Antigen antibody reactions
- 1. Dr Anuja Chandra By- Dr. Armaan SinghBy- Dr. Armaan Singh
- 2. Introduction Immunity Antibody Antigen Antigen antibody reaction and their applications Diagnostic tests of periodontal disease activity Conclusion References
- 3. ▻ The term immunity is derived from immunitas (Latin for exemption from civic duties or paying taxes) ▻ The term ‘immunity’ is defined as resistance exhibited by the host against any foreign antigen including microorganisms. ▻ The ability of an organism to resist a particular infection or toxin by the action of specific antibodies or sensitized white blood cells is called immunity.
- 5. An antigen is a substance which when introduced into a body evokes immune response to produce a specific antibody with which it reacts in an observable manner. It can be classified as- A. Complete Antigen B. Incomplete Antigen (Haptens) ‣ Complete antigens are substances which can induce antibody formation by themselves and can react specifically with these antibodies.
- 6. Haptens are substances unable to induce antibody formation on its own but can become immunogenic (capable of inducing antibodies) when covalently linked to proteins, called carrier proteins. They can be simple or complex. Proantigens are low molecular weight substances which do not induce antibody formation but can cause delayed hypersensitivity reaction. Epitope is the smallest unit of antigenicity. The combining site on the antibody molecule, corresponding to the epitope is called Paratope.
- 8. Foreignness Chemical nature Size Organ specificity Heterophile specificity Auto specificity Antigenic specificity Species specificity Susceptibility to tissue enzymes
- 9. These are molecules that can interact with antigen presenting cells and T lymphocytes in a non specific manner. These antigens do not involve the endocytic processing as required in typical antigen presentation. Viral proteins and staphylococcal enterotoxins are examples of superantigens.
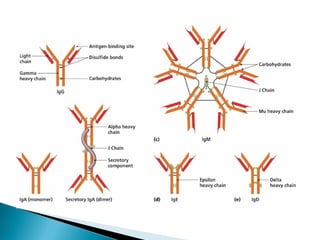
- 10. These are substances which are formed in the serum and tissue fluids in response to an antigen and react with that antigen specifically and in some observable manner. Secreted by plasma cells, occur in two physical forms, a soluble form that is secreted from the cell, and a membrane-bound form that is attached to the surface of a B cell and is referred to as the B cell receptor (BCR). The BCR is found only on the surface of B cells and facilitates the activation of these cells and their subsequent differentiation into either antibody factories called plasma cells or memory B cells that will survive in the body and remember that same antigen so the B cells can respond faster upon future exposure
- 13. Its uses are 1. In vivo Forms basis of immunity against infectious diseases May lead to tissue injury in hypersensitivity reactions and autoimmune diseases 2. In vitro For diagnosis of infections Helpful in epidemiological studies For identification of enzymes Detection and quantitation of antigens or antibodies
- 14. Reaction is specific, an antigen combines only with its homologous antibody and vice versa. However cross reactions may occur due to antigenic similarity. Entire molecules of antigen and antibody react and not the fragments. Only the surface antigens participate in the antigen antibody reaction. The reaction is firm but reversible. The firmness of combination depends on the affinity and avidity.
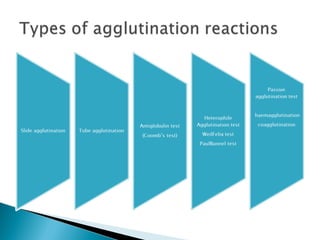
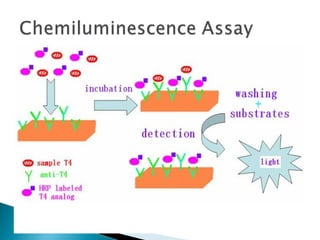
- 15. Precipitation reactions Agglutination Complement fixation test Neutralisation test Opsonisation Immunofluorescence Radioimmunoassay Enzyme linked immunosorbent assay Chemiluminescence assay Immunoelectronmicroscopic tests Immunoblotting
- 16. When a soluble antigen reacts with its antibody in the presence of electrolytes at an optimal temperature and pH, antigen antibody complex forms an insoluble precipitate that usually sediments at the bottom of the tube and it is called precipitation. Precipitation may occur in liquid media or in gels such as agar, agarose or polyacrylamide gels When instead of sedimenting, the precipitate is suspended as floccules the reaction is called flocculation
- 18. Identification of bacteria.eg Lancefield grouping of streptococcus Detection of antibody for diagnostic purposes.eg VDRL in syphilis Forensic application in identification of human blood and seminal stains Testing for food adulterants To standardise toxins and antitoxins
- 20. It is an antigen antibody reaction in which a particulate antigen combines with its antibody in presence of electrolytes at an optimal temperature and pH resulting in visible clumping of particles. Lattice formation hypothesis holds good for agglutination also. Occasionally incomplete antibodies (eg anti Rh and anti Brucella) are formed that combine with the antigen but do not cause agglutination. They act as “blocking antibodies” inhibiting the agglutination by the complete antibody added subsequently.
- 22. Principle The antigen antibody complexes have ability to ‘fix’ complement. This reaction has no visible effect. To detect fixation of a complement, an indicator system consisting of sheep erythrocytes coated with amboceptor ( rabbit antibody to sheep erythrocytes) is used.
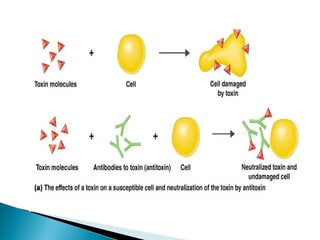
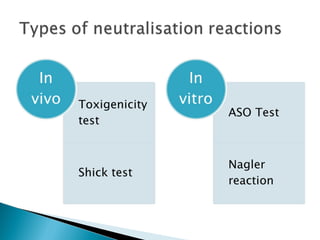
- 24. Bacterial exotoxins are capable of producing neutralising antibodies (antitoxins) which play a role in protection against diseases such as diphtheria and tetanus. The toxicity of bacterial endotoxins is not neautralised by antisera.
- 27. It is a process by which a particulate antigen becomes more susceptible to phagocytosis. Opsonic index is defined as ratio of phagocytic activity of the patient’s blood for a given bacterium to that of a normal individual. Phagocytic index is the average number of phagocytosed bacteria per polymorphonuclear leukocytes from stained blood films. Phagocytic index denotes the phagocytic activity of blood and thus helps in measuring opsonic index.
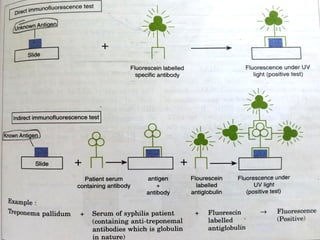
- 29. Fluorescence is the property of certain dyes which absorb rays of one particular wavelength(ultraviolet light) and emit rays with a different wavelength(visible light). Most commonly used dyes are 1.fluorescin isothiocyanate 2.lissamine rhodamine Two types are Direct and Indirect.
- 30. Specimen (Positive for antigen) + labelled antibodies ▼ Flurescence observed ▼ antigen is present in the specimen
- 31. It is a sensitive method to diagnose rabies by detection of rabies virus antigen in brain smears. It is commonly employed for detection of bacteria,viruses or other antigens in blood, CSF,urine,faeces,tissues and other specimens. Note – A separate specific fluorescent labelled antibody has to be prepared against each antigen to be tested.
- 32. Unlike direct method, antigen is known in this method. Lets have a look at the flowchart for clear understanding.
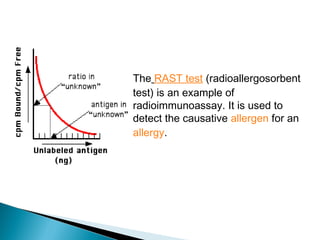
- 34. Berson and Yallow(1959) first described radioimmunoassay and since then it has been utilised for quantitation of hormones, drugs, hepatitis B surface antigen, IgE and viral antigens. This test can detect antigens upto picogram quantities. It is based on competition for a fixed amounts of specific antibody between a known radiolabelled antigen and an unknown unlabelled test antigen.
- 36. The RAST test (radioallergosorbent test) is an example of radioimmunoassay. It is used to detect the causative allergen for an allergy.
- 37. Advantages are- Highly sensitive Can be used for detection of small quantities Quantification possible Disadvantages are – Expensive Requires isotopes
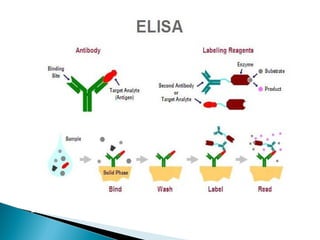
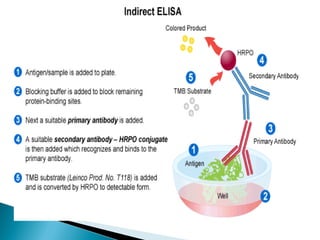
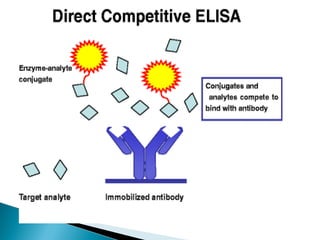
- 38. Enzyme Linked Immunosorbent Assay is as sensitive as radioimmunoassay. Requires only microlitre quantities of test reagents The enzyme acts on substrate to produce a color in a positive test. It can be used for detection of antigen or antibody Types are Sandwich, Indirect, Competitive or Cassette Elisa
- 44. Detection of HIV Antibodies in serum Detection of mycobacterial antibodies in tuberculosis Detection of Rotavirus in faeces Detection of Hepatitis B markers in serum Detection of enterotoxin of E.coli in faeces
- 46. Immunoferritin tests Immunoelectron microscopy Immunoenzyme tests Immunoblotting
- 47. Ferritin (electron dense substance) conjugated antibody is used to react with an antigen.This antigen antibody reaction can be visualised under microscope Used in identification of Legionella pnemophila
- 48. Viral particles are mixed with specific antisera and are observed under electron microscope. These are seen as clumps. Used in detection of Hepatitis A virus
- 49. Tissue sections are treated with peroxidase labelled antisera to detect corresponding antigen. The peroxidase bound to antigen is visualised under electron microscope.
- 50. In immunoblots, antibodies can detect proteins in mixtures.The mixture of proteins is electrophoretically separated in a gel. The separated proteins are transferred from gel to nitrocellulose paper. These nitrocellulose paper strips are reacted with test sera and subsequently with enzyme conjugated anti human immunoglobulin.
- 52. This test has been widely used to confirm the ELISA positive HIV antibody cases. The above procedure may also be applied to analyse DNA or RNA. When DNA is transferred on nitrocellulose strips from gel, this test is referred to as Southern Blot test. Similarily, if RNA is transferred it is named as Northern Blot test.
- 53. Potential biomarkers of the disease activity would need to be involved in the disease process in some way and therefore need to undergo extensive and careful basic research investigation before undergoing clinical evaluation. Only when the source,precise nature and the role of potential marker are known and understood can clinical evaluation be meaningful.
- 54. Potential sources from which markers can be obtained are- 1.blood or serum 2.saliva 3.subgingival plaque sample 4.gingival crevicular fluid
- 55. 1) Bacteria and their product 2) Inflammatory and immune products 3) Hydrolytic enzymes of tissue origin and those released from dead cells 4) Connective tissue degradation products 5) Products of bone resorption
- 56. Despite the complex interaction that exists between bacteria and host, a number of possible pathogens have been selected on the basis of their association with disease progression, animal pathogenicity and their possesion of virulence factors which could damage the tissues(Genco et al 1988, Listgarten 1992, Socransky and Haffajee 1992).
- 57. Porphyromonas gingivalis Prevotella intermedia Bacteroides forsythus Actinobacillus actinomycetamcomitans Capnocytophaga ochracea Eikenella corrodens Campylobacter recta Fusobacterium nucleatum Treponema denticola
- 58. There is no evidence for any one specific pathogen in chronic periodontitis and therefore it may be considered as a non specific bacterial disease (Theilade 1986). The bacteria listed here tend to be present in higher numbers at active disease sites (Socransky and Haffajee 1992). Bacterial species numbers may be determined in variety of ways (Listgarten 1992) and these include the following –
- 59. 1.Dark ground or Phase contrast microscopy 2.Culture techniques 3.Immunological assays 4. DNA probes 5. BANA assays
- 60. They use either paper points or curette bacterial sampling from pocket and include the following- Evalusite (Kodak) This utilizes ELISA’s using antibody against P.gingivalis, P intermedia, A. actinomycetemcomitans. This reaction is carried out in simple chairside kit. Subgingival plaque samples are reacted with the antibodies and detection substrate in a multiwell reaction dishes.
- 61. Omnigene and BTD(Bio technical diagnostics) These are DNA probe systems for a number of subgingival bacteria. A paper point sample of subgingival plaque is placed in a container and sent to company for assay. Probes are available for A. actinomycetemcomitans, P.gingivalis, P intermedia, E.corrodens, F.nucleatum,C. Recta and T.denticola
- 62. Perioscan (Oral B Laboratories) This is a chairside test kit system which utilises BANA Test for bacterial trypsin like proteases. They are mainly produced by P.gingivalis and in lesser amounts by B.forsythus and T.denticola. A subgingival plaque sample is reacted in the kit with the substrate linked to a color detection system.
- 63. Diamond Probe/Perio 2000 system Combines feature of periodontal probe with detection of volatile sulphur compounds in periodontal pocket.
- 64. Prototek Given by Cox et al in1990, this can be used to detect bacterial proteases arg-gingipain/gingivain and DPP in GCF. This is not commercially available yet.
- 65. Predictive of disease activity Simple Results available in short time Visual result
- 66. Polymicrobial nature of the disease Most are not predictive of the disease activity Site Can only detect bacteria we look for Special laboratory required Cost
- 67. Those of possible relevance to periodontal pathology are- Immune response Antibody Total IgG and IgG subgroups Complement Inflammatory mediators Arachidonic acid derivatives Cytokines
- 68. Porphyromonas gingivalis has been implicated as major periodontal pathogen and it has been reported that a positive co relation exists between IgG levels to P.gingivalis and severity of periodontal disease(Gmur et al 1986;Lamster et al 1998;Blackburn 1992) Furthermore elevation in P.gingivalis specific IgG2, IgG1 and IgG4 in rapidly progressing periodontitis and adult periodontitis have been reported.(Kinane et al 1999) Complement proteins are present in GCF from sites with inflammation and the split fragments C3 and Factor B have been detected during gingivitis(Patters et al 1989). However, none of these factors have been associated with disease activity.
- 69. Periotemp It has been developed to measure small changes in sublingual and subgingival temperatures and positive cross sectional comparision with clinical parameters have been found. Increased subgingival temperature has been positively corelated with increased pocket depths, decreased attachment levels, clinical parameters of gingival inflammation, higher proportions of putative periodontal pathogens and gingival crevicular fluid enzymes( Dinsdale et al 1997, Haffajee et al 1992, Wolff et al 1997)
- 70. Although GCF PGE2 has considerable potential as a screening test for periodontal activity, no commercial efforts are currently underway to develop one. Cytokines are also assayed using ELISA techniques which could be developed into chairside kits. However at present the predictive ability of these markers is still in doubt.
- 71. Only GCF PGE2 has been shown to be predictive of disease activity in longitudinal studies. ELISA techniques can be used to detect cytokines and PGE2 which could be developed into chairside kits which are simple to use. ELISA can be read after short time. They can be shown to the patient and related to the tooth site.
- 72. The choice of most appropriate biomarker may still be difficult at present state of knowledge. There is difficulty in determining the sites to sample and when to sample them. Cost
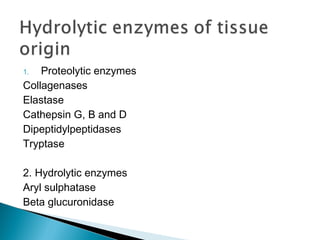
- 73. 1. Proteolytic enzymes Collagenases Elastase Cathepsin G, B and D Dipeptidylpeptidases Tryptase 2. Hydrolytic enzymes Aryl sulphatase Beta glucuronidase
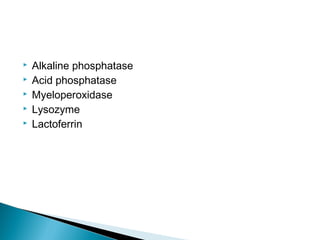
- 74. Alkaline phosphatase Acid phosphatase Myeloperoxidase Lysozyme Lactoferrin
- 75. Collagenase 2(MMP 8), collagenase 1(MMP 1) and collagenase 3(MMP 13) activity are present in gingival tissue,saliva and gcf and can be assayed biochemically with collagen substrates(Sorsa et al 1990) or with ELISA technique (Ingman et al 1996, Matsuki et al 1996). Elastase in gingival tissues is produced by PMN’s and is held in an inactive form probably bound with an inhibitor.It is inhibited by secretory leukocyte protease inhibitor (SLPI) and skin antileukoproteinase (SKALP) (Cox et al 2001)
- 76. In humans, GCF tryptase activity corelates with clinical parameters of disease severity including probing attachment and bone lossand significantly reduces following periodontal treatment (Eley and Cox 1992). Both tissue DPP 2 AND 4 corelate with clinical parameters of disease severity and significantly reduce following periodontal treatment (Cox and Eley 1992)
- 77. Periocheck These system detects presence of neutral proteinases such as collagenases in GCF. A paper strip used to obtain GCF sample is placed in contact with collagen gel to which a blue dye has been covalently bonded. It is then incubated at 43 degrees. Intensity α amount of enzyme present in the sample
- 78. Prognostik (Dentsply) This system detects presence of serine proteases, elastases in GCF samples Intensity of fluorescence α amount of enzyme in the sample
- 79. β glucuronidase It is a diagnostic kit that uses a histochemical substrate for the enzymes coupled to a color detection system which is releasedif the enzyme attacks the substrate( Lamster et al 1988, 1991, 1994) Cysteine and serine proteinases Developed in conjugation in researchers from Prototek has following advantages over it-
- 80. Can be modified to detect number of different proteinases including DPP 2 and 4, tryptase etc. GCF sample is collected on a normal paper strip and therefore leaving group are not introduced into the gingival crevice unlike Dentsply Color detection system for this method is more convenient foe the use in dental practice as it requires no special apparatus.
- 81. Simple Can be read after short time Can be shown to patient and related to tooth site
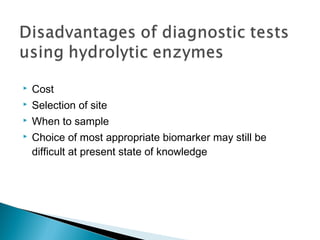
- 82. Cost Selection of site When to sample Choice of most appropriate biomarker may still be difficult at present state of knowledge
- 83. Since cell death is an essential component of periodontal tissue destruction they should be released during this process and should pass with the inflammatory exudate into GCF. Aspartate amino transferase (AST) Lactate dehydrogenase (LDH)
- 84. Periogard AST in GCF test kit
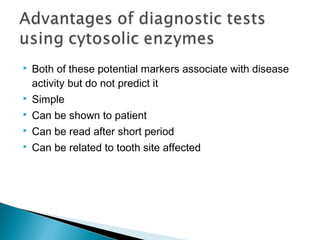
- 85. Both of these potential markers associate with disease activity but do not predict it Simple Can be shown to patient Can be read after short period Can be related to tooth site affected
- 86. Cost Selection of site When to sample Choice of most appropriate biomarker may still be difficult at present state of knowledge
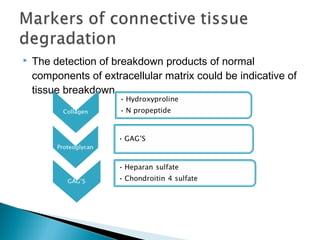
- 87. The detection of breakdown products of normal components of extracellular matrix could be indicative of tissue breakdown.
- 88. Most complex and expensive Long collection times Not suitable for chairside
- 89. Possible markers of bone resorption and hence periodontal disease activity are- Osteonectin Bone phosphoprotein (N-propeptide) Osteocalcin Telopeptides of type 1 collagen Collagen 1 Proteoglycans
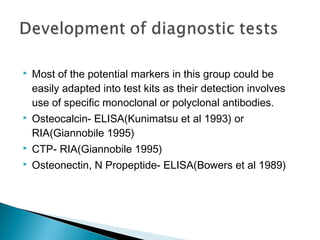
- 90. Most of the potential markers in this group could be easily adapted into test kits as their detection involves use of specific monoclonal or polyclonal antibodies. Osteocalcin- ELISA(Kunimatsu et al 1993) or RIA(Giannobile 1995) CTP- RIA(Giannobile 1995) Osteonectin, N Propeptide- ELISA(Bowers et al 1989)
- 91. Some of these potential biomarkers associate with the disease but do not predict it Can be read after relatively short periods Can be shown to the patient
- 92. Choice of most appropriate biomarker is difficult at the present state of knowledge Difficulty in determining sites to sample and when to sample them Cost
- 93. Therefore we see the application of antigen antibody reactions in development of variety of diagnostic tests. Only markers with credentials should be used in clinical practice for the reasons listed below- 1. To prevent destructive disease 2. To prevent progression of the disease 3. To identify high risk patients 4. To target treatment to specific sites 5. To monitor the effects of periodontal treatment
- 94. Thank you !! Thank you
Editor's Notes
- #7: Simple is univalent complex is polyvalent. pptn occurs when antigen as two or more antibody combining sites.
- #17: Flocculation VDRL Syphilis
- #29: Antibody dependent cellular cytotoxicity
- #35: Nobel prize 1977 yallow :10 to power minus 12
- #77: DIPEPTIDYLPEPTIDASE – ALL DPP ACTIVE AT ACID ph except DPP 4 ALKALINE ph present in gingival tissue and GCF
- #79: 7 amino trifluromethylcoumarin
- #88: METHOD OF ISOLATION IS HPLC high pressure liquid chromatography