Preprint
Article
Clinical Impact of the Use of Ologen in Filtering Surgery
Altmetrics
Downloads
119
Views
42
Comments
0
A peer-reviewed article of this preprint also exists.
Submitted:
27 June 2024
Posted:
01 July 2024
You are already at the latest version
Alerts
Abstract
Purpose: To compare the efficacy and safety of trabeculectomy with a collagen matrix implant (Ologen®) versus trabeculectomy with mitomycin C (MMC) versus trabeculectomy with both Ologen® and MMC (OLO+MMC). Methods: This non-randomized study included 119 eyes of 101 patients with uncontrolled open-angle glaucoma who underwent trabeculectomy, either alone or combined with phacoemulsification. Data were initially registered following a standard surgical protocol and using an electronic database with structured fields. Patients were divided into three groups: 44 received trabeculectomy with adjunctive MMC (MMC group), 34 with Ologen® (OLO group), and 41 with both Ologen® and MMC (OLO+MMC group). The main outcome measures were the change in intraocular pressure (IOP), change in number of medications needed, complete success rate (defined as IOP≤20 mmHg and at least 20% IOP reduction without hypotensive medications), rate of complications, and rate of postoperative interventions. The follow-up period was 36 months.
Results: IOP significantly decreased (p=0,01) in all groups across all study visits, decreasing from 19.8 ± 4.6 mmHg to 12.7 ± 4.2 mmHg in the MMC group, from 20.5 ± 4.7 mmHg to 13.9 ± 3.5 mmHg in the OLO group, and from 23.5 ± 6.1 mmHg to 13.1 ± 3.5 mmHg in the OLO+MMC group. After correcting for baseline IOP, only the first two postoperative visits (first week and first month) showed significantly greater IOP reduction in the OLO+MMC group. The number of hypotensive medications was significantly reduced from 3.1±0.6 to 0.56±1.1 in the MMC group, from 2.9±0.4 to 0.83±1.1 in the OLO group, and from 3.0±0.6 to 0.45±0.95 in OLO + MMC group, with no statistically significant differences among the groups (p=0,57). Complete success rates were 63,6% in the MMC group, 67,6% in the OLO group, and 80,5% in the OLO +MMC group, with no statistically significant differences among the groups (p=0,21). Suture release was significantly more frequent in the MMC group (86,1%) than in the OLO group (62,1%) and in the OLO + MMC group (45,9%; p=0,02). Bleb needling, with (33.3%; p=0.005) or without (66.7%; p=0.0001) 5-Fluorouracil injection (5-FU), was significantly more common in the MMC group. The highest complete-success rate (61%) was offered by the OLO+MMC group. Conclusion: The use of Ologen® and Mitomycin C provided similar surgical IOP reduction in glaucoma surgery compared with MMC or Ologen® either alone but significantly reduced the need for postoperative interventions.
Keywords:
Subject: Medicine and Pharmacology - Ophthalmology
1. Introduction
Trabeculectomy has been the gold-standard glaucoma surgery since it was described by Cairns in 1968 [1]. Episcleral and subconjunctival scarring is the main cause of failure of filtering surgery. The intraoperative use of antimetabolites, Mitomycin C (MMC) and 5-Fluorouracil (5-FU), as well as post-operative handling of sutures, needling, or 5-FU injections have allowed surgeons to modulate and decrease conjunctival scarring as well as to improve filtering surgery success [2,3]. Indications for needling are encapsulation, scarring blebs with slow filtration, or insufficiently low intraocular pressure (IOP) [4]. Currently, surgeons are still searching for substances and/or implants and/or post-operative maneuvers that could modulate conjunctival scarring, to increase the efficacy and survival rate of filtering surgery and, more importantly, to customize IOP results to adequately fit each patient’s needs.
Ologen® (Aeon Astron Europe BV, Leiden, the Netherlands; OLO) is a matrix of collagen (CM) biodegradable, composed of a crosslinking of atelocollagen type I in more than 90% and glycosaminoglycans in less than 10%. It is a three-dimensional structure with porous diameters ranging from 10 to 300 microns. It has been proposed that this matrix acts on 3 different levels favoring aqueous bleb formation. Firstly, it induces a random growth of fibroblasts and collagen fibers. Secondly, it behaves as a spacer between the conjunctiva-tenon and the episcleral. Finally, it becomes a reservoir for aqueous humor.
Previous studies that compared the efficacy of trabeculectomy with Ologen® implant vs adjunctive Mitomycin C at different concentrations have reported conflicting results, but in general, no statistically significant differences after 12 months in terms of efficacy, medication reduction, and complications [5,6,7].
In 2018 Castejon et al. studied the combination of Ologen® and MMC at low doses (0.1 mg/ml) in patients undergoing trabeculectomy and phaco-trabeculectomy with 2 years of follow-up. They obtained equal results in the trabeculectomy group using Ologen® as without using it, but better IOP results when using Ologen® in the phaco-trabeculectomy group [8].
Currently, there is no study comparing Ologen combined with MMC at the dose of 0.2 mg/ml vs Ologen alone or MMC alone. The present study intends to compare the efficacy and safety of adjunctive MMC, Ologen®, or both together, and the required postoperative maneuvers in glaucoma patients requiring filtering surgery.
2. Materials and Methods
Study Design
This is a comparative and retrospective study with systematic data collection following a predefined surgical protocol. This study was approved by the Institutional Review Board of our institution and adhered to the principles outlined in the Declaration of Helsinki.
The medical history of patients operated on consecutively by the same glaucoma expert surgeon (JN) after 2011 was retrospectively reviewed. One hundred and nineteen eyes of 101 subjects were consecutively included after verifying the inclusion criteria. All of them underwent filtration surgery, with or without simultaneous phacoemulsification. All patients were Caucasian.
The patients were divided into 3 groups. The MMC group was comprised of 44 eyes, who underwent filtering surgery (trabeculectomy) before 2014 with intraoperative MMC (0,2 mg/ml for 2 minutes). The OLO group included 34 eyes who underwent filtering surgery (trabeculectomy) between 2014 and 2016, with subconjunctival Ologen® CM implant model 830601 (6mm x 2mm) at the end of surgery. Finally, the OLO + MMC group was integrated by 41 eyes who underwent trabeculectomy between 2016 to 2019 using the same MMC dose and time as group I, and subconjunctival Ologen®. We included consecutive patients, before and after the Ologen® implant was introduced in our clinical practice. In summary, all patients having surgery before January 2014 did not have the implant, and after that, every patient received the Ologen® implant.
The inclusion criteria were age over 18 years, diagnosis of primary open-angle glaucoma, pseudo exfoliative glaucoma or pigmentary glaucoma, and inadequate IOP control at the discretion of the ophthalmologist who followed the patient and performed the filtering surgery (JN). Of the 119 eyes, 64 underwent phaco-trabeculectomy, all of whom had the additional diagnosis of cataract with visual acuity under 20/25. Exclusion criteria were diagnosis of any other type of secondary glaucoma (post-traumatic, neovascular, aphakic…), previous vitro-retinal surgery, or a follow-up of less than 3 years. Additionally, all cases with posterior capsule rupture, vitreous prolapse in the anterior chamber, or impossible IOL implantation in the bag were excluded.
Examinations
Patients were evaluated preoperatively, and postoperatively at 1, 7, 14, 21, and 30 days, and 3, 6, 12, 18, 24, 30, and 36 months after the intervention following a predefined surgical follow-up protocol. Each examination included measurement of Snellen best corrected visual acuity (BCVA), IOP measured with applanation tonometry, slit-lamp bio-microscopy, and fundus examination. Complications and postoperative interventions were registered. Visual field (VF) testing was performed, at least, at baseline, 12, 24, and 36 months with program SITA standard 24-2 (Humphrey Visual Field, HFA II-i 740-15908/5.0, software version 3.1.1.264, Carl Zeiss Meditec, Dublin, CA, USA).
Definitions
Glaucoma was defined as the presence of simultaneous functional and structural damage. A glaucomatous VF defect was defined by the presence of a confirmed (in at least 2 VFs) group of three or more contiguous points with p < 5% and one of them with p < 1% in the pattern deviation map. The optic nerve was evaluated in color photographs and considered glaucomatous when there was rim thinning, rim notch, a papillary splinter hemorrhage, a nerve fiber layer defect, a cup-to-disc ratio asymmetry more than 0.3 between two eyes that could not be explained by asymmetry in the optic disc size. Glaucoma severity was classified according to mean deviation (MD) using the Hodapp criteria [9]. Complete success was defined as an IOP under 20 mmHg and at least 20% IOP reduction without hypotensive medications, and qualified success was considered when IOP was under 20 mmHg and IOP was reduced over 20% using ocular hypotensive medications. Therapeutic failure was defined as an IOP over 20 mmHg or a reduction of IOP less than 20% with medications, or an IOP under 6 mmHg on two consecutive study visits, or by the need for a second glaucoma surgery. The definitions for success and failure were used following the Guidelines on Design and Reporting Glaucoma Surgical Trials [10]. If IOP rose to a level considered too high by the physician (JN), anti-glaucomatous medication was initiated. If medical treatment after surgery failed to lower IOP to an acceptable level, or if VF or structural damage progressed, a new glaucoma surgery was performed.
Outcome Measures
The primary outcome was the mean change in IOP from baseline to the last follow-up visit. The secondary outcomes were the number and type of postoperative interventions (massage, suture release, needling, 5-FU injections), success rate, and frequency of complications
Surgical Technique
An experienced cataract and glaucoma surgeon performed all surgeries with the same standardized technique (JN). The surgical procedure consisted of peribulbar anesthesia and corneal traction sutures. Phacoemulsification was performed via a 2.2 mm clear-cornea incision in either nasal or temporal quadrant with intraocular lens (IOL) implantation. Complete aspiration of viscoelastic was performed at the end of phacoemulsification. The filtering procedure was placed to the right of the phaco-incision in the upper opposite quadrant. In all cases, dissection of a superior fornix-based conjunctival flap was performed. Electrocautery was used to control episcleral bleeding. A square (3 x 3mm) scleral flap of half of the scleral thickness was prepared. In two first groups (MMC and OLO+MMC groups), MMC 0,2 mg/ml was applied using three sponges (4 x 4 mm) over the scleral flap and under conjunctiva for 2 minutes and washed with 50 ml of saline solution afterward. Excision of trabecular meshwork was performed with Kelly punch and a peripheral iridectomy was excised in all cases. In all three groups, two releasable 10/0 Nylon sutures were placed on both corners of the scleral flap. Then the flow was checked, filling the anterior chamber with saline solution. In the two last groups (OLO and OLO+MMC groups), a flat cylindrical OLO implant of 12 mm in diameter and 1 mm in height (Ologen model no.862051; Aeon Astron Europe BV, Leiden, Netherlands) was placed over the scleral flap without suturing. Finally, a hermetic conjunctival suture was performed at the limbus with 10/0 nylon.
Postoperative Care
The standard postoperative regimen consisted of topical moxifloxacin three times a day (for 7 days) and dexamethasone every 2 hours for the first month and gradually tapered off during the second and third months. At each visit, the investigators examined the eye and evaluated the need for bleb manipulations. Two types of bleb manipulation were considered. Mechanical maneuvers could be performed to increase flow, break down adhesions, or scarring in the bleb. And included massage, removal of releasable sutures, and/or needling. Additionally, pharmacological bleb management could also be performed by using subconjunctival 5-Fluoracil injections (0,1 ml at 50mg/ml concentration), around the bleb, to aid draining and prevent scarring. These procedures were registered and were not considered treatment failures but as postoperative interventions.
Statistical Analysis
The statistical analysis was performed with MedCalc Statistical Software version 20.013 (MedCalc Software Ltd., Ostend, Belgium; https://www.medcalc.org; 2021) and SPSS (. IBM SPSS Statistics for Windows, IBM Corp. Released 2019, version 26.0; Armonk, NY: IBM Corp).
3. Results
All patients underwent filtration surgery, with or without simultaneous phacoemulsification, at our center after 2011. Among the 119 eyes included in the study, 64 eyes (53,8%) underwent phaco-trabeculectomy and 55 underwent trabeculectomy alone.
3.1. Baseline Patients’ Characteristics
Patient demographics are shown in Table 1. No statistically significant differences were found among the groups regarding age, sex, preoperative medication, type of glaucoma, or cup/disk ratio. The mean pre-operative IOP was 19.8±4.6 mmHg in the MMC group, 20.5±4.7 mmHg in the OLO group and were significantly lower (p=0.004) than the 23.5±6.1 mmHg found in the OLO+MMC group. The MMC group had slightly worse BCVA (p=0.02), Visual Field Index (VFI; p=0.01), and Median Deviation (MD; p=0.03), than the OLO group and OLO+MMC group.
3.2. Postoperative Intraocular Pressure
IOP was significantly reduced after surgery in all three groups at all follow-up visits (P<0.05; Figure A). The average postoperative IOP (mean ± SD) was 12.7±4.2 mmHg at 36 months and it was under 15 mmHg in all groups at all time points. In the MMC group, the mean IOP was 13.2±4.3 mmHg at 12 months, 12.5±3.9 mmHg at 24 months, and 12.7±4.2 mmHg at 36 months; in the OLO group, the mean IOP was 13.0±4.4 mmHg at 12 months, 14.4±3.6 mmHg at 24 months and 13.9±3.5 mmHg at 36 months; and, finally, in the OLO+MMC group, the mean IOP was 12.5±3.7 mmHg at 12 months, 13±3.9 mmHg at 24 months and 13±3.5 mmHg at 36 months. IOP reduction was significantly greater in the OLO+MMC group at all visits, but after adjusting for age, preoperative IOP, number of preoperative ocular hypotensive medications, type of surgery, and simultaneous cataract surgery, as covariates, mean IOP reduction (absolute values) was significantly greater in the group OLO+MMC group only at one week and one month (p>0.05), but not at other time points. There were no statistically significant differences in IOP reduction between the trabeculectomy vs phaco-trabeculectomy eyes in the three groups at 36 months (p=0,8). The IOP reduction in all groups is shown in Figure B, the percentage of eyes with IOP below 14 mmHg was 72,7% in the MMC group, 61,8% in the OLO group, and 73.2% in the OLO+MMC group.
3.3. Success Rate
At month 36, the overall success rate was 63,6% in the MMC group, 67,6% in the OLO group, and 80,5% in the OLO+MMC group. Complete success rates were 50% in the MMC group, 52,9% in the OLO group, and 61% in the OLO+MMC group. Finally, qualified success rates were 13,6% in the MMC group, 14,7% in the OLO group, and 19,5% in the OLO+MMC group. No differences in Kaplan-Meier survival curves (P<0,13) were found among the groups (Figure C).
3.4. Number of Medications
There was a significant decrease in the number of medications required after surgery compared with baseline (p<0.00) in each group and considering the whole sample, there were no significant differences among the groups at any point in time during the study. At baseline, the mean ±SD number of medications was 3.1±0.6 in the MMC Group, 2.9±0.4 in the OLO Group, and 3.0±0.6 in the OLO+MMC group. At 36 months after surgery, the MMC group required an average of 0.5±1 medications, the OLO group needed a mean of 0.7±1.1 medications, and the OLO+MMC group required 0.4±1 (p=0.29). There were 70%, 67%, and 76% of patients without medications at the end of the study in the MMC group, the OLO group, and the OLO+MMC group, respectively.
3.5. Postoperative Interventions
The three groups received postoperative interventions as needed during the follow-up period (Table 2). The total number of interventions was 74, 31, and 29 in the MMC group, the OLO group, and the OLO+MMC group respectively. The frequency of bleb massage was not statistically different among the groups (P=0,8). Suture release was performed significantly less frequently in the OLO and OLO-MMC groups (both with Ologen®) than in the MMC group(p=0,02). Similarly, mechanical bleb needling (p=0.016), and 5-FU injections (p=0.000) were significantly more frequent in the MMC group than in the other two groups. Glaucoma re-operation was required in four patients in the MMC group and two in each of the OLO and OLO+MMC groups during the follow-up period.
3.6. Complications
Complications were defined as any deviation from normal postoperative course. All complications are shown in Table 3. There were no intraoperative complications in any of the eyes in either group. A total of 90 eyes (75,6%) did not present any complications. There was no significant difference in the frequency of complications among the groups (P=0.09). Transient hypotony was found in 11.4% (n=5) of eyes in the MMC group, 17.6% (n=6) in the OLO group, and 16.7% (n=7) in the OLO+MMC group (p=0.69). Only one eye in the OLO+MMC group developed hypotony with macular folds which was managed by surgical intervention with placement of conjunctival compression sutures. No adverse reaction to the Ologen® implant, matrix extrusion, or conjunctival erosion was seen.
3.7. Visual Acuity
As expected, patients who underwent phaco-trabeculectomy manifested a significant improvement in visual acuity. There were no statistically significant differences in BCVA among the groups (p=0.12).
4. Discussion
It is well known that episcleral fibrosis and subconjunctival scarring decrease the success rate of glaucoma surgery, and for that reason, adjunctive antimetabolites have been used for decades to improve surgical efficacy [2,11]. Nevertheless, the complications of the use of MMC, such as hypotony, avascular blebs, or infection have led clinicians and researchers to look for new substances or materials that could offer similar efficacy with fewer complications.
Ologen® was initially proposed as a possible substitute for MMC [5,7]. Recent systematic review and meta-analysis indicated that trabeculectomy with Ologen was a safe and effective procedure in patients with glaucoma, but was also associated with less IOP lowering and fewer cases of hypotony than when trabeculectomy is augmented with MMC [5,12]. In the present study, we combined the antifibrotic action of MMC with the capabilities of Ologen CM, which include: separating the conjunctiva from the episclera, acting as a reservoir of aqueous humor, and, in addition, preventing the organization of fibroblast fibers. To the best of our knowledge, this is the first study that compares the outcomes of trabeculectomy and phaco-trabeculectomy with Ologen (12 mm x 1mm) together with MMC (0.2 mg/ml) versus trabeculectomy with only Ologen, versus trabeculectomy with only MMC.
Evaluating surgical techniques is always challenging due to the constantly evolving surgical options, the large volume of publications (many of which carry a considerable risk of bias), and the necessity for long-term follow-up since short-term results hold little significance in chronic, lifelong diseases. Moreover, any treatment should aim to improve the patient's clinical status and/or prognosis while minimizing avoidable harm.
The present study associated and compared two well-known varieties of trabeculectomy for three years and obtained significant results that could be applied in clinics. Nevertheless, this study has certain limitations that we believe don’t impede achieving its objective. First, it is a retrospective study, but patients were examined following a predefined surgical and postoperative protocol, and parameters were registered in and structured electronic database. Second, only one center and one surgeon participated which limits the strength but enhances the homogeneity of the procedures and examinations. Third, the distribution of patients in the treatment group was not randomized but patients were operated on with one of the three techniques selected consecutively, having been all MMC patients recruited first, then all of those comprising the OLO group and, during the last years, the cases were allocated in the OLO+MMC group. Finally, it included a limited and relatively low number of cases but with a long-term follow-up and it allowed the identification of significant differences among the groups.
One difficulty in comparing surgical results is always the differences in the techniques used in the studies. With Ologen CM there is an added potential influencing factor which is the size and height of the matrix. In our study a circular 12mm x 1mm was used, Narayanswam used a circular 7mm x 4mm, and Cillino, and many other authors, 6mm x 2 mm [7,13]. The lower total volume of the Ologen matrix could partially account for the lower final IOP values obtained in their study [7]. We speculate that Ologen 6 mm(D) x 2 mm(H)(model: 830601) covers a too-small area, raises the height of the filtration bleb due to its 2 mm, and could also exerts pressure on the scleral flap hindering the outflow of aqueous humor. While the latter could explain why some authors find a lower frequency of hypotony in the group treated with Ologen [14], we preferred the use of the Ologen 12 mm(D) x 1 mm(H)(model: 862051) that allows us to cover a larger surface, facilitate the formation flatter, more diffuse and posterior bleb, while exerting less pressure on the scleral flap.
We found no significant differences in mean IOP among the groups at any time point and IOP values were similar to those of Castejon et al. using MMC 0.1 mg/ml and slightly lower than those obtained by Cillino at 24 months who reported IOPs over 16 mmHg [8,15]. Differences could be related to the technique (different Ologen size) and/or the characteristics of the sample, among other causes.
The present study did identify a greater IOP reduction in the OLO+MMC group but after adjusting for age, preoperative IOP, number of preoperative ocular hypotensive medications, type of surgery, and the presence of simultaneous cataract surgery, as covariates, mean IOP reduction (absolute values) was significantly greater in the group treated with Ologen+MMC only at one week and one month, but not at other study points.
All groups showed a significant and similar decrease in the medications needed with similar values to those reported by Sen et al. [16] who found a decrease in required medications from 3 to 0.5 with MMC or with OLO. Our results showed a non-significant tendency for a higher value in the final postoperative medications needed in the OLO group (0.7) than in the OLO+MMC group (0.4).
Success rates can be very useful to evaluate and compare different techniques but it is important to check the definition used in each study to compare results from different manuscripts. Cillino obtained a rather low success rate of 40%, with MMC or with Ologen, at 24 months which can be partially explained by its exigent definition of an IOP under 15 mmHg, but also to the slightly higher mean final IOPs reported [15]. Min et al. studied the use of Ologen soaked with MMC (0.1mL of 0.2 mg/mL) prospectively in 30 eyes and found, at 12 months, a complete success rate of 40%, with an identical definition applied in the present study [14]. This value is lower than the 61% at 36 months obtained by the Ologen+MMC group in our study. Additionally, we found IOP< 14 mmHg without medication in 72.7% of the MMC group, 61.8% in the Ologen group, and 73.2% in the Ologen+MMC group at 36 months, figures that are again superior to those reported by Cillino et al. at 24 month [15]. In their study, IOP was under 15 mmHg in 40% in the MMC group and 50% in the Ologen group [15].
Postoperative maneuvers, whether mechanical or medical, are very important and frequently needed to modulate bleb scarring, and for that reason, they become a significant factor that should be evaluated as an outcome measure of the different techniques. Suture manipulation can be very useful in the early postoperative period to increase flow when needed. One important issue is that the Ologen matrix does worsen external visual access to sutures and this needs to be taken into account to design the surgical technique. Additionally, the use of thicker Ologen implants increases the difficulty of seeing and reaching sutures with laser and, undoubtedly, increases bled height for at least several months. The use of releasable sutures from the corneal surface, thinner Ologen models, or modeling a bit of the Ologen to leave part of the sutures visible can facilitate suture manipulation. Cillino et al. [16] obtained similar IOP values with MMC or Ologen leaving one of the sutures untied in the Ologen group, Narayanswam et al. [13] used only one fixed suture with minimal tension and one releasable suture in the OLO group and two fixed sutures in the MMC group, while we sutured all flaps with two releasable sutures. All these slight differences in the technique might influence the global results, particularly those related to the number of suture lysis or suture releases performed. The higher percentage of suture release maneuvers in our study was probably related to the fact of using two sutures and may also be the reason for a low final IOP with a global mean value of 12.9 mmHg. In our study, suture release was needed less frequently in the OLO (62%) or OLO+MMC (47%) groups than in the MMC group (86%). This suggests that Ologen helps flow maintenance and keeps IOP sufficiently low to require less suture release. This could be explained by the Ologen action of keeping space between the sclera and conjunctiva and acting as a reservoir for aqueous humor. The use of a releasable suture or 1mm height Ologen is recommended to facilitate access to sutures with the laser.
Bleb needling was performed in 27% of the patients in the MMC group, while in the OLO and OLO+MMC groups, it was only performed in 7% and 13% of the cases (p=0.016), suggesting that Ologen may reduce the risk for bleb encapsulation. Nevertheless, Cillino et al. reported bleb needling in 35% of the MMC group and 30% in the OLO group without intergroup differences, and Naryanswam reports 40% bleb needling in the OLO group and 6% in the MMC group [7,13]. The latter could be explained because their study used a higher concentration of MMC (0.4mg/ml to 2 minutes) and a low rate of suture lysis in the Ologen group. These contradictory results could be related to the different criteria to indicate bleb needling among the studies.
Subconjunctival 5-FU injections in the postoperative period were more frequently performed in the MMC group (66%) than in the OLO (14%) or OLO+MMC group (16%, p<0.001). Similarly, Papaconstantinou [17] reports 10% in the Ologen group and 25% in the MMC group although this difference was not significant. Our results indicate that postoperative management in those patients operated on using Ologen was easier with the need for fewer procedures. As many as 74 postoperative interventions were performed in the MMC group, while in the groups where Ologen was used only 29 and 31 maneuvers were needed.
The use of Ologen in filtration surgery seems to be, at least, as safe as traditional trabeculectomy. The only complication that appeared more frequently in our study in the OLO+MMC group was wound leak (p=0.02). This has also been reported by other authors such as Cillino et al.l [15] and Tanna et al. [18]. Possibly the association of MMC that delays the healing process with the expanding effect of Ologen may increase the tendency to present wound leak. These results recommend paying special attention to obtaining a water-tight conjunctival closure. Finally, in our study, no allergy or increased inflammatory reaction was reported for up to 36 months.
In summary, the use of an Ologen implant in conjunction with MMC in trabeculectomy does not seem to influence final IOP values but does facilitate postoperative care by reducing the need for suture release, 5FU injections, or bleb needling. Prospective, randomized, long-term studies are needed to confirm this fact as well as to evaluate if it might improve bleb survival over time.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Institut Català de la Retina (protocol code ICR-O8/22 at 8 of September 2022).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
No data Availability Statements are available.
Acknowledgments
No financial disclosures.
Conflicts of Interest
The authors declare no conflicts of interest.
Appendix
Figure 1.
Mean IOP by treatment group.

The IOP reduction from baseline was significant compared with baseline in all groups and at all time points. No significant differences were found in mean IOP at any follow-up visit among the groups.
Figure 2.
IOP reduction in all groups at different time points.
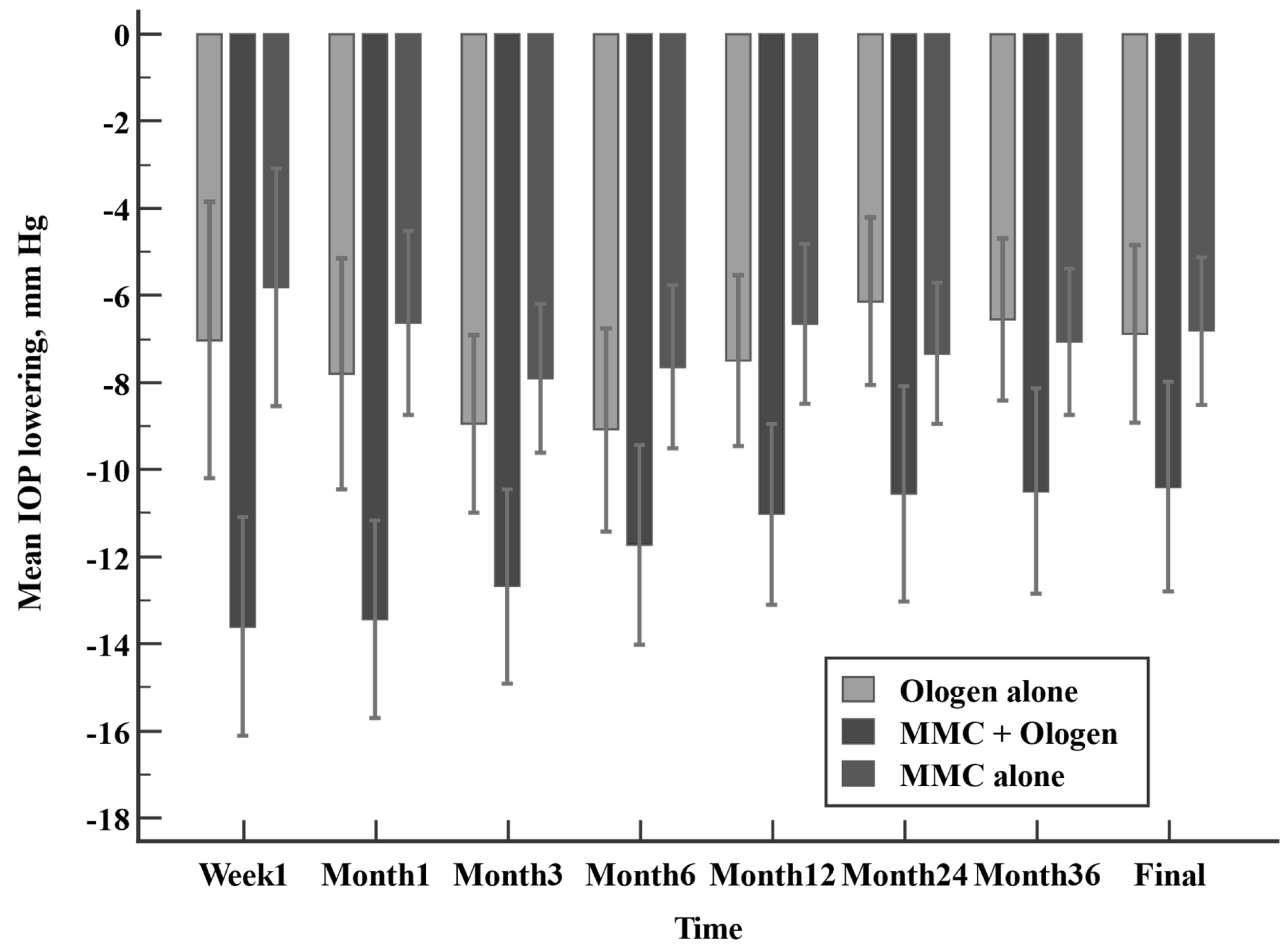
Although IOP reduction was significantly greater in the OLO+MMC group, after adjusting for age, preoperative IOP, number of preoperative ocular hypotensive medications, type of surgery, and cataract surgery or not, as covariates, mean IOP reduction (absolute values) was significantly greater in the group OLO+MMC group only at one week and one month (p>0.05).
Figure 3.
Kaplan-Meier survival curves (P<0,13).

Kaplan-Meier survival curves for qualified success (IOP≤18 mmHg with at least one medication). Log-rank (Mantel-Cox test) P=0.01
References
- Cairns, JE. Trabeculectomy. Preliminary report of a new method. Am J Ophthalmol 1968;66(4):673-679. [CrossRef]
- Bindlish R, Condon GP, Schlosser JD, D’Antonio J, Lauer KB, Lehrer R. Efficacy and safety of mitomycin-C in primary trabeculectomy: five-year follow-up. Ophthalmology 2002;109(7):1336-1341. [CrossRef]
- Khaw PT, Chiang M, Shah P, Sii F, Lockwood A, Khalili A. Enhanced trabeculectomy: the Moorfields Safer Surgery System. Dev Ophthalmol 2012;50:1-28. [CrossRef]
- Halili A, Kessel L, Subhi Y, Bach-Holm D. Needling after trabeculectomy - does augmentation by anti-metabolites provide better outcomes and is Mitomycin C better than 5-Fluoruracil? A systematic review with network meta-analyses. Acta Ophthalmol (Copenh) 2020; 98(7), 643–653. [CrossRef]
- He M, Wang W, Zhang X, Huang W. Ologen Implant versus Mitomycin C for Trabeculectomy: A Systematic Review and Meta-Analysis. PLoS ONE 2014;9(1). [CrossRef]
- Eldaly ZH, Maasoud AA, Saad MS, Mohamed AA. Comparison between Ologen implant and different concentrations of Mitomycin C as an adjuvant to trabeculectomy surgery. Oman J Ophthalmol 2017;10(3):184-192. [CrossRef]
- Cillino S, Casuccio A, Di Pace F, Cagini C, Ferraro LL, Cillino G. Biodegradable collagen matrix implant versus mitomycin-C in trabeculectomy: five-year follow-up. BMC Ophthalmol 2016;16. [CrossRef]
- Castejón MA, Teus MA, Bolivar G, Paz-Moreno-Arrones J, Castaño B. Outcomes of Trabeculectomy and Phacotrabeculectomy With Collagen Matrix Implant (Ologen) and Low-dose Mitomycin C: 2-Year Follow-up. J Glaucoma 2018;27(1):50-54. [CrossRef]
- Hodapp, E, Douglas R, Parrish R. Clinical decisions in glaucoma. In: St. Louis, Mo.:Mosby; 1993:204. Available online: http://trove.nla.gov.au/work/23580229.
- T.M. Shaarawy, M.B. Sherwood, F. Grehn. Guidelines on Design and Reporting of Glaucoma Surgical Trials. Kugler Publications 2009. Available online: www.kuglerpublications.com.
- Lama PJ, Fechtner RD. Antifibrotics and wound healing in glaucoma surgery. Surv Ophthalmol 2003;48(3):314-346. [CrossRef]
- Song, D. S. , Qian, J., & Chen, Z. J. Ologen implant versus mitomycin-C for trabeculectomy: A meta-analysis. Medicine, 1609. [Google Scholar] [CrossRef]
- Narayanaswamy, A. , Perera, S. A., Htoon, H. M., Hoh, S. T., Seah, S. K., Wong, T. T., & Aung, T. Efficacy and safety of collagen matrix implants in phacotrabeculectomy and comparison with mitomycin C augmented phacotrabeculectomy at 1 year. Clin Exp Ophthalmol. [CrossRef]
- Min JK, Kee CW, Sohn SW et al. Surgical outcome of mitomycin C-soaked Collagen Matrix Implant in trabeculectomy. 4: J Glaucoma 2013; 22, 2013.
- Cillino, S. , Di Pace, F., Cillino, G., & Casuccio, A. Biodegradable collagen matrix implant vs mitomycin-C as an adjuvant in trabeculectomy: a 24-month, randomized clinical trial. Eye (Lond), 1598. [Google Scholar] [CrossRef]
- Sen, M. , Midha, N., Sidhu, T., Angmo, D., Sihota, R., & Dada, T. (2018). Prospective Randomized Trial Comparing Mitomycin C Combined with Ologen Implant versus Mitomycin C Alone as Adjuvants in Trabeculectomy. ( 1(2), 88–98. [CrossRef] [PubMed]
- Papaconstantinou, D. , Georgalas, I., Karmiris, E., Diagourtas, A., Koutsandrea, C., Ladas, I., Apostolopoulos, M., & Georgopoulos, G. (2010). Trabeculectomy with OloGen versus trabeculectomy for the treatment of glaucoma: a pilot study. Acta Ophthalmol. [CrossRef]
- Tanna, A. P. , Rademaker, A. W., de Moraes, C. G., Godfrey, D. G., Sarkisian, S. R., Jr, Vold, S. D., & Ritch, R. (2016). Collagen matrix vs mitomycin-C in trabeculectomy and combined phacoemulsification and trabeculectomy: a randomized controlled trial. BMC Ophthalmol. [CrossRef]
Table 1.
Baseline patients’ characteristics in the MMC, the OLO, and the OLO+MMC groups.
| Units | MMC | OLO | OLO+MMC | P | |
|---|---|---|---|---|---|
| Age, years | (mean±SD) | 67.8 (11.2) | 71.5 (13.6) | 68.9 (12.3) | 0.41 |
| Gender 刘BCVA* | (M/F)刘(mean±SD) | 22/22刘0.69(0.2) | 14/20刘0.79(0.2) | 18/24刘0,8(0.2) | 0.69刘0.04 |
| Type of Glaucoma | 0.96 | ||||
| POAG* | n(%) | 35 (79.5) | 21 (79.4) | 32 (76.2) | |
| CACG* | n(%) | 3 (6.8) | 2 (5.9) | 5 (11.9) | |
| PEXG* | n(%) | 6 (13.6) | 5 (14.7) | 5 (11.9) | |
| Preoperative IOP | (mean±SD) | 19,8 (4.6) | 20.5 (4.7) | 23.5 (6.1) | 0.04 |
| Preoperative medications | Nº (mean±SD) | 3.1 (0.6) | 2.9 (0.4) | 3 (0.6) | 0.52 |
| Mean deviation | dB(mean±SD) | -12.6 (7.6) | -8.9 (7.1) | -8.5 (8.3) | 0.03 |
| MD < -6 | dB(mean±SD) | 10 (22.7) | 15 (45.5) | 20 (48.8) | |
| MD -6 – -12 | dB(mean±SD) | 10 (22.7) | 10 (30.3) | 8 (19.5) | |
| MD > -12 | dB(mean±SD) | 24 (54.5) | 8 (24.2) | 13 (31,7) | |
| VFI | (mean±SD) | 64.1 (25.5) | 75.5 (25.5) | 76.3 (22.6) | 0.01 |
| Cup/Disk Ratio刘Trabeculectomy 刘Phacotrabeculectomy | (mean±SD)刘n(%)刘n(%) | 0.7 (0.2)刘19 (43.2)刘25 (56.8) | 0.7 (0.1)刘15 (44.1)刘19 (55.9) | 0.7 (0.1)刘21 (51,2)刘20(48,8) | 0.87刘0.81刘0.81 |
*BCVA (Best Corrected Visual Acuity); POAG (Primary Open Angle Glaucoma); CACG (Chronic Angle Closure Glaucoma); SD (Standard deviation); dB (decibels).
Table 2.
Postoperative interventions in all groups.
| Porstoperative刘Intervenction | MMC (n=44) | (%) | OLO (n=34) | (%) | OLO+MMC (n=42) | (%) | P |
|---|---|---|---|---|---|---|---|
| Massage | 3 | (8.3) | 3 | (10.3) | --- | --- | 0.156 |
| Suture release | 31 | (86.1) | 18 | (62.1) | 17 | (45.9) | 0.002 |
| Needling | 12 | (27.3) | 2 | (6.9) | 5 | (13.5) | 0.016 |
| 5-Fluoracil | 22 | (61.1) | 4 | (13.8) | 6 | (16.2) | 0.000 |
| Total PI | 74 | 31 | 29 | ||||
| Nº patients | 38 | 21 | 18 |
*PI (Postoperative interventions).
Table 3.
Postoperative complications after surgery in all groups.
| Complications | MMC (n=44) | (%) | OLO (n=34) | (%) | OLO+MMC (n=41) | (%) | Total % |
|---|---|---|---|---|---|---|---|
| Choroidal detachment | 1 | (2.3) | 3 | (8.8) | 2 | (4.9) | 5 |
| Early wound leak | 2 | (4.5) | 1 | (2.9) | 8 | (19) | 9.2 |
| Encapsulated bleb | - | --- | 1 | (2.9) | 2 | (4.9) | 2.5 |
| Haematic tyndall | - | --- | - | --- | - | --- | --- |
| Hypotony maculopathy | 2 | (4.5) | 3 | (8.8) | 4 | (9.5) | 7.6 |
| Hypotony >1 month | 5 | (11.4) | 6 | (17.6) | 7 | (16.7) | 15.2 |
| Transient hypotony | 1 | (2.3) | - | --- | 1 | (2.3) | 1.5 |
| Shallow anterior chamber | 2 | (4.5) | 1 | (2.9) | 2 | (4.9) | 4.1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
XEN Glaucoma Implant for Refractory Glaucoma Management: Results and Complications during a 2-year Follow-up
Katarzyna Lewczuk
et al.
,
2021
Five-Year Clinical Outcomes of Trabectome Surgery at a Single Glaucoma Center
Hamed Esfandiari
et al.
,
2018
Impact of Same-Session Trabectome Surgery on Ahmed Glaucoma Valve Outcomes
Hamed Esfandiari
et al.
,
2018
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated








