Dr.gamal presentation
- 1. Dr. Gamal Said 1 Anatomy of the Female Genital System Clinical Pelvic Anatomy in Cadavers Dr. Gamal Said Workshop
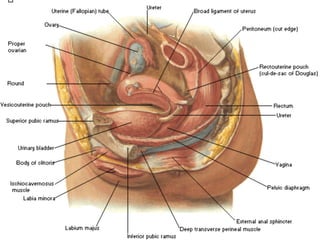
- 2. Dr. Gamal Said 2 Viscera of ♀ genital system Ovary Fallopian tubes Uterus Vagina
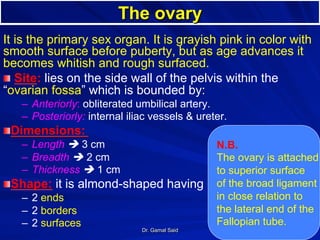
- 3. Dr. Gamal Said 3 The ovary It is the primary sex organ. It is grayish pink in color with smooth surface before puberty, but as age advances it becomes whitish and rough surfaced. ! Site: lies on the side wall of the pelvis within the “ovarian fossa” which is bounded by: – Anteriorly: obliterated umbilical artery. – Posteriorly: internal iliac vessels & ureter. ! Dimensions: – Length è 3 cm – Breadth è 2 cm – Thickness è 1 cm ! Shape: it is almond-shaped having – 2 ends – 2 borders – 2 surfaces N.B. The ovary is attached to superior surface of the broad ligament in close relation to the lateral end of the Fallopian tube.
- 4. Dr. Gamal Said 4
- 5. Dr. Gamal Said 5
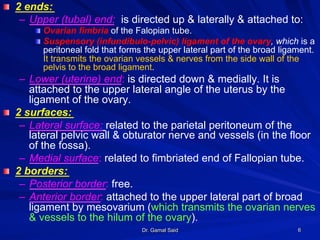
- 6. Dr. Gamal Said 6 ! 2 ends: – Upper (tubal) end: is directed up & laterally & attached to: ! Ovarian fimbria of the Falopian tube. ! Suspensory (infundibulo-pelvic) ligament of the ovary, which is a peritoneal fold that forms the upper lateral part of the broad ligament. It transmits the ovarian vessels & nerves from the side wall of the pelvis to the broad ligament. – Lower (uterine) end: is directed down & medially. It is attached to the upper lateral angle of the uterus by the ligament of the ovary. ! 2 surfaces: – Lateral surface: related to the parietal peritoneum of the lateral pelvic wall & obturator nerve and vessels (in the floor of the fossa). – Medial surface: related to fimbriated end of Fallopian tube. ! 2 borders: – Posterior border: free. – Anterior border: attached to the upper lateral part of broad ligament by mesovarium (which transmits the ovarian nerves & vessels to the hilum of the ovary).
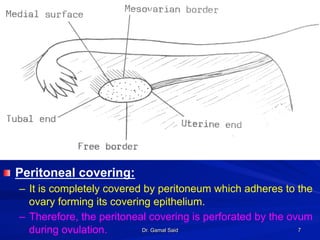
- 7. Dr. Gamal Said 7 ! Peritoneal covering: – It is completely covered by peritoneum which adheres to the ovary forming its covering epithelium. – Therefore, the peritoneal covering is perforated by the ovum during ovulation.
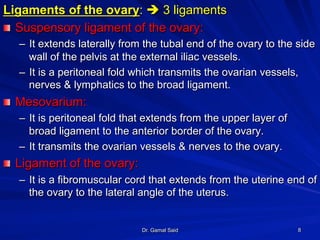
- 8. Dr. Gamal Said 8 Ligaments of the ovary: è 3 ligaments ! Suspensory ligament of the ovary: – It extends laterally from the tubal end of the ovary to the side wall of the pelvis at the external iliac vessels. – It is a peritoneal fold which transmits the ovarian vessels, nerves & lymphatics to the broad ligament. ! Mesovarium: – It is peritoneal fold that extends from the upper layer of broad ligament to the anterior border of the ovary. – It transmits the ovarian vessels & nerves to the ovary. ! Ligament of the ovary: – It is a fibromuscular cord that extends from the uterine end of the ovary to the lateral angle of the uterus.
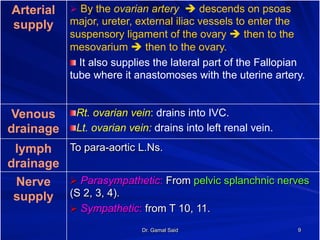
- 9. Dr. Gamal Said 9 Arterial supply Ø By the ovarian artery è descends on psoas major, ureter, external iliac vessels to enter the suspensory ligament of the ovary è then to the mesovarium è then to the ovary. ! It also supplies the lateral part of the Fallopian tube where it anastomoses with the uterine artery. Venous drainage ! Rt. ovarian vein: drains into IVC. ! Lt. ovarian vein: drains into left renal vein. lymph drainage To para-aortic L.Ns. Nerve supply Ø Parasympathetic: From pelvic splanchnic nerves (S 2, 3, 4). Ø Sympathetic: from T 10, 11.
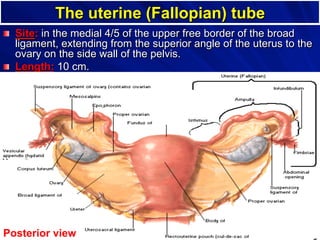
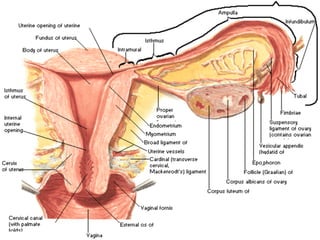
- 10. Dr. Gamal Said 10 The uterine (Fallopian) tube ! Site: in the medial 4/5 of the upper free border of the broad ligament, extending from the superior angle of the uterus to the ovary on the side wall of the pelvis. ! Length: 10 cm. Posterior view
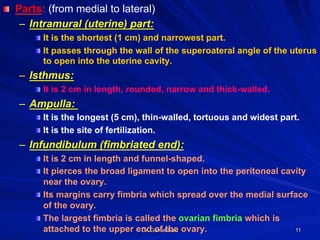
- 11. Dr. Gamal Said 11 ! Parts: (from medial to lateral) – Intramural (uterine) part: ! It is the shortest (1 cm) and narrowest part. ! It passes through the wall of the superoateral angle of the uterus to open into the uterine cavity. – Isthmus: ! It is 2 cm in length, rounded, narrow and thick-walled. – Ampulla: ! It is the longest (5 cm), thin-walled, tortuous and widest part. ! It is the site of fertilization. – Infundibulum (fimbriated end): ! It is 2 cm in length and funnel-shaped. ! It pierces the broad ligament to open into the peritoneal cavity near the ovary. ! Its margins carry fimbria which spread over the medial surface of the ovary. ! The largest fimbria is called the ovarian fimbria which is attached to the upper end of the ovary.
- 12. Dr. Gamal Said 12 ! Course and relations – Each tube runs upwards laterally & backwards from the uterus to the side wall of the pelvis. – Then, it curves backwards piercing the upper layer of the broad ligament to end on the medial surface of the ovary by the infundibulum. – Along its whole course, it is related to coils of ileum & sigmoid colon. ! Blood supply: – Medial 2/3: by the uterine artery. – Lateral 1/3 : by the ovarian artery. ! Venous drainage: – By veins accompanying the arteries into the uterine and ovarian veins. ! Lymph drainage: – Most of the tubal lymphatics pass to the paraaortic L.Ns. – Lymphatics of the isthmus pass to the superficial inguinal L.Ns.
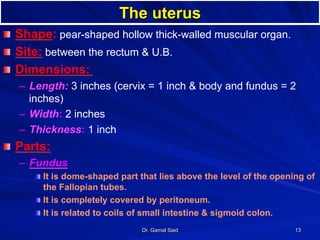
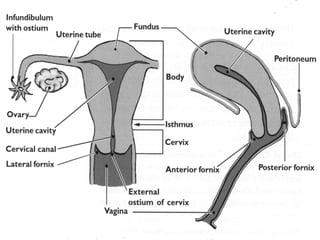
- 13. Dr. Gamal Said 13 The uterus ! Shape: pear-shaped hollow thick-walled muscular organ. ! Site: between the rectum & U.B. ! Dimensions: – Length: 3 inches (cervix = 1 inch & body and fundus = 2 inches) – Width: 2 inches – Thickness: 1 inch ! Parts: – Fundus ! It is dome-shaped part that lies above the level of the opening of the Fallopian tubes. ! It is completely covered by peritoneum. ! It is related to coils of small intestine & sigmoid colon.
- 14. Dr. Gamal Said 14
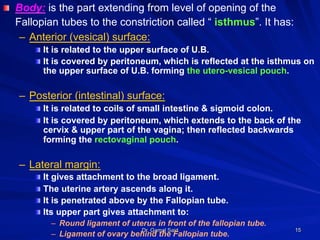
- 15. Dr. Gamal Said 15 ! Body: is the part extending from level of opening of the Fallopian tubes to the constriction called “ isthmus”. It has: – Anterior (vesical) surface: ! It is related to the upper surface of U.B. ! It is covered by peritoneum, which is reflected at the isthmus on the upper surface of U.B. forming the utero-vesical pouch. – Posterior (intestinal) surface: ! It is related to coils of small intestine & sigmoid colon. ! It is covered by peritoneum, which extends to the back of the cervix & upper part of the vagina; then reflected backwards forming the rectovaginal pouch. – Lateral margin: ! It gives attachment to the broad ligament. ! The uterine artery ascends along it. ! It is penetrated above by the Fallopian tube. ! Its upper part gives attachment to: – Round ligament of uterus in front of the fallopian tube. – Ligament of ovary behind the Fallopian tube.
- 16. Dr. Gamal Said 16 ! Isthmus: ! Slight constriction between the body and the cervix. ! Opposite its anterior aspect, the peritoneum is reflected to the U.B. to form the utero-vesical pouch. ! It is covered by peritoneum from the back. ! Cervix: it has supra-vaginal & vaginal parts – Supra-vaginal part: ! Anteriorly: it is not covered by peritoneum and related to the U.B. ! Posteriorly: it is covered by peritoneum of Douglas pouch which separates it from the rectum. ! Laterally: it gives attachment to the broad ligament and is related to the ureter and uterine vessels just below the root of the broad ligament. – Vaginal part: is surrounded by the vaginal fornices.
- 17. Dr. Gamal Said 17
- 18. Dr. Gamal Said 18 Peritoneal covering of the uterus
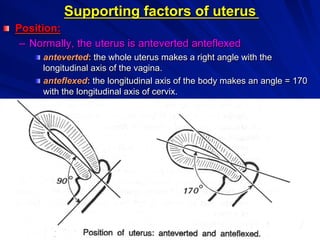
- 19. Dr. Gamal Said 19 Supporting factors of uterus ! Position: – Normally, the uterus is anteverted anteflexed ! anteverted: the whole uterus makes a right angle with the longitudinal axis of the vagina. ! anteflexed: the longitudinal axis of the body makes an angle = 170 with the longitudinal axis of cervix.
- 20. Dr. Gamal Said 20 N.B.: Abnormal position of uterus = retroverted , retroflexed uterus
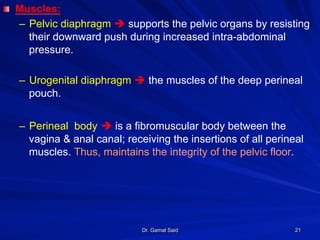
- 21. Dr. Gamal Said 21 ! Muscles: – Pelvic diaphragm è supports the pelvic organs by resisting their downward push during increased intra-abdominal pressure. – Urogenital diaphragm è the muscles of the deep perineal pouch. – Perineal body è is a fibromuscular body between the vagina & anal canal; receiving the insertions of all perineal muscles. Thus, maintains the integrity of the pelvic floor.
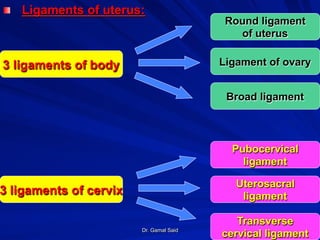
- 22. Dr. Gamal Said 22 ! Ligaments of uterus: Round ligament of uterus Ligament of ovary Broad ligament Pubocervical ligament Uterosacral ligament Transverse cervical ligament 3 ligaments of body 3 ligaments of cervix
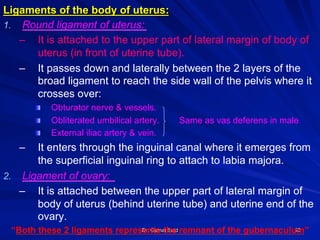
- 23. Dr. Gamal Said 23 Ligaments of the body of uterus: 1. Round ligament of uterus: – It is attached to the upper part of lateral margin of body of uterus (in front of uterine tube). – It passes down and laterally between the 2 layers of the broad ligament to reach the side wall of the pelvis where it crosses over: ! Obturator nerve & vessels. ! Obliterated umbilical artery. Same as vas deferens in male ! External iliac artery & vein. – It enters through the inguinal canal where it emerges from the superficial inguinal ring to attach to labia majora. 2. Ligament of ovary: – It is attached between the upper part of lateral margin of body of uterus (behind uterine tube) and uterine end of the ovary. “Both these 2 ligaments represents the remnant of the gubernaculum”
- 24. Dr. Gamal Said 24
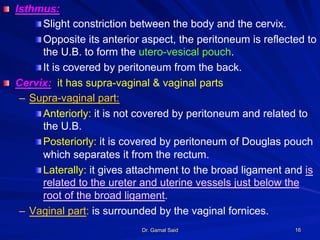
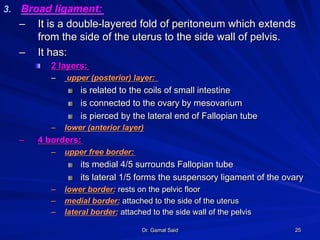
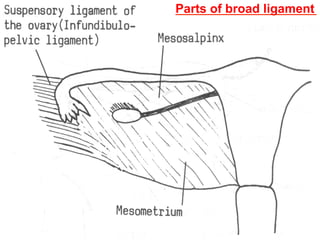
- 25. Dr. Gamal Said 25 3. Broad ligament: – It is a double-layered fold of peritoneum which extends from the side of the uterus to the side wall of pelvis. – It has: ! 2 layers: – upper (posterior) layer: ! is related to the coils of small intestine ! is connected to the ovary by mesovarium ! is pierced by the lateral end of Fallopian tube – lower (anterior layer) – 4 borders: – upper free border: ! its medial 4/5 surrounds Fallopian tube ! its lateral 1/5 forms the suspensory ligament of the ovary – lower border: rests on the pelvic floor – medial border: attached to the side of the uterus – lateral border: attached to the side wall of the pelvis
- 26. Dr. Gamal Said 26
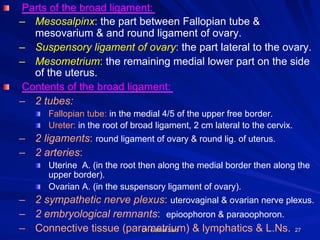
- 27. Dr. Gamal Said 27 ! Parts of the broad ligament: – Mesosalpinx: the part between Fallopian tube & mesovarium & and round ligament of ovary. – Suspensory ligament of ovary: the part lateral to the ovary. – Mesometrium: the remaining medial lower part on the side of the uterus. ! Contents of the broad ligament: – 2 tubes: ! Fallopian tube: in the medial 4/5 of the upper free border. ! Ureter: in the root of broad ligament, 2 cm lateral to the cervix. – 2 ligaments: round ligament of ovary & round lig. of uterus. – 2 arteries: ! Uterine A. (in the root then along the medial border then along the upper border). ! Ovarian A. (in the suspensory ligament of ovary). – 2 sympathetic nerve plexus: uterovaginal & ovarian nerve plexus. – 2 embryological remnants: epioophoron & paraoophoron. – Connective tissue (parametrium) & lymphatics & L.Ns.
- 28. Dr. Gamal Said 28 Parts of broad ligament
- 29. Dr. Gamal Said 29 Contents of broad ligament
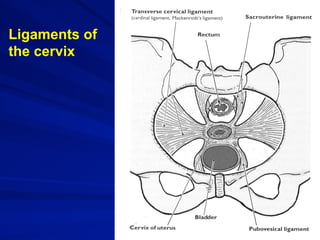
- 30. Dr. Gamal Said 30 Ligaments of the cervix: 1. Transverse cervical (Mackenrodt’s ) ligament: ! It is the main supporting factor of the uterus. ! It a fan-shaped ligament, which is formed of condensed extraperitoneal tissue between the side wall of the pelvis and side of cervix & vagina. 2. Pubo-cervical ligament: l It is a condensation of extraperitoneal tissue, which extends from the front of cervix & upper part of vagina to the back of the pubis, around the sides of the urethra. 3. Utero-sacral ligament: l It is a condensation of extraperitoneal tissue, which extends from the back of the cervix to the front of 2nd & 3rd pieces of sacrum, around the sides of the rectum.
- 31. Dr. Gamal Said 31 Ligaments of the cervix
- 32. Dr. Gamal Said 32 ! Uterine cavity: – The cavity of the body appears triangular (the upper angles are the openings of the uterine tubes & the lower angle is the opening of the internal os. – The cervix contains fusiform cervical canal: ! Its upper end is called internal os. ! Its lower end is called external os. The external os is rounded in nulliparous, slit-like in multiparous.
- 33. Dr. Gamal Said 33
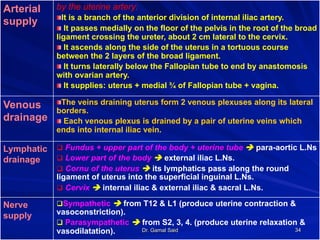
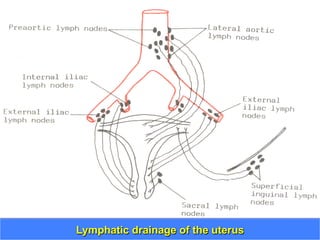
- 34. Dr. Gamal Said 34 Arterial supply by the uterine artery: ! It is a branch of the anterior division of internal iliac artery. ! It passes medially on the floor of the pelvis in the root of the broad ligament crossing the ureter, about 2 cm lateral to the cervix. ! It ascends along the side of the uterus in a tortuous course between the 2 layers of the broad ligament. ! It turns laterally below the Fallopian tube to end by anastomosis with ovarian artery. ! It supplies: uterus + medial ¾ of Fallopian tube + vagina. Venous drainage ! The veins draining uterus form 2 venous plexuses along its lateral borders. ! Each venous plexus is drained by a pair of uterine veins which ends into internal iliac vein. Lymphatic drainage q Fundus + upper part of the body + uterine tube è para-aortic L.Ns q Lower part of the body è external iliac L.Ns. q Cornu of the uterus è its lymphatics pass along the round ligament of uterus into the superficial inguinal L.Ns. q Cervix è internal iliac & external iliac & sacral L.Ns. Nerve supply q Sympathetic è from T12 & L1 (produce uterine contraction & vasoconstriction). q Parasympathetic è from S2, 3, 4. (produce uterine relaxation & vasodilatation).
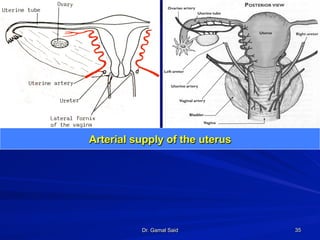
- 35. Dr. Gamal Said 35 Arterial supply of the uterus
- 36. Dr. Gamal Said 36Lymphatic drainage of the uterus
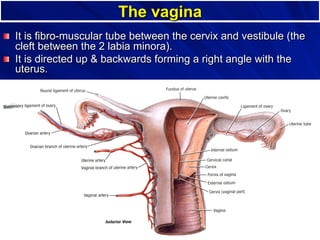
- 37. Dr. Gamal Said 37 The vagina ! It is fibro-muscular tube between the cervix and vestibule (the cleft between the 2 labia minora). ! It is directed up & backwards forming a right angle with the uterus.
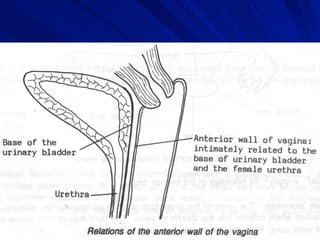
- 38. Dr. Gamal Said 38 ! Relations: – Anterior wall: (7 cm) ! Not covered by peritoneum ! Its upper 1/3 è is pierced by the cervix. ! Its middle 1/3 è is related to the base of U.B. ! Its lower 1/3 è is intimately related to the urethra. – Posterior wall: (9 cm) ! Its upper1/4 is covered by peritoneum which is reflected to the rectum to form the recto-vaginal (Douglas pouch) which contains coils of ileum ! Its middle 2/4 related to rectum. ! Its lower 1/4 is related to perineal body and anal canal.
- 39. Dr. Gamal Said 39
- 40. Dr. Gamal Said 40
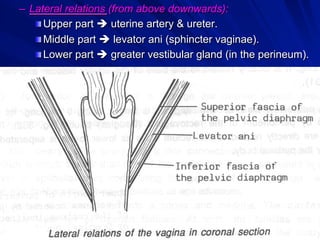
- 41. Dr. Gamal Said 41 – Lateral relations (from above downwards): ! Upper part è uterine artery & ureter. ! Middle part è levator ani (sphincter vaginae). ! Lower part è greater vestibular gland (in the perineum).
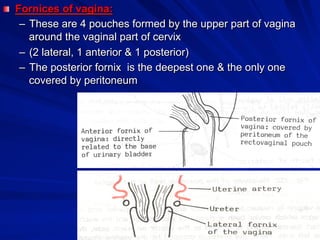
- 42. Dr. Gamal Said 42 ! Fornices of vagina: – These are 4 pouches formed by the upper part of vagina around the vaginal part of cervix – (2 lateral, 1 anterior & 1 posterior) – The posterior fornix is the deepest one & the only one covered by peritoneum
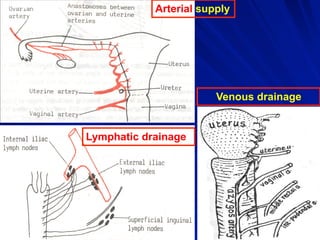
- 43. Dr. Gamal Said 43 Arterial supply It is supplied by: – Uterine artery. – Vaginal artery. – Middle rectal artery. – Internal pudendal artery. These arteries Anastomose in front & behind the vagina to form anterior & posterior “azygos arteries”. Venous drainage The vaginal veins form plexuses that drains into internal iliac vein. Lymphatic drainage ! Upper 1/3 è external iliac L.Ns. ! Middle 1/3 è internal iliac L.Ns. ! Lower 1/3 è superficial inguinal L.Ns. Nerve supply ! Upper 2/3 (pain insensitive) è by autonomic fibers – Sympathetic: L1, 2 – Parasympathetic: S 2, 3
- 44. Dr. Gamal Said 44 Arterial supply Venous drainage Lymphatic drainage