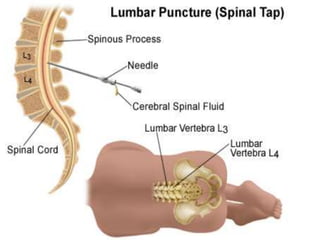
Lumbar puncture
- 2. • A lumbar puncture (or LP, and colloquially known as a spinal tap) is a diagnostic procedure that is performed in order to collect a sample of cerebrospinal fluid (CSF)
- 3. INDICATIONS Lumbar puncture should be performed for the following indications: • Suspicion of meningitis • Suspicion of subarachnoid hemorrhage (SAH) • Suspicion of central nervous system (CNS) diseases such as Guillain-Barré syndrome and carcinomatous meningitis • Therapeutic relief of pseudotumor cerebri
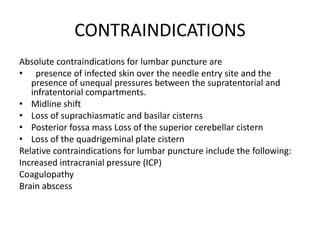
- 4. CONTRAINDICATIONS Absolute contraindications for lumbar puncture are • presence of infected skin over the needle entry site and the presence of unequal pressures between the supratentorial and infratentorial compartments. • Midline shift • Loss of suprachiasmatic and basilar cisterns • Posterior fossa mass Loss of the superior cerebellar cistern • Loss of the quadrigeminal plate cistern Relative contraindications for lumbar puncture include the following: Increased intracranial pressure (ICP) Coagulopathy Brain abscess
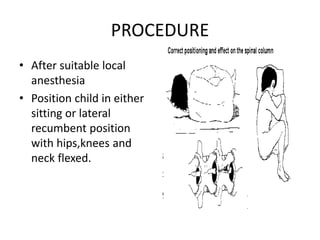
- 5. PROCEDURE • After suitable local anesthesia • Position child in either sitting or lateral recumbent position with hips,knees and neck flexed.
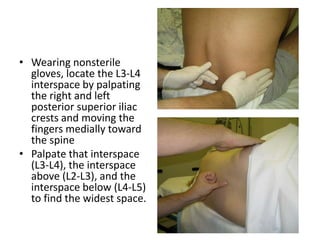
- 6. • Wearing nonsterile gloves, locate the L3-L4 interspace by palpating the right and left posterior superior iliac crests and moving the fingers medially toward the spine • Palpate that interspace (L3-L4), the interspace above (L2-L3), and the interspace below (L4-L5) to find the widest space.
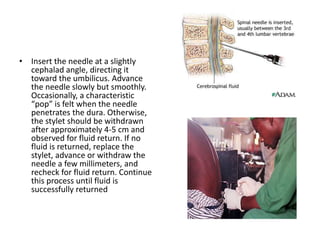
- 8. • Insert the needle at a slightly cephalad angle, directing it toward the umbilicus. Advance the needle slowly but smoothly. Occasionally, a characteristic “pop” is felt when the needle penetrates the dura. Otherwise, the stylet should be withdrawn after approximately 4-5 cm and observed for fluid return. If no fluid is returned, replace the stylet, advance or withdraw the needle a few millimeters, and recheck for fluid return. Continue this process until fluid is successfully returned
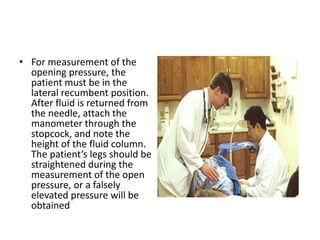
- 9. • For measurement of the opening pressure, the patient must be in the lateral recumbent position. After fluid is returned from the needle, attach the manometer through the stopcock, and note the height of the fluid column. The patient’s legs should be straightened during the measurement of the open pressure, or a falsely elevated pressure will be obtained
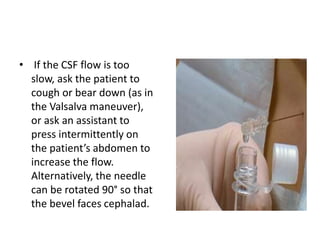
- 10. • If the CSF flow is too slow, ask the patient to cough or bear down (as in the Valsalva maneuver), or ask an assistant to press intermittently on the patient’s abdomen to increase the flow. Alternatively, the needle can be rotated 90° so that the bevel faces cephalad.
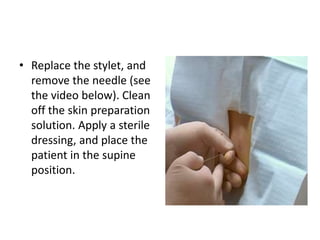
- 11. • Replace the stylet, and remove the needle (see the video below). Clean off the skin preparation solution. Apply a sterile dressing, and place the patient in the supine position.
- 12. COMPLICATIONS • Local pain • Infection • Bleeding • Spinal Fluid Leak • Hematoma • Spinal Headache/Post-tap headache • Acquired epidermal spinal cord tumor (caused by implantation of epidermal material into spinal canal if no stylet is used on skin entry)