Lateral medullary syndrome {Wallenberg Syndrome}
- 1. Lateral Medullary Syndrome Wallenberg syndrome Prof. Ahmed M Badheeb, MD. Professor Of Oncology /Internal Med.
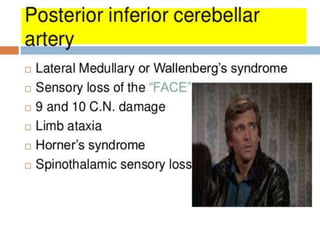
- 2. Wallenberg syndrome • or lateral medullary infarction, is associated with the acute onset of vertigo and disequilibrium. • The blood supply to the lateral medulla is the posterior inferior cerebellar artery.
- 3. PATHOPHYSIOLOGY • Most patients with Wallenberg's syndrome have an occlusion of the ipsilateral vertebral artery that gives rise to the posterior inferior cerebellar artery .
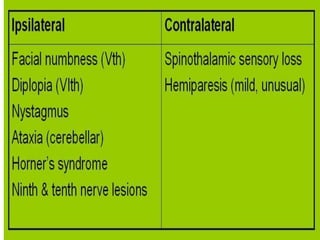
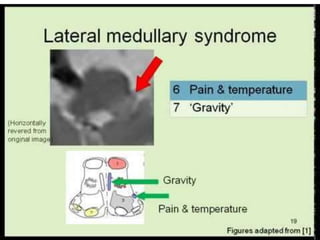
- 4. The clinical presentation, • Vertigo • abnormal eye movements • an ipsilateral Horner syndrome • ipsilateral limb ataxia • dissociated sensory loss (loss of pain and temperature sensation on the ipsilateral face and contralateral trunk with preserved vibration and position sense). • Hoarseness and dysphagia are often present.
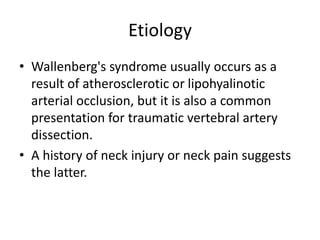
- 5. Etiology • Wallenberg's syndrome usually occurs as a result of atherosclerotic or lipohyalinotic arterial occlusion, but it is also a common presentation for traumatic vertebral artery dissection. • A history of neck injury or neck pain suggests the latter.
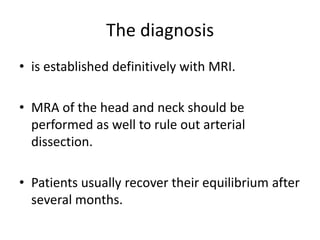
- 6. The diagnosis • is established definitively with MRI. • MRA of the head and neck should be performed as well to rule out arterial dissection. • Patients usually recover their equilibrium after several months.