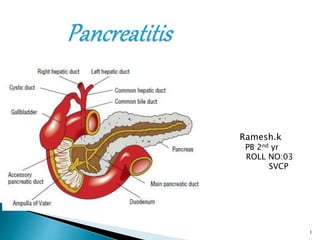
Acute pancreatitis
- 1. Ramesh.k PB 2nd yr ROLL NO:03 SVCP 1
- 2. Sudden onset of unrelenting upper abdominal pain resulting from inflammation of the pancreas Patients commonly present to ER due to severe abdominal pain Requires admission to the hospital for medical management 2
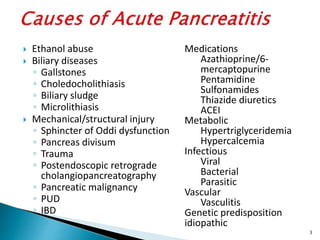
- 3. Ethanol abuse Biliary diseases ◦ Gallstones ◦ Choledocholithiasis ◦ Biliary sludge ◦ Microlithiasis Mechanical/structural injury ◦ Sphincter of Oddi dysfunction ◦ Pancreas divisum ◦ Trauma ◦ Postendoscopic retrograde cholangiopancreatography ◦ Pancreatic malignancy ◦ PUD ◦ IBD Medications Azathioprine/6- mercaptopurine Pentamidine Sulfonamides Thiazide diuretics ACEI Metabolic Hypertriglyceridemia Hypercalcemia Infectious Viral Bacterial Parasitic Vascular Vasculitis Genetic predisposition idiopathic 3
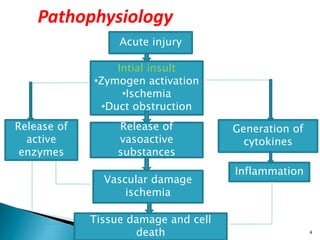
- 4. Initial insult •Zymogen activation •Ischemia •Duct obstruction Acute injury Intial insult •Zymogen activation •Ischemia •Duct obstruction Release of active enzymes Release of vasoactive substances Generation of cytokines Inflammation Vascular damage ischemia Tissue damage and cell death Pathophysiology 4
- 5. Pulmonary ◦ Atelactasis ◦ Pleural effusions Cardiovascular ◦ Cardiogenic shock Neurologic ◦ Pancreatic encephalopathy Metabolic ◦ Metabolic acidosis ◦ Hypocalcemia ◦ Altered glucose metabolism Hematologic ◦ GI bleeding Renal ◦ Prerenal failure 5
- 6. Upper abdominal pain rapidly increasing in severity, often within 60 minutes Epigastric pain Right-sided pain Diffuse abdominal pain with radiation to back Pain rarely only in left upper quadrant Restless Prefer to sit and lean N/V Fever Tachycardia 6
- 7. Decreased or absent bowel sounds Abdominal tenderness Guarding Palpable mass in epigastric area Biliary colic Jaundice if there’s obstruction of the bile duct Cullen’s sign Grey Turner’s Sign 7
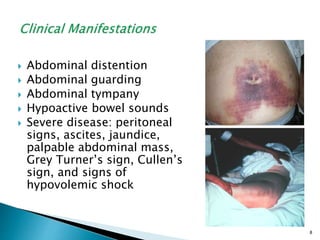
- 8. Abdominal distention Abdominal guarding Abdominal tympany Hypoactive bowel sounds Severe disease: peritoneal signs, ascites, jaundice, palpable abdominal mass, Grey Turner’s sign, Cullen’s sign, and signs of hypovolemic shock 8
- 9. Patient’s history Physical examination Diagnostic findings ◦ Serum amylase levels greater than three times the upper limit ◦ Serum amylase levels may be normal in patients with pancreatitis related to alcohol abuse or hypertriglyceridemia ◦ Levels greater than five times the top normal value should be expected in patients with renal failure because amylase is cleared by the kidneys 9
- 10. Plain abdominal x-rays for visualizing gallstones or a gas-filled transverse colon ending at the area of pancreatic inflammation ◦ colon cut-off sign Abdominal ultrasound ◦ Cholelithiasis, biliary sludge, bile duct dilation, and pseudocysts CT of abdomen MRCP (magnetic resonance cholangiopancreatography) 10
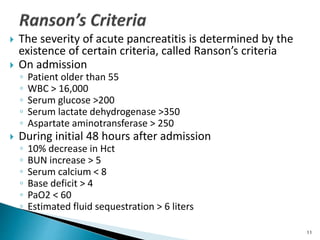
- 11. The severity of acute pancreatitis is determined by the existence of certain criteria, called Ranson’s criteria On admission ◦ Patient older than 55 ◦ WBC > 16,000 ◦ Serum glucose >200 ◦ Serum lactate dehydrogenase >350 ◦ Aspartate aminotransferase > 250 During initial 48 hours after admission ◦ 10% decrease in Hct ◦ BUN increase > 5 ◦ Serum calcium < 8 ◦ Base deficit > 4 ◦ PaO2 < 60 ◦ Estimated fluid sequestration > 6 liters 11
- 12. Fluid Management Nutritional support ◦ Rest gut ◦ TPN Pain management Supporting other organ systems 12
- 13. IV replacement of fluids, proteins, and electrolytes Fluid volume replacement and blood transfusions Withholding food and fluids to rest the pancreas NG tube suctioning Peritoneal lavage Surgical drainage Laparotomy to remove obstruction 13
- 14. General approach: Initial treatment usually involves withholding foods or liquids . Nasogastric aspiration Aggressive fluid resucitation Intravenous colloids Drotrecogin alfa Insulin 14
- 15. Nonpharmacologic therapy: Nutritional therapy. Pharmacologic therapy: Relief of abdominal pain Analgesics:-pethidine,morphine Prevention of infection Antibiotics:-Imipenem+cilastatin, Quinolones+metronidazole Anti emetics:-Ondansetron 15
- 16. 16
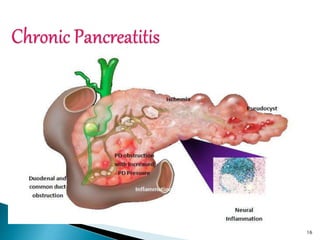
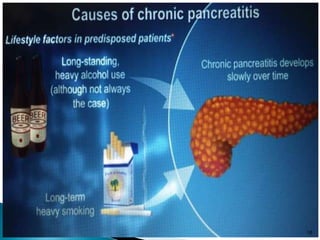
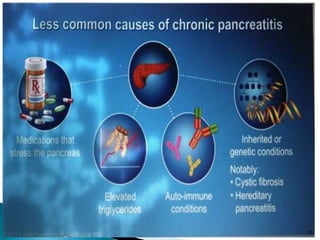
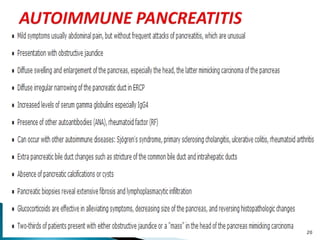
- 17. It is characterised by permanent damage to pancreatic structure and function because of progressive inflammation and long standing pancreatic injury Permanent destruction of pancreatic tissue usually leads to exocrine and endocrine insufficiency. 17
- 18. 18
- 19. 19
- 20. 20
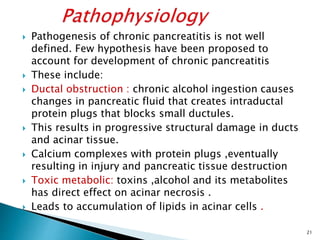
- 21. Pathogenesis of chronic pancreatitis is not well defined. Few hypothesis have been proposed to account for development of chronic pancreatitis These include: Ductal obstruction : chronic alcohol ingestion causes changes in pancreatic fluid that creates intraductal protein plugs that blocks small ductules. This results in progressive structural damage in ducts and acinar tissue. Calcium complexes with protein plugs ,eventually resulting in injury and pancreatic tissue destruction Toxic metabolic: toxins ,alcohol and its metabolites has direct effect on acinar necrosis . Leads to accumulation of lipids in acinar cells . 21
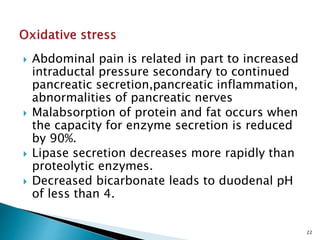
- 22. Abdominal pain is related in part to increased intraductal pressure secondary to continued pancreatic secretion,pancreatic inflammation, abnormalities of pancreatic nerves Malabsorption of protein and fat occurs when the capacity for enzyme secretion is reduced by 90%. Lipase secretion decreases more rapidly than proteolytic enzymes. Decreased bicarbonate leads to duodenal pH of less than 4. 22
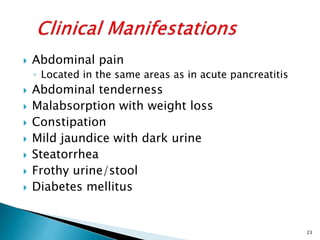
- 23. Abdominal pain ◦ Located in the same areas as in acute pancreatitis Abdominal tenderness Malabsorption with weight loss Constipation Mild jaundice with dark urine Steatorrhea Frothy urine/stool Diabetes mellitus 23
- 24. 24
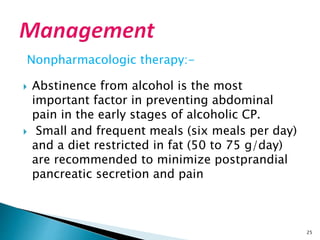
- 25. Nonpharmacologic therapy:- Abstinence from alcohol is the most important factor in preventing abdominal pain in the early stages of alcoholic CP. Small and frequent meals (six meals per day) and a diet restricted in fat (50 to 75 g/day) are recommended to minimize postprandial pancreatic secretion and pain 25
- 26. Treatment of chronic pain: Analgesics Acetaminophen NSAIDS Tramadol Codeine TREATMENT OF MALABSORPTION AND STEATORRHEA Pancreatic enzyme supplements –Amylase, lipase Antisecretory drugs –Somatostatin, octreotide GIT- proton pump inhibitor H2 receptor antagonist SURGERY 26
- 27. Pharmacotherapy, A Pathophysiologic approach by J.T.Dipiro 7 th edition, page.no:659-673 Ross and wilson anatomy and physiology http://gastro.ucsd.edu/Chronic%20Pancreatitis http://www.webmd.com/digestive- disorders/digestive-diseases-pancreatitis 27
- 28. THANK YOU 2 8