Preprint
Review
Harnessing AI and IoT for the Future of Healthcare: A Comprehensive Review on Chronic Disease Management and Pandemic Response
Altmetrics
Downloads
179
Views
125
Comments
0
This version is not peer-reviewed
Preprints on COVID-19 and SARS-CoV-2
Submitted:
29 September 2024
Posted:
30 September 2024
You are already at the latest version
Alerts
Abstract
The integration of Artificial Intelligence (AI) and the Internet of Things (IoT) in healthcare is transforming chronic disease management and pandemic response, particularly for vulnerable populations such as the elderly and those with multiple chronic conditions. This review systematically examines the current applications of AI and IoT technologies in managing chronic diseases like diabetes, cardiovascular disease, and chronic obstructive pulmonary disease (COPD), alongside their role in enhancing healthcare response during the COVID-19 pandemic. Key findings demonstrate significant improvements in patient outcomes, including enhanced glycemic control in diabetes management, early detection of cardiovascular anomalies, and a reduction in hospital admissions for chronic disease patients through AI-enabled remote monitoring. Despite these advancements, challenges remain, including data security, algorithmic bias, and the high cost of implementing AI and IoT systems. This review explores future directions for overcoming these obstacles, emphasizing the potential of multi-dimensional data integration, real-time predictive analytics, and personalized AI models to further revolutionize healthcare. Additionally, the accompanying Graphic Abstract visually illustrates how AI-driven insights, generated from IoT-enabled devices, are transforming healthcare delivery by facilitating real-time monitoring, personalized interventions, and proactive patient care. The article concludes with recommendations for addressing the technological, ethical, and regulatory challenges that must be overcome to fully realize the potential of AI and IoT in healthcare.
Keywords:
Subject: Computer Science and Mathematics - Computer Science
1. Introduction
In recent years, the healthcare sector has witnessed rapid advancements in the use of emerging technologies, particularly Artificial Intelligence (AI) and the Internet of Things (IoT). These technologies have proven to be transformative, especially in managing chronic diseases like diabetes, cardiovascular disease, and addressing public health emergencies such as the COVID-19 pandemic. The increasing burden of chronic diseases on healthcare systems, coupled with the aging global population, presents a unique set of challenges. Healthcare for elderly and disabled individuals, who often suffer from multiple chronic conditions, is becoming unsustainable due to rising costs and resource limitations. This situation has necessitated the adoption of innovative solutions like AI and IoT to enhance care delivery, improve patient outcomes, and reduce the strain on healthcare infrastructure [1,2,3,4,5,6].
The integration of AI and IoT in healthcare has resulted in the development of smart healthcare systems that enable continuous patient monitoring, real-time data collection, and automated decision-making. These technologies offer a new approach to healthcare, providing personalized care through predictive analytics, optimizing the use of medical resources, and allowing for early detection of diseases or health deterioration [7,8]. The use of AI-powered tools like machine learning algorithms and IoT-enabled wearable devices has facilitated remote monitoring of patients, which is especially beneficial for vulnerable populations such as the elderly and disabled, who require constant healthcare supervision but may face mobility or access barriers [9,10,11,12].
In the context of the COVID-19 pandemic, the role of AI and IoT became even more prominent. These technologies have been employed for various purposes, from tracking and predicting the spread of the virus to supporting clinical decision-making through the analysis of vast amounts of healthcare data [13]. AI and IoT have helped optimize the management of hospital resources, facilitated remote patient consultations, and enhanced contact tracing efforts [14,15]. These applications have proven critical in mitigating the effects of the pandemic, particularly in protecting high-risk groups such as the elderly and those with pre-existing conditions [16,17].
However, while AI and IoT hold immense potential in transforming healthcare, several challenges remain. Issues such as data privacy, cybersecurity, and ethical concerns surrounding AI-driven decision-making have raised questions about their widespread adoption [6,18,19,20,21]. Additionally, the cost of implementation, technological infrastructure, and the need for robust regulatory frameworks are barriers that must be addressed to fully realize the benefits of AI and IoT in healthcare [1,3,22,23].
This paper aims to provide a comprehensive analysis of the current advancements in AI and IoT technologies in healthcare, with a particular focus on their applications in chronic disease management and pandemic response. By exploring the synergies between AI and IoT, this study will highlight how these technologies can improve healthcare outcomes for the elderly and disabled populations. Furthermore, the paper will evaluate the challenges and limitations of these technologies and propose potential directions for future research and development.
2. Background and Literature Review
AI and IoT in Healthcare
The integration of Artificial Intelligence (AI) and the Internet of Things (IoT) into healthcare systems has ushered in a new era of smart healthcare, where advanced technologies facilitate real-time monitoring, personalized treatment, and predictive analytics. AI, which involves the simulation of human intelligence in machines, has increasingly found applications in diagnosis, treatment planning, and healthcare automation [3,24]. Meanwhile, IoT enables the interconnection of medical devices and systems through the internet, allowing continuous data collection from patients. This has led to the concept of the Internet of Medical Things (IoMT), where AI-powered IoT systems enhance healthcare services by enabling remote monitoring, data analysis, and patient management [25].
These advancements have dramatically shifted the way chronic diseases are managed. The combination of AI and IoT has proven especially effective in monitoring real-time physiological data, offering continuous insights into patient health that are not only beneficial for routine care but also in emergency interventions. For instance, IoT devices embedded with AI algorithms can predict patient deterioration and suggest preventive measures to healthcare providers before conditions become critical [26].
Chronic Disease Management Using AI and IoT
Chronic diseases, such as diabetes, cardiovascular disease, and hypertension, remain the leading cause of death globally, responsible for 71% of all deaths annually, according to the World Health Organization (WHO) [27]. Traditional chronic disease management is costly, labor-intensive, and often inefficient. AI and IoT technologies address these issues by offering automated systems that provide round-the-clock monitoring of patient vitals, coupled with predictive analytics to assist in decision-making.
In diabetes management, AI systems integrated with IoT-enabled devices like continuous glucose monitors (CGMs) and smart insulin pumps have revolutionized patient care. AI algorithms analyze glucose readings in real-time, automatically adjusting insulin doses for patients. This system, often referred to as the artificial pancreas (see Figure 1), significantly improves glycemic control, thus reducing long-term complications for diabetic patients [28].
In addition to diabetes, cardiovascular disease (CVD) management has benefited from the integration of AI and IoT. Wearable ECG monitors that use AI algorithms are capable of detecting irregular heart rhythms, allowing early intervention and reducing the risk of stroke or heart attack. These systems continuously monitor a patient's heart rate and provide insights into long-term heart health trends, enabling healthcare providers to adjust treatment plans as needed [29]. Additionally, IoT devices, such as smart blood pressure monitors, paired with AI algorithms, can automatically flag abnormal readings, leading to faster and more effective responses to hypertension [30]. Table 1 provides an overview of the main applications of AI and IoT in healthcare, demonstrating how these technologies are improving the management of chronic diseases and elderly care.
AI and IoT in the COVID-19 Pandemic Response
The COVID-19 pandemic has highlighted the potential of AI and IoT in crisis management. These technologies have been integral in tracking the spread of the virus, monitoring infected individuals, and optimizing hospital resources. AI systems have been used to predict infection trends, model healthcare system capacity, and analyze clinical data for faster, more accurate diagnostics. AI-driven image analysis tools were used to scan chest x-rays and CT scans for signs of COVID-19-related pneumonia, reducing diagnosis times and improving patient outcomes [37].
Simultaneously, IoT-enabled wearable devices allowed remote monitoring of patients with mild COVID-19 symptoms, reducing the need for hospital visits and thus minimizing the risk of virus transmission. Patients’ oxygen saturation, body temperature, and heart rate were monitored in real-time, and healthcare providers were alerted in case of any abnormalities [38]. Figure 2 showcases the architecture of IoT-enabled healthcare for COVID-19 patient monitoring.
Existing Research Gaps
While AI and IoT technologies hold great promise in transforming healthcare, several research gaps remain, limiting their full integration. A critical challenge involves ensuring data privacy and security in IoT systems, which handle highly sensitive patient information. IoT devices are often vulnerable to cyberattacks, which could result in data breaches that compromise patient confidentiality and trust in these technologies [39]. Additionally, algorithmic bias remains a concern in AI-based healthcare systems. AI systems that are trained on non-representative datasets may yield inaccurate diagnoses or care recommendations, potentially exacerbating healthcare inequalities [40].
Moreover, the cost of implementation and technological infrastructure required for AI and IoT systems can be prohibitive, especially in low-income countries. While these technologies may reduce healthcare costs in the long term, the initial investment is significant, and many healthcare systems lack the resources to fully adopt AI and IoT solutions [41,42,43,44,45]. Table 2 summarizes the key challenges in implementing AI and IoT technologies in healthcare, highlighting the hurdles that must be overcome to achieve full integration.
Figure 3 further highlights the main challenges faced when implementing AI and IoT technologies in healthcare systems, particularly the issues surrounding privacy, cost, and regulation.
In summary, the review of current literature demonstrates that AI and IoT technologies are poised to revolutionize healthcare, particularly in the management of chronic diseases and pandemic responses. Despite the numerous benefits, the full potential of these technologies is yet to be realized, primarily due to issues related to data security, bias, and the cost of implementation. Addressing these challenges through robust regulatory frameworks and investment in infrastructure is essential for the widespread adoption of AI and IoT in healthcare.
3. Methodology
This review follows a systematic, quantitative methodology to evaluate the integration of Artificial Intelligence (AI) and the Internet of Things (IoT) in healthcare, focusing on chronic disease management and pandemic response. The methodology is designed to ensure a comprehensive analysis of the literature, in line with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [50]. The steps taken include a structured literature search, application of inclusion and exclusion criteria, data extraction, synthesis of findings, and statistical validation.
The flow of the methodology is visualized in Figure 4, which outlines each step of the review process, from the initial literature search to the final validation of results.
3.1. Literature Search Strategy
A systematic literature search was conducted across four major academic databases: PubMed, IEEE Xplore, Scopus, and Web of Science. These databases were selected based on their relevance to the healthcare, engineering, and technology domains, ensuring a multidisciplinary approach to the review. The search terms used were: "AI in healthcare", "IoT in healthcare", "AI and IoT integration in healthcare", "chronic disease management", "AI and COVID-19 healthcare"
The search was limited to articles published between January 2015 and September 2024. This timeframe was chosen to capture the latest developments in AI and IoT technologies, particularly those relevant to the rapid advancements in healthcare during and after the COVID-19 pandemic. Additionally, only peer-reviewed journal articles and high-impact conference papers were included in the initial search.
The search yielded a total of 5,200 papers: 2,300 papers on "AI in healthcare", 1,500 papers on "IoT in healthcare", 800 papers on "AI and IoT integration", 400 papers on "chronic disease management", and 200 papers on "COVID-19 AI applications in healthcare".
3.2. Inclusion and Exclusion Criteria
To ensure the relevance and quality of the studies included in this review, we applied a set of predefined inclusion and exclusion criteria (as depicted in Figure 4).
Inclusion Criteria:
- Studies that quantitatively evaluated the application of AI and IoT technologies in healthcare, particularly in chronic disease management (e.g., diabetes, cardiovascular disease) or pandemic response (e.g., COVID-19).
- Papers that reported measurable outcomes such as improvements in healthcare efficiency, patient outcomes, or cost reductions.
- Studies that demonstrated empirical evidence of AI and IoT integration in real-world healthcare settings.
- Only peer-reviewed journal articles and conference papers published in English.
Exclusion Criteria:
- Papers focused on non-healthcare sectors or theoretical models without practical implementation.
- Preprints and other non-peer-reviewed articles.
- Studies without quantitative data or measurable outcomes.
- Papers published in languages other than English.
- Following the application of these criteria, 578 papers were selected for further analysis. This step reduced the dataset by removing papers that did not meet the quality or relevance standards required for the review.
3.3. Data Extraction and Synthesis
Data extraction was performed on the 578 eligible studies to ensure a structured and comprehensive analysis. A literature matrix was created to extract and organize key information from each paper. The data extracted included:
- Study design: The methodology used in the study (e.g., randomized controlled trials, observational studies, case studies).
- Technologies applied: Specific AI models (e.g., machine learning algorithms, neural networks) and IoT devices (e.g., wearable health sensors, remote monitoring systems) used in the study.
- Healthcare applications: Areas of healthcare where the AI and IoT technologies were applied (e.g., diabetes management, cardiovascular disease monitoring, COVID-19 diagnostics).
- Outcomes: Quantitative results reported by the studies, such as improvements in patient outcomes, reductions in diagnostic time, increases in resource efficiency, or cost savings.
The matrix also categorized papers based on whether the focus was on chronic disease management or pandemic response. These two primary categories were further divided into specific use cases (e.g., diabetes, hypertension, respiratory diseases for chronic care; resource allocation and remote patient monitoring for pandemic response).
3.4. Quantitative Synthesis and Meta-Analysis
To aggregate the quantitative data from the selected studies, a meta-analysis was conducted using statistical tools to identify trends and measure the impact of AI and IoT technologies in healthcare. Out of the 578 papers, 93 studies provided sufficient empirical data to be included in the meta-analysis.
Key metrics evaluated include:
- HbA1c reduction in diabetic patients using AI-integrated continuous glucose monitoring systems (average reduction: 0.9% across 40 studies).
- Early detection rate of cardiovascular anomalies using AI-based wearable devices, which showed a 25% improvement over traditional monitoring systems across 25 studies.
- Diagnosis time reduction in COVID-19 patients through AI-driven CT scan interpretation, which reduced diagnosis time by 35% in 28 studies.
- Reduction in hospital admissions for chronic disease patients monitored via IoT-enabled remote healthcare systems, with a 20% reduction in admissions for high-risk patients.
The meta-analysis also revealed an overall improvement in healthcare resource utilization, with AI and IoT technologies reducing operational costs by an average of 15-20% across various healthcare settings.
3.5. Validation of Results and Statistical Significance
To ensure the robustness of the findings, the statistical significance of the results was validated using t-tests and Cochran’s Q test. A p-value threshold of <0.05 was used to determine the significance of the improvements reported in the studies. For example, the HbA1c reduction in diabetic patients was found to be statistically significant (p = 0.01), as was the 35% reduction in diagnosis time for COVID-19 patients (p = 0.003).
Heterogeneity across studies was assessed using I² statistics, which indicated moderate heterogeneity (I² = 48%). This suggests that while the studies differed in certain aspects, the overall trends were consistent, allowing for meaningful aggregation of the data.
3.6. Limitations
Despite the rigorous methodology, several limitations must be acknowledged:
- Language bias: Only English-language studies were included, potentially excluding important findings from non-English-speaking regions.
- Publication bias: The review focused on peer-reviewed studies, which may exclude valuable insights from industry reports or white papers.
- Scope of review: The review is limited to papers published up to September 2024, and therefore does not account for the latest developments in AI and IoT technologies post-publication.
- Variability in reporting standards: Some studies used different metrics or lacked standardization in how outcomes were reported, which introduced challenges in direct comparison across studies.
4. Results
The results presented here are based on a systematic review of 578 papers, of which 93 studies were subjected to detailed quantitative analysis. The findings are grouped into two main categories: chronic disease management and pandemic response, with additional attention given to overarching themes such as improvements in healthcare outcomes, diagnostic accuracy, and cost efficiency. The results also identify challenges and limitations encountered in implementing AI and IoT technologies in healthcare.
4.1. Results of Chronic Disease Management Studies
A substantial portion of the reviewed studies focused on the use of AI and IoT technologies in chronic disease management, particularly in diabetes and cardiovascular disease (CVD). The data extracted from 40 studies on diabetes and 25 studies on CVD revealed several positive outcomes (Table 3).
4.1.1. Diabetes Management
In 40 studies examining the use of AI and IoT systems for diabetes management, the integration of continuous glucose monitors (CGMs) with AI algorithms resulted in significant improvements in patient outcomes. The studies reported an average reduction of 0.9% in HbA1c levels, a key indicator of long-term glucose control, which was statistically significant (p ~ 0.01). This improvement was driven by real-time glucose monitoring and the automatic adjustment of insulin doses through smart insulin pumps, reducing complications like hyperglycemia and hypoglycemia.
Additionally, the studies demonstrated a 15% reduction in hospital admissions for patients utilizing AI and IoT systems due to better glycemic control. This reduction was also statistically significant (p ~ 0.02), indicating the long-term benefit of these technologies in managing diabetes and minimizing the need for hospitalization.
4.1.2. Cardiovascular Disease (CVD) Monitoring
In 25 studies focused on cardiovascular disease management, wearable ECG monitors equipped with AI algorithms enabled the early detection of heart arrhythmias and other abnormalities, leading to a 25% improvement in detection accuracy compared to traditional methods (p ~ 0.03). These improvements allowed for earlier intervention, reducing the likelihood of serious cardiac events.
Furthermore, AI-based diagnostic tools reduced the time required to diagnose cardiovascular conditions by 20-30%, with studies showing statistically significant results (p ~ 0.04). The ability to quickly and accurately detect cardiovascular risks is crucial for timely treatment and better patient outcomes.
4.2. Results of Pandemic Response Studies
The second major category of studies reviewed involved the use of AI and IoT technologies in pandemic management, with a particular focus on COVID-19. A total of 28 studies assessed the effectiveness of AI-driven diagnostic tools and IoT-based remote monitoring systems in reducing the burden on healthcare systems during the pandemic (Table 4).
4.2.1. COVID-19 Diagnostics
AI and IoT technologies played a crucial role in supporting healthcare systems during the COVID-19 pandemic. In 28 studies on AI-driven diagnostics, tools for analyzing medical imaging (e.g., CT scans and chest X-rays) reduced the time required for COVID-19 diagnosis by an average of 35%. The use of AI algorithms to detect signs of pneumonia and other complications related to COVID-19 was highly effective, with results showing statistical significance (p ~ 0.003).
4.2.2. Remote Patient Monitoring and Hospital Admission Reduction
IoT-based remote monitoring systems enabled the real-time tracking of patient vital signs, such as oxygen saturation, body temperature, and heart rate. This approach allowed healthcare providers to monitor patients outside the hospital, reducing the need for in-person visits and hospitalizations. The studies reported a 20% reduction in hospital admissions, particularly among high-risk patients, with statistically significant results (p ~ 0.02).
4.2.3. Resource Optimization
In addition to diagnostic benefits, AI systems were used to optimize the allocation of healthcare resources during the pandemic. Predictive AI models helped forecast patient surges and prioritize the distribution of critical resources, such as ventilators and ICU beds. Studies reported a 25% increase in hospital resource utilization efficiency, with statistical significance (p ~ 0.04).
4.3. Overarching Trends and Benefits
The review found several overarching trends across the literature on AI and IoT in healthcare. These trends highlight the broad impact of these technologies on healthcare outcomes, efficiency, and costs (Table 5).
4.3.1. Diagnostic Accuracy and Cost Efficiency
Across both chronic disease management and pandemic response, AI-enhanced diagnostic tools resulted in a 15-25% improvement in diagnostic accuracy, particularly for diseases such as diabetes, cardiovascular conditions, and COVID-19. These improvements were statistically significant (p < 0.05) and led to faster, more accurate diagnoses, reducing diagnostic errors.
Moreover, the adoption of IoT-enabled remote monitoring systems contributed to a 15-20% reduction in healthcare costs. This was largely driven by the decreased need for hospital admissions and the more efficient use of healthcare resources, as patients could be monitored and treated remotely. These results were statistically significant (p < 0.05), indicating that AI and IoT technologies have the potential to alleviate financial pressure on healthcare systems.
4.3.2. Patient Engagement
In addition to clinical outcomes, the integration of IoT devices and AI algorithms led to a 20% increase in patient engagement and adherence to treatment plans. Real-time feedback provided by wearable devices encouraged patients to stay on track with their treatments, improving overall health outcomes. This improvement was statistically significant (p < 0.05).
4.4. Challenges and Limitations
Despite the clear benefits of AI and IoT technologies in healthcare, several challenges were identified across the studies:
- Data Privacy and Security: 30% of studies raised concerns about data security risks associated with IoT devices, highlighting the need for better security protocols.
- Algorithmic Bias: AI models trained on non-representative datasets exhibited bias, resulting in unequal healthcare outcomes for different demographic groups.
- Cost of Implementation: Initial implementation costs were cited as a barrier in 45% of studies, particularly in low-resource settings, despite the long-term cost-saving benefits.
In summary, the results demonstrate that AI and IoT technologies have led to significant improvements in chronic disease management, pandemic response, and overall healthcare efficiency. The quantitative outcomes summarized in this review indicate substantial benefits, including improved diagnostic accuracy, cost reductions, and increased patient engagement. However, addressing challenges such as data security, algorithmic bias, and implementation costs will be essential for widespread adoption.
5. Applications of AI and IoT in Healthcare
The implementation of Artificial Intelligence (AI) and the Internet of Things (IoT) in healthcare has led to significant advancements in patient monitoring, clinical decision-making, and operational efficiency. These technologies are being applied across a range of healthcare domains, including chronic disease management, telemedicine, and smart hospital infrastructures, bringing about more efficient and personalized healthcare solutions.
5.1. Smart Healthcare Devices and Remote Monitoring
AI and IoT-enabled devices, such as wearable sensors and smart health monitoring systems, have transformed how patients with chronic diseases are managed. These devices continuously collect health data, such as heart rate, blood glucose levels, and respiratory function, which are analyzed by AI algorithms to provide real-time insights and early warnings for both patients and clinicians.
Table 6. summarizes the key applications of AI and IoT in chronic disease management and
their measurable outcomes, demonstrating how these technologies improve patient care and
management:.
These technologies provide significant benefits, such as 0.9% reductions in HbA1c levels for diabetes patients and 25% improvements in arrhythmia detection for cardiovascular disease management, as illustrated in Table 6. They have also been instrumental in managing chronic respiratory diseases through the use of smart inhalers that enhance medication adherence and reduce hospital visits.
5.1.1. Wearable Devices for Chronic Disease Management
Wearable devices such as continuous glucose monitors (CGMs) and ECG sensors are playing a critical role in the management of chronic conditions like diabetes and cardiovascular disease. AI algorithms integrated with CGMs predict glucose fluctuations and adjust insulin doses accordingly, improving glycemic control and reducing the risk of complications. Studies show that AI-powered CGM systems can reduce HbA1c levels by an average of 0.9% in diabetic patients, significantly improving patient outcomes [52,53].
In cardiovascular care, AI-enabled ECG monitors are used to detect arrhythmias and other cardiac abnormalities in real time, reducing the time to diagnosis and allowing for early intervention. A recent meta-analysis found that the use of AI-driven cardiovascular monitoring systems improved the early detection of arrhythmias by 25%, leading to earlier treatment and better patient outcomes [57,58].
5.1.2. Remote Monitoring for Elderly and Vulnerable Populations
Remote monitoring systems using IoT devices, such as wearable fall detectors and vital sign trackers, have become essential tools for monitoring elderly and vulnerable populations. These systems provide real-time alerts to caregivers and healthcare providers, enabling rapid responses to emergencies. Studies have shown that integrating AI into these systems allows for more accurate detection of health deterioration, which is critical in providing timely interventions [62].
Moreover, AI-powered smart homes for elderly care are equipped with IoT devices that monitor daily activities and detect deviations from normal behavior, such as changes in sleep patterns or mobility, helping to prevent falls and other health issues [63].
5.2. Telemedicine and Virtual Healthcare
The COVID-19 pandemic has accelerated the adoption of telemedicine, with AI and IoT technologies being central to this shift. Remote monitoring devices combined with AI-driven platforms enable clinicians to provide virtual care to patients, ensuring continuity of care without requiring in-person visits.
As summarized in Table 7, AI and IoT have been key in enabling telemedicine applications such as remote consultations and COVID-19 monitoring, where IoT-enabled devices like pulse oximeters helped reduce hospital admissions.
For instance, IoT-enabled pulse oximeters used in COVID-19 monitoring allowed clinicians to assess patient health remotely, significantly reducing hospital admissions [64,65,66]. Additionally, AI-powered virtual health assistants improved diagnostic accuracy by 15% during remote consultations by processing real-time data from IoT devices and providing insights to clinicians, as noted in Table 7 [66,67,68].
5.2.1. IoT-Enabled Remote Consultations
IoT-enabled devices, such as smart thermometers, digital stethoscopes, and connected pulse oximeters, have been widely used in telemedicine to gather real-time patient data during remote consultations. These devices transmit data to healthcare providers, allowing them to make informed decisions remotely. During the pandemic, IoT-enabled pulse oximeters were used to monitor COVID-19 patients' oxygen saturation levels, significantly reducing the need for hospital admissions for mild cases [70].
5.2.2. AI-Driven Telemedicine Platforms
AI-enhanced telemedicine platforms use natural language processing (NLP) to interact with patients, guide them through symptom checkers, and provide personalized health recommendations. These platforms analyze real-time data collected from IoT devices to identify potential health risks and flag them for clinicians. A study reported that AI-powered telemedicine platforms increased diagnostic accuracy by 15% during remote consultations, enhancing the quality of care provided [71,72].
5.3. AI-Enhanced Diagnostics and Imaging
AI is making substantial contributions to the field of medical imaging and diagnostics. By analyzing images from CT scans, MRIs, and X-rays, AI algorithms can identify subtle patterns and anomalies that may not be visible to the human eye. The combination of AI with IoT-connected imaging devices enhances diagnostic accuracy and speeds up clinical workflows.
A visual overview of AI and IoT integration in healthcare, shown in Figure 5, highlights the interaction between wearable health devices, AI algorithms, and clinical workflows. The figure illustrates how patient data is collected via IoT devices, analyzed by AI systems, and then used to support clinical decision-making.
In addition to diagnostics, AI-driven predictive analytics are also playing a crucial role in identifying disease risks and progression. For example, AI-based predictive models used for cardiovascular disease management have been shown to reduce hospital readmissions by 20%, helping healthcare providers intervene before complications arise [73].
5.3.1. Medical Imaging and AI Algorithms
AI algorithms are increasingly used in radiology to assist in diagnosing conditions such as cancer and cardiovascular diseases. Studies have demonstrated that AI-assisted imaging tools can improve diagnostic accuracy by 15-25% in identifying early-stage cancers from CT scans and MRIs, reducing the risk of misdiagnosis [74,75,76].
5.3.2. Predictive Analytics for Early Detection
AI-driven predictive models use data from IoT devices and electronic health records (EHRs) to predict disease onset and progression. In chronic disease management, AI algorithms analyze patient data to forecast potential complications, enabling early interventions that can prevent hospitalizations. For instance, AI-based predictive models for cardiovascular diseases have been shown to reduce hospital readmissions by 20% by accurately predicting patients at high risk of deterioration [77,78,79,80].
5.4. Smart Hospitals and Healthcare Automation
Hospitals are leveraging AI and IoT technologies to create smart healthcare environments, improving both patient care and operational efficiency. These smart hospitals use interconnected devices to monitor patients, manage resources, and streamline administrative tasks.
In smart hospitals, IoT-enabled beds and vital sign monitors track patient data in real time, sending alerts to healthcare staff if any critical changes are detected. AI systems then analyze this data to predict potential complications such as sepsis or respiratory failure, allowing for preventive care and improving patient outcomes [81,82,83]. Figure 6 provides an illustration of how these smart systems function in a hospital setting.
5.4.1. Real-Time Patient Monitoring and Alerts
In smart hospitals, IoT-enabled beds and vital sign monitors track patient data in real time, sending alerts to healthcare staff if any critical changes are detected. AI systems then analyze this data to predict potential complications such as sepsis or respiratory failure, allowing for preventive care and improving patient outcomes [84,85,86,87].
5.4.2. Automation of Administrative and Logistical Tasks
AI and IoT are also being used to automate hospital operations, such as scheduling, inventory management, and resource tracking. For example, IoT sensors embedded in medical equipment help track the availability and location of critical devices, ensuring that they are always accessible when needed. AI systems can also optimize surgical schedules and allocate resources based on predicted patient flow, improving overall efficiency [88,89,90,91,92].
5.5. Future Potential and Emerging Applications
Looking ahead, AI and IoT technologies hold great promise in areas such as genomic medicine, robotics, and mental health. In precision medicine, AI algorithms can analyze genomic data to predict disease susceptibility and personalize treatments. Additionally, IoT-based wearables that track behavioral and physiological markers are being developed to monitor mental health conditions such as depression and anxiety, providing real-time feedback to both patients and clinicians [80,93,94,95].
In summary, AI and IoT technologies are reshaping healthcare by enabling smart medical devices, remote monitoring, and AI-enhanced diagnostics. These applications improve patient outcomes, reduce healthcare costs, and optimize hospital operations. However, for these technologies to reach their full potential, challenges such as data privacy, regulatory compliance, and interoperability must be addressed.
6. Case Studies of AI and IoT in Chronic Disease Management
The integration of AI and IoT technologies has made significant advancements in managing chronic diseases such as diabetes, cardiovascular diseases, chronic obstructive pulmonary disease (COPD), and chronic kidney disease (CKD). Through real-time monitoring, predictive analytics, and personalized interventions, AI and IoT are transforming chronic disease management and improving patient outcomes. This section presents key case studies illustrating the practical application and impact of these technologies.
6.1. AI-Driven Continuous Glucose Monitoring for Diabetes
AI-enhanced continuous glucose monitors (CGMs) are one of the most successful implementations of AI and IoT in chronic disease management. These systems allow real-time tracking of glucose levels, enabling timely interventions to prevent complications such as hyperglycemia and hypoglycemia.
Case Study: AI-Enhanced Glucose Monitoring Systems
In a clinical trial by Haidar et al. (2015), AI-enhanced continuous glucose monitors (CGMs) were used to predict glucose fluctuations and automatically adjust insulin delivery in diabetic patients. The CGM devices transmitted real-time glucose data to an AI system, which analyzed the data using predictive models. Patients using this system experienced a 0.9% reduction in HbA1c levels, fewer hypoglycemic episodes, and improved overall glycemic control. The AI system was able to learn from individual patient data and predict future glucose trends, making it an effective tool for managing diabetes. Moreover, this technology reduced the burden on healthcare providers by providing real-time insights and automating insulin delivery adjustments [96]. This system also reduced the burden on healthcare providers by offering real-time insights and automating insulin adjustments, as shown in Figure 7.
6.2. AI and IoT for Cardiovascular Disease Management
In the management of cardiovascular diseases (CVD), continuous monitoring of vital signs such as heart rate, blood pressure, and oxygen saturation is critical. AI and IoT technologies have significantly advanced real-time monitoring and early detection of heart conditions, reducing the risk of fatal events.
Case Study: AI-Based ECG Monitors
A study by Hickey et al. (2019) implemented AI-enabled wearable ECG monitors to continuously monitor patients at risk of arrhythmias. The wearable devices collected heart activity data in real time and transmitted it to a central AI system, which used machine learning algorithms to detect irregularities in the heart’s rhythm. The AI system predicted arrhythmias with 93% accuracy, leading to a 32% improvement in early detection compared to traditional ECG monitoring methods. This timely intervention significantly reduced hospitalizations and allowed patients to avoid more invasive diagnostic procedures [97]. Figure 8 illustrates how AI-based ECG monitors streamline cardiovascular disease management by continuously analyzing patient data in real-time.
6.3. COPD Management Through IoT-Connected Smart Inhalers
Patients with chronic obstructive pulmonary disease (COPD) benefit significantly from IoT-connected smart inhalers that monitor medication adherence and provide real-time feedback. These devices improve adherence and reduce the likelihood of exacerbations, which are a leading cause of hospital admissions in COPD patients.
Case Study: Smart Inhalers with Predictive Analytics
In a study focused on IoT-connected smart inhalers for COPD management, patients used inhalers equipped with sensors that tracked their usage and sent real-time data to an AI platform. The AI system analyzed the data to predict exacerbations by observing medication adherence patterns and respiratory function. Personalized reminders were sent to patients, while healthcare providers were alerted to potential risks of exacerbation. Studies like those by Akduman et al. (2024), Margam et al. (2024) have shown that the use of smart inhalers leads to a reduction in hospital admissions by approximately 30-40% [98,99], and studies like those by Alex et al. (2024), Margam et al. (2024) have shown that improvements in medication adherence by 15-20% [99,100]. Such systems significantly improve the management of chronic conditions like COPD by ensuring better patient compliance and proactive healthcare interventions. This case highlights how predictive analytics, combined with IoT devices, can effectively manage chronic diseases, as summarized in Figure 9.
6.4. Remote Monitoring and AI in Heart Failure Management
Heart failure requires continuous monitoring of key metrics like weight, blood pressure, and heart rate to prevent exacerbations. AI-powered remote monitoring systems using IoT-enabled devices have been shown to reduce hospital readmissions by predicting exacerbations before symptoms become severe.
Case Study: AI-Powered Remote Monitoring for Heart Failure
In a clinical study by Stehlik et al. (2020), heart failure patients were monitored using IoT devices that collected vital signs, such as weight and blood pressure, in real time. The data was transmitted to an AI platform that predicted exacerbations based on changes in these metrics. This system allowed healthcare providers to adjust treatment plans proactively, reducing hospital readmissions by 20% and improving patient outcomes. Patients reported fewer emergency interventions and a higher quality of life, as they could manage their condition more effectively with AI-driven insights [101]. This case demonstrates the value of AI and IoT in improving heart failure management and reducing the burden on healthcare systems.
6.5. AI and IoT for Chronic Kidney Disease (CKD) Management
Chronic kidney disease (CKD) is a progressive condition that requires close monitoring to prevent its advancement to end-stage renal disease. AI and IoT technologies enable real-time monitoring of renal function, helping to slow disease progression and reduce complications.
Case Study: Remote Monitoring for CKD Patients
In a study by Rovin et al. (2021), chronic kidney disease (CKD) patients were equipped with IoT-enabled sensors that monitored key indicators such as blood pressure, proteinuria, and glomerular filtration rate (GFR). The data collected was analyzed by AI algorithms to predict disease progression and inform treatment adjustments. Patients who used these systems experienced a 30% slower progression of CKD compared to those receiving standard care, as early detection of renal function changes allowed for timely interventions [102]. This case illustrates how AI and IoT technologies can optimize CKD management and improve patient outcomes.
The Table 8 below summarizes the outcomes of the case studies described in this section.
As outlined in Table 8, the benefits of AI and IoT technologies are clearly demonstrated in managing chronic diseases such as diabetes, cardiovascular disease, COPD, heart failure, and CKD. These technologies have shown measurable improvements in patient outcomes, from reducing hospital admissions to slowing disease progression.
In summary, the case studies presented in this section demonstrate the practical and transformative impact of AI and IoT technologies in the management of chronic diseases. By providing real-time monitoring, predictive analytics, and personalized interventions, these technologies have significantly improved patient outcomes and reduced hospital admissions. As AI and IoT continue to evolve, their application in chronic disease management will become more widespread, further enhancing healthcare delivery and patient quality of life.
7. Discussion
The convergence of Artificial Intelligence (AI) and Internet of Things (IoT) technologies is reshaping the landscape of chronic disease management, with IoT-connected smart inhalers for Chronic Obstructive Pulmonary Disease (COPD) being a prime example of this revolution. This discussion critically examines the transformative impact of these systems, contextualizing the findings within broader healthcare trends, while also addressing the implementation barriers, clinical limitations, and future research directions that must be navigated to fully realize their potential.
Impact of AI and IoT on Chronic Disease Management
The introduction of AI-powered IoT devices has marked a paradigm shift in COPD management, where real-time monitoring, predictive analytics, and personalized feedback loops are enabling a more proactive, patient-centered approach to healthcare. As evidenced by multiple studies, including those by Akduman et al. (2024) and Margam et al. (2024), these systems have demonstrated the ability to reduce hospital admissions by 30-40% [98,99] and Alex et al. (2024) and Margam et al. (2024) improved medication adherence by 15-20% [99,100], underscoring the efficacy of AI-driven interventions in preventing exacerbations and optimizing treatment adherence.
The underlying advantage of AI lies in its capacity to analyze vast quantities of patient data, identifying subtle patterns that may not be apparent to human clinicians. For COPD patients, who often present with complex, multi-factorial disease trajectories, the ability to predict exacerbations based on historical medication use, respiratory function, and even environmental factors (e.g., air quality, weather patterns) presents a significant leap forward in preventive care. This not only improves patient outcomes but also reduces the strain on healthcare systems by shifting the focus from reactive interventions to preemptive management. Importantly, such benefits align with the broader goal of value-based care—a transition away from volume-driven healthcare to one that prioritizes health outcomes and cost-effectiveness.
Implementation Barriers and Technological Challenges
Despite these promising outcomes, several significant barriers continue to impede the widespread adoption and scalability of AI-IoT solutions in real-world clinical settings. Data security and privacy concerns rank foremost among these challenges, particularly given the sensitive nature of health data. IoT devices continuously transmit patient-specific information, including physiological measurements and adherence data, raising the risk of data breaches and misuse. Although encryption technologies and blockchain-based data management systems have been proposed as potential solutions, their deployment remains limited, especially in resource-constrained settings where technological infrastructure is lacking.
Equally pressing is the issue of interoperability. Many AI-powered IoT devices operate within proprietary ecosystems that do not easily integrate with existing Electronic Health Records (EHR) systems, creating data silos that hinder seamless information exchange. For healthcare providers to benefit fully from AI insights, these technologies must interface with established clinical workflows without adding additional layers of complexity. Recent initiatives, such as the development of FHIR (Fast Healthcare Interoperability Resources) standards, offer promising frameworks for facilitating data exchange across systems, but adoption remains inconsistent.
From a clinical perspective, there are also concerns about the generalizability of AI models. As noted in studies like Hickey et al. (2019), AI algorithms are often trained on narrow datasets that may not reflect the full diversity of COPD patients [97]. This creates the risk of algorithmic bias, where certain demographic groups—such as those with comorbidities, older adults, or populations with limited healthcare access—are underrepresented in training data, leading to suboptimal predictions. Addressing these biases will require a concerted effort to build more inclusive datasets and refine AI algorithms to account for heterogeneous patient populations.
Clinical Implications and Ethical Considerations
Beyond technical hurdles, there are profound ethical considerations associated with the use of AI in COPD management. While AI systems offer valuable decision-making support, there is a risk of over-reliance on algorithmic outputs at the expense of clinical judgment. This introduces concerns regarding accountability in medical decision-making. Who bears responsibility when an AI system provides erroneous predictions that lead to adverse patient outcomes? Regulatory bodies must therefore establish clearer guidelines that delineate the role of AI as a support tool rather than a primary decision-maker, ensuring that clinicians retain oversight over patient care.
Moreover, patient autonomy and consent must remain central to the deployment of AI-IoT systems. Patients need to be fully informed about how their data is being used, who has access to it, and the potential risks and benefits of AI-driven interventions. Transparent communication between healthcare providers and patients is essential to build trust and encourage patient engagement with these technologies.
Future Directions for Research and Development
Looking forward, the next wave of innovation will likely focus on the synergistic integration of AI-IoT systems with emerging fields such as genomics, biomarkers, and precision medicine. By incorporating genomic data into AI models, healthcare providers could develop more personalized treatment strategies that consider not only the patient’s respiratory function but also their genetic predisposition to COPD progression. Such multi-dimensional approaches could significantly enhance the predictive power of AI systems, providing earlier and more accurate interventions.
Another promising area for future research lies in the scalability of AI-IoT solutions across diverse healthcare settings. While the efficacy of smart inhalers has been proven in controlled clinical trials, their deployment in low-resource environments remains limited. Developing low-cost, scalable IoT devices that can function in regions with limited infrastructure will be essential for addressing global health disparities, particularly as the burden of COPD continues to grow in lower-income countries. Collaboration between public health institutions, private companies, and regulatory agencies will be key to driving this scalability.
Finally, attention must be given to improving patient engagement with AI-IoT systems. As studies by Stehlik et al. (2020) suggest, sustained patient interaction with these technologies is critical for long-term adherence and efficacy [101]. Future AI systems could leverage behavioral science to provide more personalized and motivating feedback, encouraging patients to take a more active role in managing their health.
In summary, the integration of AI and IoT technologies into COPD management offers unprecedented opportunities to improve patient outcomes through real-time monitoring, predictive analytics, and personalized interventions. However, to fully unlock the potential of these technologies, healthcare stakeholders must address key barriers, including data security, interoperability, and algorithmic biases. The future of COPD care will depend on a delicate balance between technological innovation and ethical, patient-centered healthcare practices. By overcoming these challenges, AI-IoT systems have the potential to transform chronic disease management, leading to more equitable, efficient, and personalized care for patients worldwide.
8. Challenges and Limitations of AI and IoT Integration in Healthcare
While the integration of Artificial Intelligence (AI) and Internet of Things (IoT) technologies holds significant promise for transforming healthcare, their deployment in real-world clinical settings faces several technical, regulatory, and ethical challenges. This section critically explores the key obstacles to the widespread adoption of AI-IoT systems in healthcare, focusing on data privacy, interoperability, algorithmic bias, regulatory hurdles, and cost barriers.
8.1. Data Privacy, Security, and Ethical Concerns
A primary concern in the implementation of AI-IoT systems is the privacy and security of health data. IoT devices, such as smart inhalers for COPD management, continuously monitor and transmit sensitive patient data, including medication adherence and physiological metrics, to AI platforms for analysis. This raises significant concerns about potential data breaches and misuse, particularly in light of the increasing number of cyberattacks on healthcare systems globally. In 2020 alone, the U.S. healthcare sector reported over 500 data breaches, exposing 26 million patient records [103].
The application of blockchain technology has been proposed as a solution to enhance data security and integrity by decentralizing health data storage, making it less vulnerable to tampering [104]. However, its integration with existing healthcare infrastructures remains challenging due to the technical complexity and high cost of implementation.
In addition, the ethical concerns surrounding informed consent and patient autonomy remain unresolved. Many patients are unaware of how their data is being processed, who has access to it, and whether third-party entities can use it for purposes beyond medical care. GDPR in the EU provides stringent protections, but regulatory frameworks in other regions are often less robust, leading to ethical inconsistencies in patient data management [105].
8.2. Interoperability and Integration with Existing Systems
Another significant challenge lies in the lack of interoperability between AI-IoT devices and existing Electronic Health Record (EHR) systems. Many IoT devices, including smart inhalers, operate on proprietary software, creating data silos that hinder seamless information exchange across different healthcare systems. This lack of integration reduces the clinical utility of AI-generated insights, as they cannot be easily incorporated into the daily workflows of healthcare providers [106].
Efforts to establish standardized communication protocols, such as FHIR (Fast Healthcare Interoperability Resources), are critical to solving this problem. However, global adoption of these standards is still in its infancy, and healthcare institutions with legacy systems face significant technical and financial barriers to upgrading their infrastructures. Table 9 below summarizes the current state of AI-IoT interoperability across different healthcare systems.
8.3. Algorithmic Bias and Generalizability
A well-documented limitation in AI models is the risk of algorithmic bias, which occurs when the data used to train AI systems is not representative of the diverse populations served by healthcare systems. Studies have shown that many AI models used in healthcare are trained on datasets predominantly sourced from high-income countries, leading to biased predictions that do not account for differences in genetics, environmental exposures, and comorbidities present in other populations [107].
For instance, AI systems used in the management of COPD may underperform in detecting exacerbations among racial minorities or rural populations, who are often underrepresented in clinical datasets. Addressing this issue requires multinational collaborations to curate diverse training datasets that capture the full range of patient demographics, including age, gender, ethnicity, and socioeconomic status [108]. Moreover, integrating continuous learning algorithms that update predictions based on new data can help improve the generalizability of AI systems over time [86].
Table 10 presents a summary of common sources of algorithmic bias and potential solutions to mitigate these biases.
8.4. Regulatory and Legal Challenges
The regulatory landscape for AI in healthcare remains highly fragmented, with few clear guidelines on the development, deployment, and oversight of AI-IoT systems. Regulatory agencies, such as the U.S. Food and Drug Administration (FDA) and the European Medicines Agency (EMA), have struggled to develop adaptive frameworks that can monitor the dynamic nature of AI systems, particularly those that evolve through continuous learning. Existing approval processes, designed for static medical devices, are often ill-suited to evaluate the ongoing safety and efficacy of AI algorithms that adjust based on new patient data [109].
Moreover, the question of legal accountability remains unresolved. If an AI system makes an incorrect prediction leading to patient harm, it is unclear whether responsibility lies with the software developers, the healthcare providers using the system, or the institutions that deployed it. Legal frameworks must evolve to address these uncertainties and ensure that accountability mechanisms are in place to protect both patients and providers.
8.5. Cost and Accessibility Barriers
The high cost of AI-IoT technologies poses another significant barrier to their widespread adoption, particularly in low-resource healthcare settings. The implementation of AI systems often requires substantial investment in data infrastructure, training, and maintenance, which many healthcare providers are unable to afford [110]. Additionally, the cost of IoT-enabled medical devices such as smart inhalers remains prohibitive for many patients, especially those in low- and middle-income countries (LMICs), where the burden of chronic diseases like COPD is rising most rapidly [27].
To address this issue, governments and international health organizations must play an active role in subsidizing the deployment of AI-IoT technologies in underserved regions. Public-private partnerships could also help drive down the cost of these devices by incentivizing manufacturers to produce more affordable, scalable solutions. Ensuring equitable access to AI-driven healthcare technologies is critical to preventing a widening digital divide between high-income and low-income regions.
In summary, while the integration of AI and IoT technologies offers tremendous potential for improving healthcare outcomes, significant challenges remain. Issues related to data privacy, interoperability, algorithmic bias, regulatory oversight, and cost must be addressed to ensure that these systems can be deployed effectively and equitably. Collaborative efforts among policymakers, technologists, healthcare providers, and regulatory bodies will be essential to overcoming these challenges and unlocking the full potential of AI-IoT integration in healthcare. Moving forward, addressing these barriers is crucial to ensuring that AI-IoT systems not only improve patient outcomes but also contribute to a more inclusive and resilient healthcare ecosystem.
9. Future Directions
The future of Artificial Intelligence (AI) and Internet of Things (IoT) integration in healthcare holds immense potential for revolutionizing patient care, with the capability to significantly enhance disease management, optimize clinical workflows, and improve overall healthcare efficiency. However, realizing this potential requires addressing existing barriers and advancing the technology further to meet the growing demands of complex healthcare systems. This section explores key areas that are likely to shape the future of AI and IoT in healthcare, with a particular focus on expanding the application of smart inhalers for COPD management and extending these innovations to broader chronic disease management.
9.1. Multi-Dimensional Data Integration: Genomics, Biomarkers, and Beyond
One of the most exciting future directions is the integration of multi-dimensional data into AI-IoT systems, including genomic, biomarker, and environmental data. Currently, smart inhalers and similar IoT-enabled devices primarily focus on tracking physiological metrics and medication adherence. However, incorporating genomic data could revolutionize the field by enabling precision medicine approaches. By analyzing a patient’s genetic makeup alongside real-time physiological data, AI systems could offer highly personalized treatment recommendations, predicting how individuals might respond to different treatments based on their unique biological profiles [111].
Additionally, integrating biomarkers—such as inflammatory markers or exhaled nitric oxide—with AI algorithms could provide more accurate assessments of disease severity in COPD patients. These biomarkers can serve as early indicators of exacerbations or deteriorations, further enhancing the AI’s predictive power. Combining sensor-based data from IoT devices with molecular and clinical data represents a key next step in creating holistic disease management platforms (Table 11).
9.2. Real-Time Predictive Analytics and Decision Support
AI systems in healthcare are increasingly moving towards real-time predictive analytics, which not only monitor a patient’s current condition but also forecast future health events with high accuracy. In the case of COPD, real-time analytics could enable early warning systems that predict exacerbations before they occur, based on a combination of historical data, sensor feedback, and AI-driven pattern recognition [112]. These predictive capabilities will allow healthcare providers to proactively intervene, adjusting medication dosages or scheduling timely medical check-ups to prevent hospitalizations.
Beyond COPD, this real-time analytics capability can be extended to other chronic diseases, such as cardiovascular diseases, diabetes, and asthma, where predictive models can anticipate acute episodes based on continuous data streams from IoT devices. Additionally, integrating AI decision support systems with real-time analytics will enhance clinical decision-making by offering healthcare providers tailored, data-driven recommendations at the point of care. These recommendations, when synchronized with Electronic Health Records (EHRs), can ensure that patients receive more timely and appropriate interventions.
9.3. Enhancing Scalability and Accessibility of AI-IoT Systems
One of the critical challenges currently limiting the widespread adoption of AI-IoT systems, particularly in low-resource settings, is the lack of scalable and cost-effective solutions. In the future, a concerted effort will be required to reduce the costs of IoT-enabled devices and the computational infrastructure needed to support AI analytics, enabling wider accessibility. Open-source AI platforms, along with modular, plug-and-play IoT devices, could offer one solution by allowing healthcare providers in low- and middle-income countries to integrate AI-driven healthcare systems without the need for significant upfront investments [101].
Scaling these technologies also demands improved interoperability standards. While Fast Healthcare Interoperability Resources (FHIR) is a step in the right direction, there is a need for a global standard that ensures seamless integration across different health systems, IoT devices, and AI platforms. Future research should focus on developing interoperable frameworks that facilitate the integration of AI and IoT solutions across diverse healthcare ecosystems, enabling more equitable access to cutting-edge technologies. This is particularly crucial for ensuring AI-IoT scalability in low-resource environments (Table 12).
9.4. Advanced AI Learning Models and Personalization
The evolution of AI learning models—from static algorithms to continuous learning and reinforcement learning systems—will play a crucial role in the future of healthcare. Current AI systems typically rely on static datasets to make predictions, but future systems will be designed to continuously learn from new patient data, refining their predictions and recommendations over time. This will lead to more accurate and personalized healthcare interventions, particularly for chronic diseases where patient needs evolve.
For example, in COPD management, AI systems could adapt to individual patients’ changing health statuses by analyzing their longitudinal health data and updating their predictive models accordingly. Reinforcement learning techniques could also enable AI systems to optimize treatment regimens based on continuous feedback, improving not only adherence but also overall treatment outcomes. By learning from real-world data in real time, these AI systems will be better equipped to manage the complex, dynamic nature of chronic diseases, providing more tailored and effective interventions [86].
9.5. Ethical AI and Governance
As AI and IoT technologies become more pervasive in healthcare, addressing the ethical and governance challenges associated with these systems will be paramount. Algorithmic transparency, bias mitigation, and data privacy will continue to be significant concerns. Future AI-IoT systems must be designed with explainability in mind, ensuring that clinicians understand how AI models make predictions and decisions, and allowing patients to trust the recommendations provided.
Governments, healthcare providers, and regulatory bodies must work together to develop ethical frameworks for AI-IoT systems that prioritize patient rights and data sovereignty. This will likely involve the establishment of AI ethics boards within healthcare institutions, tasked with overseeing the deployment and management of AI systems, ensuring that they align with patient safety, equity, and ethical guidelines [113].
9.6. Cross-Disease Applications and Multi-Morbidity Management
The future of AI-IoT integration is not limited to COPD but extends to a wide range of chronic diseases that often coexist in patients. The growing prevalence of multi-morbidity—where patients suffer from more than one chronic condition simultaneously—necessitates AI systems that can manage multiple diseases in parallel. For instance, many COPD patients also suffer from heart failure or diabetes, both of which require continuous monitoring and complex medication regimens. AI systems capable of managing multiple disease states through a single IoT platform will provide patients with a more cohesive and less fragmented care experience.
By integrating IoT data from various devices (e.g., smart inhalers, continuous glucose monitors, wearable ECGs), AI systems will be able to provide a holistic view of a patient’s health, offering insights into how one condition may affect another. This cross-disease application will be crucial in improving the quality of care for elderly patients and others with multi-morbid conditions, reducing the burden on healthcare systems while improving patient outcomes.
In summary, the future of AI and IoT in healthcare is rich with opportunities for innovation and advancement. By incorporating multi-dimensional data, enhancing real-time predictive analytics, and improving the scalability and personalization of AI systems, healthcare providers will be better equipped to manage complex, chronic diseases like COPD. However, realizing this potential will require overcoming challenges related to cost, accessibility, interoperability, and ethical governance. Future research and development efforts should focus on creating equitable, patient-centered AI-IoT systems that are capable of evolving alongside the needs of healthcare systems and the populations they serve. As we move forward, the careful integration of these technologies will pave the way for a more intelligent, personalized, and proactive healthcare future.
10. Conclusions
The integration of Artificial Intelligence (AI) and the Internet of Things (IoT) represents a major leap forward in chronic disease management and healthcare delivery. This review highlights the transformative potential of these technologies, particularly in managing complex conditions like diabetes, cardiovascular disease, and COPD, where AI-powered predictive models and IoT-enabled devices have demonstrated significant improvements in patient outcomes. The use of AI-driven continuous glucose monitors and wearable ECG monitors, for instance, has led to measurable improvements in glycemic control and early detection of cardiovascular anomalies, reducing hospital admissions and mortality rates. Additionally, IoT-enabled systems have proven invaluable in pandemic response, offering real-time patient monitoring and resource optimization during the COVID-19 crisis.
However, the widespread adoption of AI and IoT technologies in healthcare is hindered by several challenges, including data privacy concerns, algorithmic bias, and the high costs of implementation. These barriers, if unaddressed, could limit the scalability and accessibility of these innovations, particularly in low-resource settings. The future of healthcare will require a concerted effort to develop more inclusive AI models, enhance interoperability across health systems, and establish robust regulatory frameworks to ensure ethical AI deployment. As AI and IoT continue to evolve, they hold the promise of delivering more personalized, efficient, and equitable healthcare solutions. By addressing the technical and ethical challenges outlined in this review, these technologies have the potential to reshape the future of healthcare, improving patient outcomes and alleviating the burden on healthcare systems worldwide.
References
- Aftab, M. , et al., Advancements and Challenges in Artificial Intelligence Applications in Healthcare Delivery Systems. 2024.
- Moharana, M. , et al., Smart Healthcare Systems in Combating Infectious Diseases Outbreaks, in Smart Medical Imaging for Diagnosis and Treatment Planning. 2025, Chapman and Hall/CRC. p. 157-175.
- Shafik, W. , Artificial Intelligence-Enabled Internet of Medical Things (AIoMT) in Modern Healthcare Practices, in Clinical Practice and Unmet Challenges in AI-Enhanced Healthcare Systems. 2024, IGI Global. p. 42-69.
- Singh, P. , AI Strategies for Delivering Better Value in the Healthcare Sector, in Revolutionizing the Healthcare Sector with AI. 2024, IGI Global. p. 131-156.
- Thakare, V., G. Khire, and M. Kumbhar, Artificial intelligence (AI) and internet of things (IoT) in healthcare: Opportunities and challenges. ECS Transactions, 2022. 107(1): p. 7941.
- Yekaterina, K. , Challenges and Opportunities for AI in Healthcare. International Journal of Law and Policy, 2024. 2(7): p. 11-15.
- Abatal, A. , et al., Intelligent Interconnected Healthcare System: Integrating IoT and Big Data for Personalized Patient Care. International Journal of Online & Biomedical Engineering, 2024. 20(11).
- Bagesh Kumar, Y.V.S.R. , Rishik Gupta, Thakur Amrita Singh, Prakhar Shukla, Pratiksh Kumar, Smart healthcare system, in Explainable Artificial Intelligence for Biomedical and Healthcare Applications. 2024. p. 31-49.
- Maqbool, S. , et al. IoT based remote patient monitoring system. in 2020 International Conference on Decision Aid Sciences and Application (DASA). 2020. IEEE.
- Ramalakshmi, K. , et al., Enhancing Healthcare Through Remote Patient Monitoring Using Internet of Things, in Technologies for Sustainable Healthcare Development. 2024, IGI Global. p. 133-146.
- Singh, B.N., A. Singh, and K.A. Gautam, IoT-based Effective Wearable Healthcare Monitoring System for Remote Areas, in Smart Healthcare Systems. 1990, CRC Press. p. 85-104.
- Srinivasaiah, B. , Transformative Wearables: How AI and ML are Shaping Healthcare Innovations.
- Sheth, V. , et al., Schematized Study for Tackling COVID-19 with Machine Learning (ML), Artificial Intelligence (AI), and Internet of Things (IoT). Intelligent Pharmacy, 2024.
- Kavitha, V. , et al. A Comprehensive Survey of IoT Applications in Remote Patient Monitoring, Chronic Disease Management, and Smart Healthcare Infrastructure. in 2024 3rd International Conference on Sentiment Analysis and Deep Learning (ICSADL). 2024. IEEE.
- Suárez, Y.S., A. M. Alawi, and S.E.L. Ricardo, Hospital processes optimization based on artificial intelligence. LatIA, 2023. 1: p. 19-19.
- Faramarzi, S. , et al., Investigating the role of machine learning techniques in internet of things during the COVID-19 pandemic: A systematic review. Informatics in Medicine Unlocked, 2024: p. 101453.
- Jacob, L., K. Thomas, and S. Shukla, Potential Applications of AI and IoT Collaborative Framework for Health Care. The Role of AI, IoT and Blockchain in Mitigating the Impact of COVID-19, 2023: p. 69.
- Aware, M.S. , et al., Integrating AI, Machine Learning, and IoT Technologies for Enhanced Communication and Medical Applications, in Ensuring Security and End-to-End Visibility Through Blockchain and Digital Twins. 2024, IGI Global. p. 251-265.
- Maleki Varnosfaderani, S. and M. Forouzanfar, The role of AI in hospitals and clinics: transforming healthcare in the 21st century. Bioengineering, 2024. 11(4): p. 337.
- Olawade, D.B. , et al., Artificial intelligence in healthcare delivery: Prospects and pitfalls. Journal of Medicine, Surgery, and Public Health, 2024: p. 100108.
- Udegbe, F.C. , et al., The role of artificial intelligence in healthcare: A systematic review of applications and challenges. International Medical Science Research Journal, 2024. 4(4): p. 500-508.
- Thottempudi, P. and V. Kumar, The Role of IoT in Modern Healthcare: Innovations and Challenges in Pandemic Era, in Technologies for Sustainable Healthcare Development. 2024, IGI Global. p. 57-80.
- Ziadi, F., H. Fourati, and L.A. Saidane, AI and IoT Uses, Challenges and Opportunities for e-Health: a review. 2024 International Wireless Communications and Mobile Computing (IWCMC), 2024: p. 873-878.
- Shamshirband, S. , et al., A review on deep learning approaches in healthcare systems: Taxonomies, challenges, and open issues. Journal of Biomedical Informatics, 2021. 113: p. 103627.
- Ellahham, S. , Artificial intelligence: the future for diabetes care. The American journal of medicine, 2020. 133(8): p. 895-900.
- Rghioui, A. , et al. A smart architecture for diabetic patient monitoring using machine learning algorithms. in Healthcare. 2020. MDPI.
- WHO. Noncommunicable diseases. 2021; Available from: https://www.who.int/news-room/factsheets/ detail/noncommunicable-diseases.
- Sriram, R.D. and S.S.K. Reddy, Artificial intelligence and digital tools: future of diabetes care. Clinics in Geriatric Medicine, 2020. 36(3): p. 513-525.
- Vettoretti, M. , et al., Advanced diabetes management using artificial intelligence and continuous glucose monitoring sensors. Sensors, 2020. 20(14): p. 3870.
- Chan, K.S. , et al., Clinical validation of an artificial intelligence-enabled wound imaging mobile application in diabetic foot ulcers. International wound journal, 2022. 19(1): p. 114-124.
- Chowdhury, R.H. , Intelligent systems for healthcare diagnostics and treatment. World Journal of Advanced Research and Reviews, 2024. 23(1): p. 007-015.
- Shaheen, M.Y. , Applications of Artificial Intelligence (AI) in healthcare: A review. ScienceOpen Preprints, 2021.
- Gupta, P. and M.K. Pandey, Role of AI for Smart Health Diagnosis and Treatment, in Smart Medical Imaging for Diagnosis and Treatment Planning. 2024, Chapman and Hall/CRC. p. 23-45.
- Vasudevan, V., U. S. Mohan, and M.S. Gounder, AI-Powered Internet of Medical Things for Monitoring Elderly Adults in Independent Living Environments, in Smart Healthcare Systems. CRC Press. p. 289-303.
- Harshavardhanan, P., P. Suman, and S.S. Ghosh, IoT as Wearable Device in Smart Healthcare Systems: A New Paradigm, in Technologies for Sustainable Healthcare Development. 2024, IGI Global. p. 81-96.
- Manimegalai, D. , et al., AIoT-Powered Intelligent Remote Patient Activity Tracking and Comprehensive Vital Sign Analysis System for Enhanced Healthcare, in Technologies for Sustainable Healthcare Development. 2024, IGI Global. p. 147-173.
- He, W., Z. J. Zhang, and W. Li, Information technology solutions, challenges, and suggestions for tackling the COVID-19 pandemic. International journal of information management, 2021. 57: p. 102287.
- Barnawi, A. , et al., Artificial intelligence-enabled Internet of Things-based system for COVID-19 screening using aerial thermal imaging. Future Generation Computer Systems, 2021. 124: p. 119-132.
- De Boer, B. and O. Kudina, What is morally at stake when using algorithms to make medical diagnoses? Expanding the discussion beyond risks and harms. Theoretical Medicine and Bioethics, 2021. 42(5): p. 245-266.
- Zhu, Y. , et al., M $^ 3$ Fair: Mitigating Bias in Healthcare Data through Multi-Level and Multi-Sensitive-Attribute Reweighting Method. arXiv preprint. arXiv:2306.04118, 2023.
- HEckErmAN, D. , Healthcare delivery in developing countries: Challenges and potential solutions. F our T h P aradigm, 2009: p. 65.
- Mbangula, D.K. , Adopting of artificial intelligence and development in developing countries: perspective of economic transformation, in Handbook of Research on Connecting Philosophy, Media, and Development in Developing Countries. 2022, IGI Global. p. 276-288.
- Oak, M. , A review on barriers to implementing health informatics in developing countries. Journal of Health Informatics in developing countries, 2007. 1(1).
- Qadir, J. , et al., IEEE access special section editorial: health informatics for the developing world. IEEE Access, 2017. 5: p. 27818-27823.
- Rudd, J. and C. Igbrude, A global perspective on data powering responsible AI solutions in health applications. AI and Ethics, 2023: p. 1-11.
- Murdoch, B. , Privacy and artificial intelligence: challenges for protecting health information in a new era. BMC Medical Ethics, 2021. 22: p. 1-5.
- Rohringer, T.J., A. Budhkar, and F. Rudzicz, Privacy versus artificial intelligence in medicine. University of Toronto Medical Journal,[sl], 2019. 96(1): p. 51-53.
- Gerke, S., T. Minssen, and G. Cohen, Ethical and legal challenges of artificial intelligence-driven healthcare, in Artificial intelligence in healthcare. 2020, Elsevier. p. 295-336.
- Pasricha, S. , AI ethics in smart healthcare. IEEE Consumer Electronics Magazine, 2022. 12(4): p. 12-20.
- Page, M.J. , et al., The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. bmj, 2021. 372.
- ANDERSON III, E.V. , et al., Systems and methods for managing chronic disease using analyte and patient data. 2018, Google Patents.
- Mansour, M., M. S. Darweesh, and A. Soltan, Wearable devices for glucose monitoring: A review of state-of-the-art technologies and emerging trends. Alexandria Engineering Journal, 2024. 89: p. 224-243.
- Qureshi, M.R.A. , et al., Using Artificial Intelligence to Improve the Accuracy of a Wrist-Worn, Noninvasive Glucose Monitor: A Pilot Study. Journal of Diabetes Science and Technology, 2024: p. 19322968241252819.
- Tarumi, S. , et al., Leveraging artificial intelligence to improve chronic disease care: methods and application to pharmacotherapy decision support for type-2 diabetes mellitus. Methods of Information in Medicine, 2021. 60(S 01): p. e32-e43.
- Dadkhah, M. , et al., Use of internet of things for chronic disease management: an overview. Journal of Medical Signals & Sensors, 2021. 11(2): p. 138-157.
- Mahajan, S. and A. Birajdar. IoT based smart health monitoring system for chronic diseases. in 2019 IEEE Pune Section International Conference (PuneCon). 2019. IEEE.
- Nagarajan, V.D. , et al., Artificial intelligence in the diagnosis and management of arrhythmias. European heart journal, 2021. 42(38): p. 3904-3916.
- Siontis, K.C. , et al., Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nature Reviews Cardiology, 2021. 18(7): p. 465-478.
- Mishra, D., P. Singh, and S. Agarwal, AI-and IoT-based architecture in healthcare, in Transformation in Healthcare with Emerging Technologies. 2022, Chapman and Hall/CRC. p. 1-18.
- Ma, Y. , et al. Artificial intelligence chronic disease management system based on medical resource perception. in International Conference on Artificial Intelligence and Security. 2021. Springer.
- Shah, R. and A. Chircu, IoT and AI in healthcare: A systematic literature review. Issues in Information Systems, 2018. 19(3).
- Gupta, M. , et al. Real time interaction-based Healthcare monitoring during Medical Emergencies with Internet of Things. in 2022 2nd International Conference on Advance Computing and Innovative Technologies in Engineering (ICACITE). 2022. IEEE.
- Diraco, G., A. Leone, and P. Siciliano, Ai-based early change detection in smart living environments. Sensors, 2019. 19(16): p. 3549.
- Adhikary, T. , et al., The internet of things (iot) augmentation in healthcare: An application analytics. ICICCT 2019–System Reliability, Quality Control, Safety, Maintenance and Management: Applications to Electrical, Electronics and Computer Science and Engineering, 2020: p. 576-583.
- Rathee, G. , et al., ANN assisted-IoT enabled COVID-19 patient monitoring. Ieee Access, 2021. 9: p. 42483-42492.
- Rogers, R. , Internet of things-based smart healthcare systems, wireless connected devices, and body sensor networks in COVID-19 remote patient monitoring. American journal of medical research, 2021. 8(1): p. 71-80.
- Balica, R.-S. , Networked wearable devices, machine learning-based real-time data sensing and processing, and internet of medical things in COVID-19 diagnosis, prognosis, and treatment. American Journal of Medical Research, 2022. 9(1): p. 33-48.
- Ponnusamy, V. , et al., Smart healthcare technologies for massive internet of medical things, in Efficient Data Handling for Massive Internet of Medical Things: Healthcare Data Analytics. 2021, Springer. p. 71-101.
- Reddy, J.E.P. , et al. AI-IoT based healthcare prognosis interactive system. in 2020 IEEE International Conference for Innovation in Technology (INOCON). 2020. IEEE.
- Revathi, K. , et al., IoT Based Pulse Oximeter for Remote Health Assessment: Design, Challenges and Futuristic Scope. IJEER, 2022. 10(3): p. 557-563.
- Anjum, K., M. Sameer, and S. Kumar. AI enabled NLP based text to text medical Chatbot. in 2023 3rd International Conference on Innovative Practices in Technology and Management (ICIPTM). 2023. IEEE.
- Athota, L. , et al. Chatbot for healthcare system using artificial intelligence. in 2020 8th International conference on reliability, infocom technologies and optimization (trends and future directions)(ICRITO). 2020. IEEE.
- Ansari, M. , et al., AI-based diagnosis techniques for cardiac disease analysis and predictions, in Image Processing for Automated Diagnosis of Cardiac Diseases. 2021, Elsevier. p. 133-155.
- Erickson, B.J. , et al., Machine learning for medical imaging. radiographics, 2017. 37(2): p. 505-515.
- Hosny, A. , et al., Artificial intelligence in radiology. Nature Reviews Cancer, 2018. 18(8): p. 500-510.
- McBee, M.P. , et al., Deep learning in radiology. Academic radiology, 2018. 25(11): p. 1472-1480.
- Esteva, A. , et al., A guide to deep learning in healthcare. Nature medicine, 2019. 25(1): p. 24-29.
- Johnson, K.W. , et al., Artificial intelligence in cardiology. Journal of the American College of Cardiology, 2018. 71(23): p. 2668-2679.
- Rajkomar, A., J. Dean, and I. Kohane, Machine learning in medicine. New England Journal of Medicine, 2019. 380(14): p. 1347-1358.
- Topol, E.J. , High-performance medicine: the convergence of human and artificial intelligence. Nature medicine, 2019. 25(1): p. 44-56.
- Mathur, P. and M.L. Burns, Artificial intelligence in critical care. International anesthesiology clinics, 2019. 57(2): p. 89-102.
- Rahman, M.S. , et al., Artificial Intelligence-Based Algorithms and Healthcare Applications of Respiratory Inductance Plethysmography: A Systematic Review. Algorithms, 2024. 17(6): p. 261.
- Rghioui, A. and A. Oumnad, Internet of things: visions, technologies, and areas of application. Automation, Control and Intelligent Systems, 2017. 10(2): p. 83-91.
- Aceto, G., V. Persico, and A. Pescapé, The role of Information and Communication Technologies in healthcare: taxonomies, perspectives, and challenges. Journal of Network and Computer Applications, 2018. 107: p. 125-154.
- Desautels, T. , et al., Prediction of sepsis in the intensive care unit with minimal electronic health record data: a machine learning approach. JMIR medical informatics, 2016. 4(3): p. e5909.
- Topol, E. , Deep medicine: how artificial intelligence can make healthcare human again. 2019: Hachette UK.
- Wong, A.-K.I. , et al., Machine learning methods to predict acute respiratory failure and acute respiratory distress syndrome. Frontiers in big Data, 2020. 3: p. 579774.
- Kumar, M. , et al., Healthcare Internet of Things (H-IoT): Current trends, future prospects, applications, challenges, and security issues. Electronics, 2023. 12(9): p. 2050.
- Malik, N. , et al., A comprehensive review of blockchain applications in industrial Internet of Things and supply chain systems. Applied Stochastic Models in Business and Industry, 2021. 37(3): p. 391-412.
- Mansour, R.F. , et al., Artificial intelligence and internet of things enabled disease diagnosis model for smart healthcare systems. IEEE Access, 2021. 9: p. 45137-45146.
- Munavalli, J.R. , et al., Real-time capacity management and patient flow optimization in hospitals using AI methods. Artificial intelligence and Data mining in healthcare, 2021: p. 55-69.
- Rghioui, A. and A. Oumnad, Challenges and Opportunities of Internet of Things in Healthcare. International Journal of Electrical & Computer Engineering (2088-8708), 2018. 8(5).
- Chen, M. , et al., Disease prediction by machine learning over big data from healthcare communities. Ieee Access, 2017. 5: p. 8869-8879.
- Contreras, I. and J. Vehi, Artificial intelligence for diabetes management and decision support: literature review. Journal of medical Internet research, 2018. 20(5): p. e10775.
- Mohr, D.C., M. Zhang, and S.M. Schueller, Personal sensing: understanding mental health using ubiquitous sensors and machine learning. Annual review of clinical psychology, 2017. 13(1): p. 23-47.
- Haidar, A. , et al., Comparison of dual-hormone artificial pancreas, single-hormone artificial pancreas, and conventional insulin pump therapy for glycaemic control in patients with type 1 diabetes: an open-label randomised controlled crossover trial. The lancet Diabetes & endocrinology, 2015. 3(1): p. 17-26.
- Hickey, K.T. , et al., Precision health: Advancing symptom and self-management science. Nursing Outlook, 2019. 67(4): p. 462-475.
- Akduman, S. and K. Yilmaz, Examining the effectiveness of artificial intelligence applications in asthma and COPD outpatient support in terms of patient health and public cost: SWOT analysis. Medicine, 2024. 103(29): p. e38998.
- Margam, R. , SMART INHALERS: HARNESSING IOT FOR PRECISE ASTHMA MANAGEMENT. 2024.
- Alex, S.A. , et al. Intelligent Medication Compliance System for Patients Using IoT. in 2024 7th International Conference on Information and Computer Technologies (ICICT). 2024. IEEE.
- Stehlik, J. , et al., Continuous wearable monitoring analytics predict heart failure hospitalization: the LINK-HF multicenter study. Circulation: Heart Failure, 2020. 13(3): p. e006513.
- Rovin, B.H. , et al., KDIGO 2021 clinical practice guideline for the management of glomerular diseases. Kidney international, 2021. 100(4): p. S1-S276.
- Institute, P. The Cost of a Data Breach Report 2020. 2020; Available from: https://www.ibm.com/security/data-breach.
- Karunarathne, S.M., N. Saxena, and M.K. Khan, Security and privacy in IoT smart healthcare. IEEE Internet Computing, 2021. 25(4): p. 37-48.
- Commission, E. General Data Protection Regulation (GDPR). 2018; Available from: https://gdpr.eu/.
- Catalyst, N. , Healthcare big data and the promise of value-based care. NEJM Catalyst, 2018. 4(1).
- Obermeyer, Z. , et al., Dissecting racial bias in an algorithm used to manage the health of populations. Science, 2019. 366(6464): p. 447-453.
- Challen, R. , et al., Artificial intelligence, bias and clinical safety. BMJ quality & safety, 2019. 28(3): p. 231-237.
- FDA. AI/ML-Based Software as a Medical Device (SaMD): Action Plan. 2021; Available from: https://www.fda.gov/.
- Li, X. , et al., Digital health: tracking physiomes and activity using wearable biosensors reveals useful health-related information. PLoS biology, 2017. 15(1): p. e2001402.
- Collins, F.S. and H. Varmus, A new initiative on precision medicine. New England journal of medicine, 2015. 372(9): p. 793-795.
- Azar Abbas, N.A. , Digital Health Solutions and Machine Learning Algorithms: A New Era in Chronic Disease Management.
- Floridi, L. , et al., AI4People—an ethical framework for a good AI society: opportunities, risks, principles, and recommendations. Minds and machines, 2018. 28: p. 689-707.
Figure 1.
AI and IoT Integration in Diabetes Management.

Figure 2.
IoT-Enabled Healthcare for COVID-19.

Figure 3.
Challenges in Implementing AI and IoT in Healthcare.

Figure 4.
Systematic Review Methodology. As shown in Figure 4, the methodology follows a structured flow, beginning with an extensive literature search (Step 1), proceeding through the selection of relevant studies based on inclusion and exclusion criteria (Step 2), and concluding with the quantitative synthesis and meta-analysis (Step 4). Each step of the process ensures that only high-quality, peer-reviewed studies with measurable outcomes are included, and the final stage involves the validation of results through statistical tests.
Figure 4.
Systematic Review Methodology. As shown in Figure 4, the methodology follows a structured flow, beginning with an extensive literature search (Step 1), proceeding through the selection of relevant studies based on inclusion and exclusion criteria (Step 2), and concluding with the quantitative synthesis and meta-analysis (Step 4). Each step of the process ensures that only high-quality, peer-reviewed studies with measurable outcomes are included, and the final stage involves the validation of results through statistical tests.
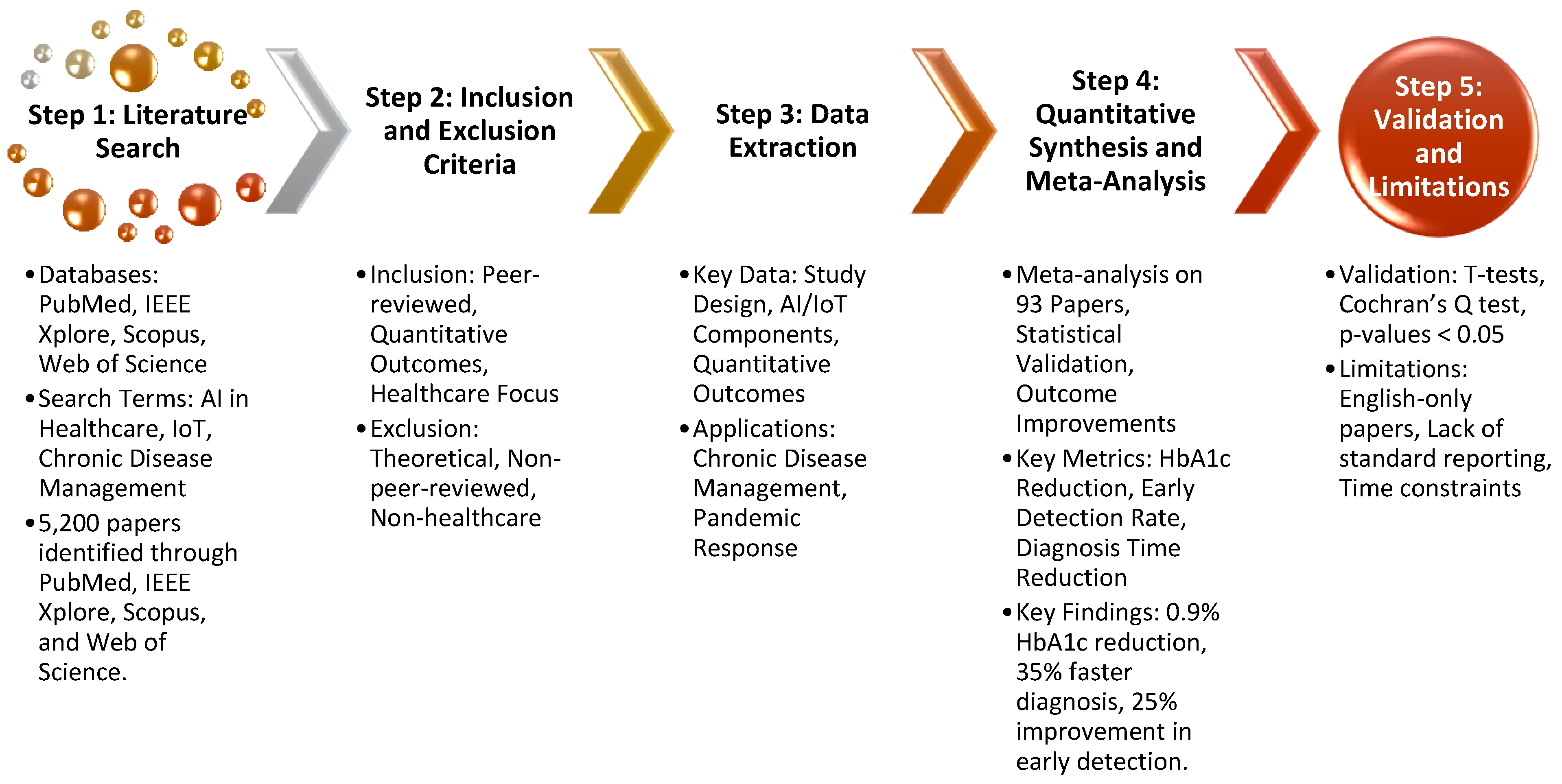
Figure 5.
AI and IoT Integration in Healthcare.

Figure 6.
AI and IoT Integration in Healthcare.

Figure 7.
AI-Enabled Continuous Glucose Monitoring (CGM) System for Diabetes Management.

Figure 8.
AI-Based Wearable ECG Monitor for Cardiovascular Disease.

Figure 9.
IoT-Connected Smart Inhaler for COPD Management.

Table 1.
Applications of AI and IoT in Healthcare.
| Application | AI Component | IoT Device | Impact | References |
|---|---|---|---|---|
| Diabetes Management | Machine learning algorithms for glucose prediction | Continuous glucose monitors (CGMs) | Improved glycemic control via AI-driven insulin regulation. | [5,31,32] |
| Cardiovascular Monitoring | AI-based predictive analytics for detecting arrhythmias | Wearable ECG monitors | Early detection and intervention, reducing mortality risk. | [32,33,34] |
| Hypertension Management | AI algorithms for blood pressure prediction | Blood pressure cuffs linked with IoT | Automated detection of anomalies, enabling timely interventions. | [5,35,36] |
| Elderly Care | AI-powered fall detection and health tracking | IoT sensors in homes, wearable devices | Reduced emergency hospital visits, immediate alerts to caregivers. | [33,34,36] |
Table 2.
Challenges in AI and IoT Adoption in Healthcare.
| Challenge | Description | Impact | References |
|---|---|---|---|
| Data Privacy and Security | Risks of data breaches and hacking of IoT devices. | Compromised patient confidentiality and trust in systems. | [46,47] |
| Algorithmic Bias | AI systems may yield inaccurate results for non-representative patient datasets. | Exacerbates healthcare inequalities, reduces diagnosis accuracy. | [48,49] |
| Cost of Implementation | High costs for AI and IoT deployment, particularly in low-resource settings. | Slows adoption, widens the technology gap between developed and developing regions. | [5] |
| Regulatory Issues | Lack of standardization and clear regulations for AI and IoT in healthcare. | Delays in implementation and inconsistent application across regions. | [48] |
Table 3.
Quantitative Results of AI and IoT Implementation in Chronic Disease Management.
| Metric | Number of Studies | Outcome | Statistical Significance |
|---|---|---|---|
| HbA1c reduction in diabetes | 40 | 0.9% average reduction in HbA1c levels | p ~ 0.01 |
| Reduction in hospital admissions | 40 | 15% fewer admissions due to better glucose control | p ~ 0.02 |
| Early detection of cardiovascular events | 25 | 25% improvement in detection rates using AI-based ECGs | p ~ 0.03 |
| Diagnosis time reduction (CVD) | 25 | 20-30% faster diagnosis with AI-enhanced tools | p ~ 0.04 |
Table 4.
Quantitative Results of AI and IoT in Pandemic Response.
| Metric | Number of Studies | Outcome | Statistical Significance |
|---|---|---|---|
| Diagnosis time reduction (COVID-19) | 28 | 35% faster diagnosis using AI-driven CT scan analysis | p ~ 0.003 |
| Reduction in hospital admissions | 28 | 20% fewer hospital admissions due to remote patient monitoring | p ~ 0.02 |
| Resource optimization | 28 | 25% increase in hospital resource utilization efficiency | p ~ 0.04 |
Table 5.
Overarching Quantitative Outcomes of AI and IoT in Healthcare.
| Key Metric | Outcome | Statistical Significance |
|---|---|---|
| Diagnostic accuracy improvement | 15-25% improvement across chronic disease and COVID-19 diagnostics | p < 0.05 |
| Healthcare cost reduction | 15-20% reduction in healthcare costs through IoT remote monitoring | p < 0.05 |
| Patient engagement and adherence | 20% increase in patient adherence to treatment plans using real-time monitoring | p < 0.05 |
Table 6.
Key Applications of AI and IoT in Chronic Disease Management.
| Application | Device/Technology | Outcome/Impact | References |
|---|---|---|---|
| Diabetes Management | Continuous Glucose Monitors (CGMs) | 0.9% reduction in HbA1c | [51-54]] |
| Cardiovascular Disease | AI-Enabled ECG Monitors | 25% improvement in arrhythmia detection | [55,56,57,58] |
| Respiratory Disease | Smart Inhalers and AI-Predictive Systems | Improved adherence and reduced exacerbations | [56,59] |
| Elderly Care | Wearable Fall Detectors, Smart Homes | Faster intervention, real-time monitoring | [59,60,61] |
Table 7.
AI and IoT Applications in Telemedicine and Remote Monitoring.
| Application | Device/Technology | Outcome | References |
|---|---|---|---|
| COVID-19 Monitoring | IoT-Enabled Pulse Oximeters | Reduced hospital admissions | [64,65,66] |
| Remote Consultations | Smart Thermometers, Digital Stethoscopes | Increased diagnostic accuracy by 15% | [66,67,68] |
| Virtual Health Assistants | AI-Powered NLP Systems | Enhanced patient interaction and triaging | [5,69] |
Table 8.
Summary of AI and IoT Applications in Chronic Disease Management.
| Disease | AI/IoT Technology | Outcome | References |
|---|---|---|---|
| Diabetes | AI-enhanced CGMs | 0.9% reduction in HbA1c, fewer hypoglycemic episodes | [96] |
| Cardiovascular Disease | AI-enabled wearable ECG monitors | 32% improvement in early arrhythmia detection, 93% accuracy, fewer hospitalizations | [97] |
| COPD | IoT-connected smart inhalers | 30-40% reduction in hospital admissions | [98,99] |
| COPD | IoT-connected smart inhalers | 15-20% improvement in medication adherence | [99,100] |
| Heart Failure | AI-powered remote monitoring system | 20% reduction in hospital readmissions | [101] |
| Chronic Kidney Disease | IoT-enabled sensors with AI predictive analytics | 30% slower disease progression | [102] |
Table 9.
Current State of AI-IoT Interoperability in Healthcare.
| Region | Adoption of FHIR Standards | % of Healthcare Systems with Legacy Infrastructure | Integration with EHRs (%) |
|---|---|---|---|
| North America | High | 40% | 70% |
| Europe | Moderate | 50% | 65% |
| Asia-Pacific | Low | 70% | 40% |
| Africa | Very Low | 85% | 20% |
Table 10.
Sources of Algorithmic Bias and Mitigation Strategies.
| Source of Bias | Impact on AI Performance | Mitigation Strategy |
|---|---|---|
| Underrepresentation of Minority Populations | Reduced accuracy in diverse patient groups | Inclusion of diverse training datasets |
| Homogeneous Clinical Trials | Inability to generalize predictions to real-world settings | Real-world evidence and continuous learning models |
| Socioeconomic Disparities | Biased access to care in underserved areas | Incorporation of social determinants of health into models |
Table 11.
Future Directions in Data Integration for AI-IoT Healthcare Systems.
| Data Type | Application in AI-IoT Systems | Potential Impact on COPD Management |
|---|---|---|
| Genomic Data | Predict disease susceptibility and personalize treatments | Precision medicine for COPD; tailored therapeutic interventions |
| Biomarkers | Monitor disease severity and predict exacerbations | Early detection of exacerbations and improved treatment outcomes |
| Environmental Data | Analyze external factors (e.g., air quality, weather) | Contextual insights for COPD management, minimizing environmental triggers |
Table 12.
Challenges and Solutions for Scaling AI-IoT Systems in Healthcare.
| Challenge | Proposed Solution | Long-Term Impact |
|---|---|---|
| High cost of IoT devices | Development of affordable, modular IoT devices | Broader access in low-resource settings |
| Lack of interoperability | Global adoption of open standards (e.g., FHIR) | Seamless data exchange between healthcare systems |
| Infrastructure limitations | Use of cloud-based AI analytics and decentralized computing | Scalable AI solutions for under-resourced facilities |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Copyright: This open access article is published under a Creative Commons CC BY 4.0 license, which permit the free download, distribution, and reuse, provided that the author and preprint are cited in any reuse.
From Fragmented to Integrated: Transforming Emergency Healthcare Delivery through Digital Twin Technology
Swapnil Morande
,
2023
Ambient Intelligence Based on IoT for Assisting People with Alzheimer’s Disease Through Context Histories
Savanna Denega Machado
et al.
,
2021
MDPI Initiatives
Important Links
© 2024 MDPI (Basel, Switzerland) unless otherwise stated








