilization / elevation and hygiene
- 53. Types of Surgical Infections Soft Tissue Infections: Cellulitis, Erysipelas, Lymhangitis
- 54. Types of Surgical Infections Soft Tissue Infections: Soft tissue abscess Furunculosis, felon, carbuncle Tx: - incision and drainage - antibiotic - hygiene and nutrition
- 55. Carbuncle
- 56. Types of Surgical Infections Soft Tissue Infections: Necrotizing Soft Tissue Infections: Necrotizing fascitis, strep. Gangrene, gas gangrene, bacterial synergistic gangrene, clostridium myonecrosis and Fournier’s gangrene Mixed aerobic and anaerobic gram negative and gram positive bacteria as well as fungi
- 57. Patients at risk; elderly, immunosuppressed, or diabetic; peripheral vascular disease; or those with a combination of these factors. common among these host factors: compromise of the fascial blood supply to some degree, coupled with the introduction of exogenous microbes most commonly affected: extremities, perineum, trunk, and torso
- 59. Manifestations: 1. small break or sinus in the skin from which grayish, turbid semipurulent material ("dishwater pus") can be expressed 2. skin changes (bronze hue or brawny induration), blebs, or crepitus 3. pain at the site of infection that appears to be out of proportion to any of the physical manifestations 4. sepsis syndrome or septic shock
- 60. Treatment: Debridement of all necrotic tissue (amputation) Reconstruction done once infection is controlled
- 61. Treatment: Antimicrobial agents directed against gram-positive and gram-negative aerobes and anaerobes (e.g., vancomycin plus a carbapenem), as well as high-dose aqueous penicillin G (16,000 to 20,000 U/d for clostridial pathogens Antibiotic therapy can be refined based on culture and sensitivity results, particularly in the case of monomicrobial soft tissue infections.
- 62. D. Tetanus Clostridium tetany: Tetanospasm – acts on the anterior horn cells of spinal cord and brain stem by blocking the inhibitor synapses Tetanolysin - cardiotoxic and hemolysis Sx: Restlessness , headache, stiff neck, difficulty of swallowing Orthotonus, opisthotonus, convulsion
- 63. Tetanus Tx: Tetanus immune globulin (TIG) 500 to 10,000 units and tetanus toxoid Intensive unit: - sedation, respirator if needed, good nursing care, quite room Wound debridement Penicillin G Na Muscle relaxant, analgesic, adequate nutrition, laxatives, pressure sore precautions, eye protection
- 64. II. Body Cavity Infections: Peritonitis and Intra-abdominal abscess Primary peritonitis Single organism, in children and adult microbes invade the normally sterile confines of the peritoneal cavity via hematogenous dissemination from a distant source of infection or direct inoculation more common among patients with ascites and individuals being treated for renal failure via peritoneal dialysis Tx: antibiotic
- 65. Primary peritonitis Diagnosis is established based on identification of risk factors a. physical examination: diffuse tenderness and guarding without localized findings b. absence of pneumoperitoneum on abdominal flat plate and upright roentgenograms c. more than 100 WBCs/mL, and microbes with a single morphology on Gram's stain performed on fluid obtained via paracentesis
- 66. Primary peritonitis Treatment : a. Administration of an antibiotic to which the organism is sensitive; often 14 to 21 days of therapy are required. b. Removal of indwelling devices (e.g., peritoneal dialysis catheter or peritoneovenous shunt) may be required for effective therapy of recurrent infections.
- 67. 2. Secondary bacterial peritonitis secondary to perforation or rupture of a hollow viscus Ruptured AP, perforated duodenal ulcer, complicated diverticular disease, etc
- 68. Secondary bacterial peritonitis combination of antibiotic agents or single agents with a broad spectrum of activity can be used conversion of a parenteral to an oral regimen only when the patient's ileus resolves Effective source control and antibiotic therapy is associated with low failure rates and a mortality rate of approximately 5 to 6%; inability to control the source of infection leads to mortality greater than 40%.
- 69. Secondary bacterial peritonitis Treatment: surgical intervention and antibiotic effective therapy requires source control: remove the diseased organ débridement of necrotic, infected tissue and debris administration of antimicrobial agents directed against aerobes and anaerobes
- 70. Secondary bacterial peritonitis Diagnosis & Treatment: computed tomographic (CT) scan- best percutaneous drainage under imaging Surgical intervention: Multiple abscesses Abscesses in proximity to vital structures such that percutaneous drainage would be hazardous, and Those in whom an ongoing source of contamination (e.g., enteric leak) is identified.
- 71. Secondary bacterial peritonitis Treatment: antibiotics with aerobic and anaerobic activity drainage catheter in situ until: it is clear that cavity collapse has occurred, output is less than 10 to 20 mL/d, no evidence of an ongoing source of contamination is present patient's clinical condition has improved.
- 72. 3. Tertiary peritonitis poorly understood more common in immunosuppressed patients in whom peritoneal host defenses do not effectively clear or sequester the initial secondary microbial peritoneal infection associated with mortality rates in excess of 50%
- 73. Types of Surgical Infections III. Prosthetic Device – Associated Infections Frequently eradicated after removal of the foreign body IV. Hospital – Acquired Infection Wound infection Urinary tract infection (most common) Lower respiratory tract infection Vascular catheter-related infection
- 74. NOSOCOMIAL INFECTION related to prolonged use of indwelling tubes and catheters for the purpose of urinary drainage, ventilation, and venous and arterial access, respectively. a. UTI: Treatment for 10 to 14 days with a single antibiotic. indwelling urinary catheters removed as quickly as possible
- 75. b. Mechanical Ventilator: associated with an increased incidence of pneumonia Diagnosis: X-ray evidence of one or more areas of pulmonary consolidation. broncho-alveolar lavage to obtain samples; Gram's stain & culture to assess for the presence of microbes. Surgical patients should be weaned from mechanical ventilation as soon as feasible, based on oxygenation and inspiratory effort.
- 76. c. Intravascular catheter: Increase the risk of infection Prolonged insertion Insertion under emergency conditions Manipulation under nonsterile conditions use of multilumen catheters
- 77. ASEPSIS and ANTISEPSIS
- 78. Surgical Asepsis: Prevention of the access of microorganisms to an operative wound Destroy and remove bacteria and other pathogens from all objects coming in contact with the wound NEW: Surgical isolators cemented to operative site Use of laminar flow
- 79. TERMS 1. Antiseptic: Chemical agents that either kills or inhibits the growth of bacteria and applied to human tissues 2. Disinfectant: Germicidals applied to inanimate objects 3. Sterilization: A process of killing all microorganism
- 80. ASEPTIC TECHNIQUE Hygienic hand washing Pre-operative preparation of the patient’s skin Use of sterile gloves and gown as well as application of sterile drapes to operative sites Isolation precaution Sterilization, with autoclave or other method, of instrument that will be used. Proper waste disposal
- 81. OPERATING ROOM Ideally, free from bacterial contamination 20 x 20 ft recommended size Area for gowning of operative team Room for additional materials needed Appropriate ventilation: Laminar flow (ideal) Air passes through a filter that efficiently removes bacteria and fungi but not viruses Doors should remain closed except as needed Pressure in the OR should be positive relative to outside Minimize personnel inside the room
- 82. PATIENT The most common source of contamination in the OR Preparation of patient’s skin: Preoperative showering Hair removal, only at operative sites, done in the OR Application of antiseptic (Povidone iodine – active to bacteria, fungi and viruses) to patient’s skin Application of sterile drapes
- 83. PATIENT Factors associated w/ increased infection rates: Age Obesity Diabetes mellitus Cirrhosis Uremia Connective tissue disorders Hereditary or induced immunodeficiency state Nutrition
- 84. OR Team Minimize the number of people inside the room Proper scrubbing and attire Sterile gloves and gown Gloves protect the patient from the hands of the surgeon Gloves protect the doctor from contaminated blood/body fluids Punctured gloves: 50-70% frequency Non-dominant index finger is the most common site of perforation 90% of perforation if surgery last for > 2 hrs.
- 85. OR Team 3. Sterile gloves and gown Ideal gown: Should be impermeable to moisture 1. Single layer gown --> < 2hrs operation or <100 ml of blood 2. Reinforced gown --> 2-4 hrs or 100-500ml of blood 3. Plastic reinforced --> > 4hrs or > 500ml of blood loss
- 86. STERILIZATION Steam Under Pressure (Autoclave) Most reliable, power of penetration, easy to control and economical Steam---->Condense----> Produce heat 15psi for 15 to 45 min = 121 C
- 87. 2. Dry Heat Sterilization: Used for: a. glassware b. talc, vaseline, fats and oils Bake the material in hot air oven 121 C (250 F) = 6 hrs. 170 C (340 F) = 1 hr.
- 88. 3. Gas Sterilization: Ethylene oxide Uses a chamber where temp and humidity is controlled and air can be evacuated 3 – 6 hrs Use: (for delicate instruments) – optical lenses, tubings and plastic parts of heart-lung machine and respirators
- 89. STERILIZATION 4. Radiation Sterilization: Cobalt 60 For heat sensitive materials (drugs) 5. Chemical Sterilization: 2% glutaraldehyde ----> cidex / sonacide Bactericidal, sporocidal and virucidal
- 90. De-germing the Skin Antiseptics are also admixed with soap Vigorous scrubbing with soap containing: 1. Hexachlorophene 2. Iodophors 3. Chlorhexidine gluconate
- 91. 1. Hexachlorophene Bisphenol Gm (+) organism but not for Gm (-) bacteria Side effect: Vacuolar encephalopathy teratogenic
- 92. 3. Iodophores: 1% iodine – iodine is liberated when the compound is diluted with water For gm (+) and (-) but not for spores
- 93. 3. Chlorhexidine Gluconate: For gm (+), (-) and fungi Sporicidal at elevated temperature This plus 4% isopropanolol -----> surgical hand scrub and skin preparation
- 94. end